Nurse education consists of the theoretical and practical training provided to nurses with the purpose to prepare them for their duties as nursing care professionals. This education is provided to student nurses by experienced nurses and other medical professionals who have qualified or experienced for educational tasks, traditionally in a type of professional school known as a nursing school. Most countries offer nurse education courses that can be relevant to general nursing or to specialized areas including mental health nursing, pediatric nursing and post-operatory nursing. Courses leading to autonomous registration as a nurse typically last four years. Nurse education also provides post-qualification courses in specialist subjects within nursing.
Team nursing is a system of integrated care that was developed in 1950s directed by Eleanor Lambertson at Teachers College, Columbia University in New York, NY. Because the functional method received criticism, a new system of nursing was devised to improve patient satisfaction. “Care through others” became the hallmark of team nursing. It was developed in an effort to decrease the problems associated with the functional model of nursing care. Many people felt that, despite a continued shortage of professional nursing staff, a patient care delivery model had to be developed that reduced the fragmented care that accompanies functional nursing.

Matron is the job title of a very senior or the chief nurse in several countries, including the United Kingdom, and other Commonwealth countries and former colonies.
Nursing in the United Kingdom has a long history. The current form of nursing is often considered as beginning with Florence Nightingale who pioneered modern nursing. Nightingale initiated formal schools of nursing in the United Kingdom in the late 19th and early 20th centuries. The role and perception of nursing has dramatically changed from that of a handmaiden to the doctor to professionals in their own right. There are over 700,000 nurses in the United Kingdom and they work in a variety of settings, such as hospitals, health centres, nursing homes, hospices, communities, military, prisons, and academia, with most working for the National Health Service (NHS). Nurses work across all demographics and requirements of the public: adults, children, mental health, and learning disability. Nurses work in a range of specialties from the broad areas of medicine, surgery, theatres, and investigative sciences such as imaging. Nurses also work in large areas of sub-specialities such as respiratory, diabetes, cancer, neurology, infectious diseases, liver, research, cardiac, women's health, sexual health, emergency and acute care, gastrointestinal, infection prevention and control, neuroscience, ophthalmic, pain and palliative, and rheumatology. Nurses often work in multi-disciplinary teams but increasingly are found working independently.
Primary nursing is a system of nursing care delivery that emphasizes continuity of care and responsibility acceptance by having one registered nurse (RN), often teamed with a licensed practical nurse (LPN) and/or nursing assistant (NA), who together provide complete care for a group of patients throughout their stay in a hospital unit or department. While the patient is on the nurses' unit, the primary nurse accepts responsibility for administering some and coordinating all aspects of the patient's nursing care, with the support of other members of the nursing staff. This results in the nurse having greater insight into the patient's condition, both medical and emotional.

Queen Alexandra's Royal Naval Nursing Service (QARNNS) is the nursing branch of the British Royal Navy. The Service unit works alongside the Royal Navy Medical Branch.
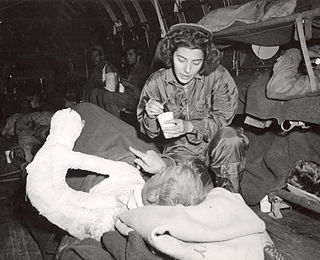
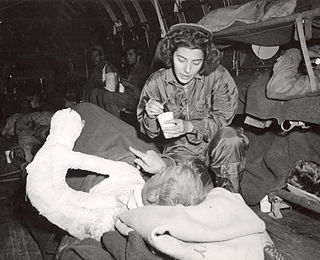
A flight nurse is a registered nurse who specialises in the field of providing comprehensive pre-hospital, emergency critical care, and hospital care to a vast scope of patients. The care of these patients is generally during aeromedical evacuation or rescue operations aboard helicopters, propeller aircraft or jet aircraft. On board a rescue aircraft you would find a flight nurse accompanied by flight medics and respiratory practitioners, as well as the option of a flight physician for comprehensive emergency and critical transport teams. The inclusion of a flight physician is more commonly seen in pediatric and neonatal transport teams. A critical care flight nurse must be able to deal with all age groups with broad critical emergencies. With no physicians on site the nurses scope of practice is expanded. The critical care experience is transferred over to a flight nurse with impacting factors such as altitude and changes in pressure, gravitational forces, and weather. Some patients may experience exacerbation because of factors related to the cabin environment including hypoxia, limited mobility, gas expansion, and risk of injury related to turbulence and resources with definitive care are limited. Aeromedical evacuation crews coordinate with other organizations to plan for the safe and timely care and evacuation of patients. Crews must be prepared for patients with trauma and mental health illnesses.

