Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. The term includes work done in providing primary care, secondary care, and tertiary care, as well as in public health.
Palliative care is an interdisciplinary medical caregiving approach aimed at optimizing quality of life and mitigating suffering among people with serious, complex, and often terminal illnesses. Within the published literature, many definitions of palliative care exist. The World Health Organization (WHO) describes palliative care as "an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain, illnesses including other problems whether physical, psychosocial, and spiritual". In the past, palliative care was a disease specific approach, but today the WHO takes a broader patient-centered approach that suggests that the principles of palliative care should be applied as early as possible to any chronic and ultimately fatal illness. This shift was important because if a disease-oriented approach is followed, the needs and preferences of the patient are not fully met and aspects of care, such as pain, quality of life, and social support, as well as spiritual and emotional needs, fail to be addressed. Rather, a patient-centered model prioritizes relief of suffering and tailors care to increase the quality of life for terminally ill patients.

The healthcare industry is an aggregation and integration of sectors within the economic system that provides goods and services to treat patients with curative, preventive, rehabilitative, and palliative care. It encompasses the creation and commercialization of products and services conducive to the preservation and restoration of well-being. The contemporary healthcare sector comprises three fundamental facets, namely services, products, and finance. It can be further subdivided into numerous sectors and categories and relies on interdisciplinary teams of highly skilled professionals and paraprofessionals to address the healthcare requirements of both individuals and communities.

Healthcare in Canada is delivered through the provincial and territorial systems of publicly funded health care, informally called Medicare. It is guided by the provisions of the Canada Health Act of 1984, and is universal. The 2002 Royal Commission, known as the Romanow Report, revealed that Canadians consider universal access to publicly funded health services as a "fundamental value that ensures national health care insurance for everyone wherever they live in the country."

Telenursing refers to the use of information technology in the provision of nursing services whenever physical distance exists between patient and nurse, or between any number of nurses. As a field, it is part of telemedicine, and has many points of contacts with other medical and non-medical applications, such as telediagnosis, teleconsultation, and telemonitoring. The field, however, is still being developed as the information on telenursing isn't comprehensive enough.
Psychiatric nursing or mental health nursing is the appointed position of a nurse that specialises in mental health, and cares for people of all ages experiencing mental illnesses or distress. These include: neurodevelopmental disorders, schizophrenia, schizoaffective disorder, mood disorders, addiction, anxiety disorders, personality disorders, eating disorders, suicidal thoughts, psychosis, paranoia, and self-harm.
A public hospital, or government hospital, is a hospital which is government owned and is fully funded by the government and operates solely off the money that is collected from taxpayers to fund healthcare initiatives. In almost all the developed countries but the United States of America, and in most of the developing countries, this type of hospital provides medical care free of charge to patients, covering expenses and wages by government reimbursement.
A health professional, healthcare professional, or healthcare worker is a provider of health care treatment and advice based on formal training and experience. The field includes those who work as a nurse, physician, physician assistant, registered dietitian, veterinarian, veterinary technician, optometrist, pharmacist, pharmacy technician, medical assistant, physical therapist, occupational therapist, dentist, midwife, psychologist, audiologist, or healthcare scientist, or who perform services in allied health professions. Experts in public health and community health are also health professionals.
Case management is a managed care technique within the health care coverage system of the United States. It involves an integrated system that manages the delivery of comprehensive healthcare services for enrolled patients. Case managers are employed in almost every aspect of health care and these employ different approaches in the control of clinical actions.
Health advocacy or health activism encompasses direct service to the individual or family as well as activities that promote health and access to health care in communities and the larger public. Advocates support and promote the rights of the patient in the health care arena, help build capacity to improve community health and enhance health policy initiatives focused on available, safe and quality care. Health advocates are best suited to address the challenge of patient-centered care in our complex healthcare system. The Institute of Medicine (IOM) defines patient-centered care as: Health care that establishes a partnership among practitioners, patients, and their families to ensure that decisions respect patients' wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care. Patient-centered care is also one of the overreaching goals of health advocacy, in addition to safer medical systems, and greater patient involvement in healthcare delivery and design.

The healthcare delivery system of Pakistan is complex because it includes healthcare subsystems by federal governments and provincial governments competing with formal and informal private sector healthcare systems. Healthcare is delivered mainly through vertically managed disease-specific mechanisms. The different institutions that are responsible for this include: provincial and district health departments, parastatal organizations, social security institutions, non-governmental organizations (NGOs) and private sector. The country's health sector is also marked by urban-rural disparities in healthcare delivery and an imbalance in the health workforce, with insufficient health managers, nurses, paramedics and skilled birth attendants in the peripheral areas. Pakistan's gross national income per capita in 2021 was $4,990 and the total expenditure on health per capita in 2021 was Rs 657.2 Billion, constituting 1.4% of the country's GDP. The health care delivery system in Pakistan consists of public and private sectors. Under the constitution, health is primarily responsibility of the provincial government, except in the federally administered areas. Health care delivery has traditionally been jointly administered by the federal and provincial governments with districts mainly responsible for implementation. Service delivery is being organized through preventive, promotive, curative and rehabilitative services. The curative and rehabilitative services are being provided mainly at the secondary and tertiary care facilities. Preventive and promotive services, on the other hand, are mainly provided through various national programs; and community health workers’ interfacing with the communities through primary healthcare facilities and outreach activities. The state provides healthcare through a three-tiered healthcare delivery system and a range of public health interventions. Some government/ semi government organizations like the armed forces, Sui Gas, WAPDA, Railways, Fauji Foundation, Employees Social Security Institution and NUST provide health service to their employees and their dependants through their own system, however, these collectively cover about 10% of the population. The private health sector constitutes a diverse group of doctors, nurses, pharmacists, traditional healers, drug vendors, as well as laboratory technicians, shopkeepers and unqualified practitioners.