Nursing is a profession within the healthcare sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses can be differentiated from other healthcare providers by their approach to patient care, training, and scope of practice. Nurses practice in many specialties with differing levels of prescription authority. Nurses comprise the largest component of most healthcare environments; but there is evidence of international shortages of qualified nurses. Nurses collaborate with other healthcare providers such as physicians, nurse practitioners, physical therapists, and psychologists. There is a distinction between nurses and nurse practitioners; in the U.S., the latter are nurses with a graduate degree in advanced practice nursing, and are permitted to prescribe medications unlike the former. They practice independently in a variety of settings in more than half of the United States. Since the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles are changing.

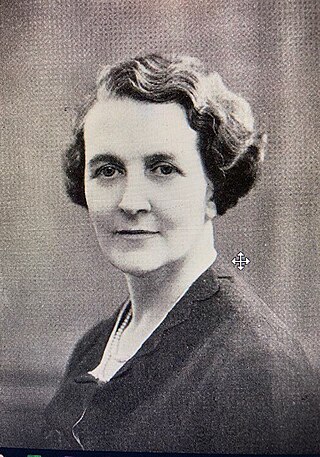
Eva Charlotte Ellis Luckes was Matron of The London Hospital from 1880 to 1919.
Caroline Keer, was a British military nurse and nursing administrator, who served in Natal during the Second Boer War.
Occupational health nursing is a specialty nursing practice that provides for and delivers health and safety programs and services to workers, worker populations, and community groups. The practice focuses on promotion, maintenance and restoration of health, prevention of illness and injury, and protection from work‐related and environmental hazards. Occupational health nurses (OHNs) aim to combine knowledge of health and business to balance safe and healthful work environments and a "healthy" bottom line.
A healthcare technician is a health professional that provides care to patients. Healthcare technician's primary position is to assist medical staff complete tasks around their assigned unit or clinic's and accommodate patient needs. Healthcare technicians are typically found in specialty clinics, intensive care, emergency departments, or laboratory collection facilities. Technicians will perform basic cardiology reports such as, electrocardiograms and will have basic understanding of bodily function. The technician is an integral member of the unit-based healthcare team, they contribute to the continuity of care by decreasing fragmentation through decentralization of selected diagnostic and therapeutic treatment modalities.

The history of nursing in the United States focuses on the professionalization of Nursing in the United States since the Civil War.
Marie Schuber Manthey is an American nurse, author, and entrepreneur. She is recognized as one of the originators of Primary Nursing, an innovative system of nursing care delivery.
Community nursing is nursing care delivered outside acute hospitals, for example in the home, within General Practice facilities, in community hospitals, in police custody, at a school or in a care home. In the UK, a community nurse needs a degree approved by the Nursing and Midwifery Council, as well as 1–2 years’ experience as a qualified Adult Nurse.
Rosalie Dreyer was a Swiss-born naturalised British nurse and administrator. Immigrating to England at the age of eighteen, she trained as a nurse in London and worked her way through the ranks to become matron, principal matron and chief matron-in-charge of the Nursing Service of the London County Council. At this time, nursing was making a shift from a voluntary service to a profession and Dreyer was involved as a pioneer in the development of Britain's public-funded nursing service.
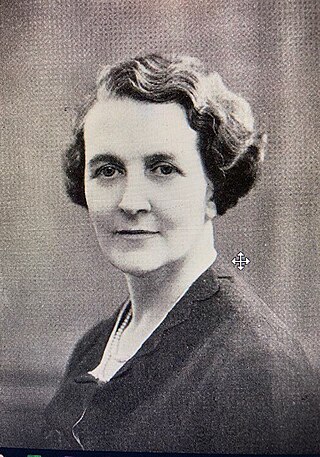
Dorothy Bannon, CBE was a pioneering British nurse who as Chief Matron-in-Charge of the Hospital and School Nursing Service of the London County Council. She was instrumental in the development of Britain's public-funded nursing service.
Nursing educational programs in Iran are similar to the nursing educational programs in other countries in many aspects. Holding a secondary school diploma and passing the entrance exam is necessary for the admission. The entrance exams to governmental universities and Azad University are held separately. The duration of the associate degree course for operating room and anesthesia is two years, a bachelor's degree in nursing is four years, a master's degree in nursing is two to two and a half years, and a doctorate degree in nursing is four to five years.

Ethel Tracy Richardson (1877–1942) was an Australian nursing sister, army matron-in-chief, and honorary major who served during the First World War. She was the first person to become Matron-in-chief on the staff of the director general of medical services at Army Headquarters, Melbourne.
The Salmon Report (1966) or the Salmon Report on Senior Nursing Staff Structure was the report of a committee established to bring standardisation in structure and pay for senior hospital nurses in England and Scotland. The report recommended changes to how nurses jobs were categorised in hospitals and management training for nurses.
Nurse Manager Core Competencies: A Proposal in the Spanish Health System. International Journal of Environmental Research and Public Health. 2020; 17(9):3173. https://doi.org/10.3390/ijerph17093173