Health policy can be defined as the "decisions, plans, and actions that are undertaken to achieve specific healthcare goals within a society". According to the World Health Organization, an explicit health policy can achieve several things: it defines a vision for the future; it outlines priorities and the expected roles of different groups; and it builds consensus and informs people.
The philosophy of healthcare is the study of the ethics, processes, and people which constitute the maintenance of health for human beings. For the most part, however, the philosophy of healthcare is best approached as an indelible component of human social structures. That is, the societal institution of healthcare can be seen as a necessary phenomenon of human civilization whereby an individual continually seeks to improve, mend, and alter the overall nature and quality of their life. This perennial concern is especially prominent in modern political liberalism, wherein health has been understood as the foundational good necessary for public life.

Healthcare in Israel is universal and participation in a medical insurance plan is compulsory. All Israeli residents are entitled to basic health care as a fundamental right. The Israeli healthcare system is based on the National Health Insurance Law of 1995, which mandates all citizens resident in the country to join one of four official health insurance organizations, known as Kupat Holim which are run as not-for-profit organizations and are prohibited by law from denying any Israeli resident membership. Israelis can increase their medical coverage and improve their options by purchasing private health insurance. In a survey of 48 countries in 2013, Israel's health system was ranked fourth in the world in terms of efficiency, and in 2014 it ranked seventh out of 51. In 2020, Israel's health system was ranked third most efficient in the world. In 2015, Israel was ranked sixth-healthiest country in the world by Bloomberg rankings and ranked eighth in terms of life expectancy.

Nursing is a health care profession that "integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence". Nurses practice in many specialties with varying levels of certification and responsibility. Nurses comprise the largest component of most healthcare environments. Shortages of qualified nurses are found in many countries.

Healthcare in Senegal is a center topic of discourse in understanding the well-being and vitality of the Senegalese people. As of 2008, there was a need to improve Senegal's infrastructure to promote a healthy, decent living environment for the Senegalese.
In South Africa, private and public health systems exist in parallel. The public system serves the vast majority of the population. Authority and service delivery are divided between the national Department of Health, provincial health departments, and municipal health departments.
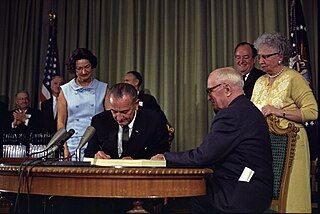
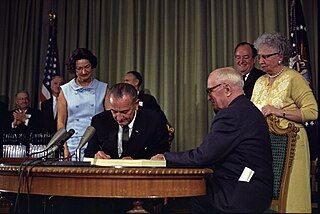
Healthcare in the United States is largely provided by private sector healthcare facilities, and paid for by a combination of public programs, private insurance, and out-of-pocket payments. The U.S. is the only developed country without a system of universal healthcare, and a significant proportion of its population lacks health insurance. The United States spends more on healthcare than any other country, both in absolute terms and as a percentage of GDP; however, this expenditure does not necessarily translate into better overall health outcomes compared to other developed nations. Coverage varies widely across the population, with certain groups, such as the elderly and low-income individuals, receiving more comprehensive care through government programs such as Medicaid and Medicare.

Holistic nursing is a way of treating and taking care of the patient as a whole body, which involves physical, social, environmental, psychological, cultural and religious factors. There are many theories that support the importance of nurses approaching the patient holistically and education on this is there to support the goal of holistic nursing. The important skill to be used in holistic nursing would be communicating skills with patients and other practitioners. This emphasizes that patients being treated would be treated not only in their body but also their mind and spirit.. Holistic nursing is a nursing speciality concerning the integration of one's mind, body, and spirit with his or her environment. This speciality has a theoretical basis in a few grand nursing theories, most notably the science of unitary human beings, as published by Martha E. Rogers in An Introduction to the Theoretical Basis of Nursing, and the mid-range theory Empowered Holistic Nursing Education, as published by Dr. Katie Love. Holistic nursing has gained recognition by the American Nurses Association (ANA) as a nursing specialty with a defined scope of practice and standards. Holistic nursing focuses on the mind, body, and spirit working together as a whole and how spiritual awareness in nursing can help heal illness. Holistic medicine focuses on maintaining optimum well-being and preventing rather than just treating disease.
Genetics nursing is a nursing specialty that focuses on providing genetic healthcare to patients.