Related Research Articles

Physical restraint refers to means of purposely limiting or obstructing the freedom of a person's bodily movement.
A nursing home is a facility for the residential care of older people, senior citizens, or disabled people. Nursing homes may also be referred to as care homes, skilled nursing facilities (SNF) or long-term care facilities. Often, these terms have slightly different meanings to indicate whether the institutions are public or private, and whether they provide mostly assisted living, or nursing care and emergency medical care. Nursing homes are used by people who do not need to be in a hospital, but require care that is hard to provide in a home setting. The nursing home staff attends to the patients' medical and other needs. Most nursing homes have nursing aides and skilled nurses on hand 24 hours a day.
A patient is any recipient of health care services that are performed by healthcare professionals. The patient is most often ill or injured and in need of treatment by a physician, nurse, optometrist, dentist, veterinarian, or other health care provider.
Elder abuse is "a single, or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust, which causes harm or distress to an older person." This definition has been adopted by the World Health Organization (WHO) from a definition put forward by Hourglass in the UK. Laws protecting the elderly from abuse are similar to and related to laws protecting dependent adults from abuse.
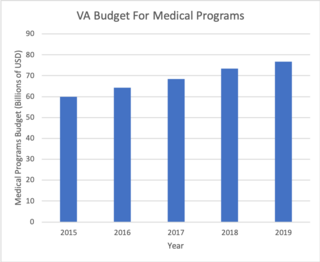
The Veterans Health Administration (VHA) is the component of the United States Department of Veterans Affairs (VA) led by the Under Secretary of Veterans Affairs for Health that implements the healthcare program of the VA through a nationalized healthcare service in the United States, providing healthcare and healthcare-adjacent services to veterans through the administration and operation of 146 VA Medical Centers (VAMC) with integrated outpatient clinics, 772 Community Based Outpatient Clinics (CBOC), and 134 VA Community Living Centers Programs. It is the largest division in the department, and second largest in the entire federal government, employing over 350,000 employees. All VA hospitals, clinics and medical centers are owned by and operated by the Department of Veterans Affairs, and all of the staff employed in VA hospitals are federal employees. Because of this, veterans that qualify for VHA healthcare do not pay premiums or deductibles for their healthcare but may have to make copayments depending on the medical procedure. VHA is not a part of the US Department of Defense Military Health System.
Care in the Community is a British policy of deinstitutionalisation, treating and caring for physically and mentally disabled people in their homes rather than in an institution. Institutional care was the target of widespread criticism during the 1960s and 1970s, but it was not until 1983 that the government of Margaret Thatcher adopted a new policy of care after the Audit Commission published a report called 'Making a Reality of Community Care' which outlined the advantages of domiciliary care.
Developmental disability is a diverse group of chronic conditions, comprising mental or physical impairments that arise before adulthood. Developmental disabilities cause individuals living with them many difficulties in certain areas of life, especially in "language, mobility, learning, self-help, and independent living". Developmental disabilities can be detected early on and persist throughout an individual's lifespan. Developmental disability that affects all areas of a child's development is sometimes referred to as global developmental delay.

Deinstitutionalisation is the process of replacing long-stay psychiatric hospitals with less isolated community mental health services for those diagnosed with a mental disorder or developmental disability. In the late 20th century, it led to the closure of many psychiatric hospitals, as patients were increasingly cared for at home, in halfway houses and clinics, in regular hospitals, or not at all.
A health professional, healthcare professional, or healthcare worker is a provider of health care treatment and advice based on formal training and experience. The field includes those who work as a nurse, physician, physician assistant, registered dietitian, veterinarian, veterinary technician, optometrist, pharmacist, pharmacy technician, medical assistant, physical therapist, occupational therapist, dentist, midwife, psychologist, audiologist, or healthcare scientist, or who perform services in allied health professions. Experts in public health and community health are also health professionals.
Patient advocacy is a process in health care concerned with advocacy for patients, survivors, and caregivers. The patient advocate may be an individual or an organization, concerned with healthcare standards or with one specific group of disorders. The terms patient advocate and patient advocacy can refer both to individual advocates providing services that organizations also provide, and to organizations whose functions extend to individual patients. Some patient advocates are independent and some work for the organizations that are directly responsible for the patient's care.

Nursing is a health care profession that "integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence". Nurses practice in many specialties with varying levels of certification and responsibility. Nurses comprise the largest component of most healthcare environments. Shortages of qualified nurses are found in many countries.
Research published from 2000 to 2020 illustrates increased prevalence rates of sexual violence against people with intellectual disabilities, compared to the general population.:61 The World Health Organization (WHO) funded a study which concluded that 15% of the adult population worldwide in 2012 had a disability, putting them at increased risk of physical, sexual, and intimate partner violence. Of that 15%, 6.1% had intellectual disability with 5.5% experiencing sexual violence. In another 2012 report, the WHO found that worldwide, children with intellectual disabilities experienced a 4.6 times greater risk of sexual violence than those without disability.
Disability abuse is when a person with a disability is abused physically, financially, sexually and/or psychologically due to the person having a disability. This type of abuse has also been considered a hate crime. The abuse is not limited to those who are visibly disabled or physically deformed, but also includes those with learning, intellectual and developmental disabilities or mental illnesses.
Institutional abuse is the maltreatment of a person from a system of power. This can range from acts similar to home-based child abuse, such as neglect, physical and sexual abuse, and hunger, to the effects of assistance programs working below acceptable service standards, or relying on harsh or unfair ways to modify behavior. Institutional abuse occurs within emergency care facilities such as foster homes, group homes, kinship care homes, and pre-adoptive homes. Children who are placed in this type of out of home care are typically in the custody of the state. The maltreatment is usually caused by an employee of the facility.
Professional abuse is "a pattern of conduct in which a person abuses, violates, or takes advantage of a victim within the context of the abuser's profession." This typically involves a violation of the relevant professional organization's code of ethics. Organizational ethics or standards of behavior require the maintenance of professional boundaries and the treatment of people with respect and dignity.
Unlicensed assistive personnel (UAP) are paraprofessionals who assist individuals with physical disabilities, mental impairments, and other health care needs with their activities of daily living (ADLs). UAPs also provide bedside care—including basic nursing procedures—all under the supervision of a registered nurse, licensed practical nurse or other health care professional. UAPs must demonstrate their ability and competence before gaining any expanded responsibilities in a clinical setting. While providing this care, UAPs offer compassion and patience and are part of the patient's healthcare support system. Communication between UAPs and registered nurses (RNs) is key as they are working together in their patients' best interests. The scope of care UAPs are responsible for is delegated by RNs or other clinical licensed professionals.
The nursing organization workplace has been identified as one in which workplace bullying occurs quite frequently. It is thought that relational aggression are relevant. Relational aggression has been studied amongst girls but rarely amongst adult women. According to a finding, 74% of the nurses, 100% of the anesthetists, and 80% of surgical technologists have experienced or witnessed uncivil behaviors like bullying by nursing faculty. There have been many incidents that have occurred throughout the past couple of years. OSHA, which stands for "Occupational Safety and Health Administration" stated that from 2011 to 2013, the United States healthcare workers experienced 15,000 to 20,000 significant injuries while in the workplace.
The Winterbourne View hospital inquiry occurred at Winterbourne View, a private hospital at Hambrook, South Gloucestershire, England, owned and operated by Castlebeck. A Panorama investigation, broadcast on television in 2011, exposed the physical and psychological abuse suffered by people with learning disabilities and challenging behaviour at the hospital.
Diagnostic overshadowing is the attribution of a person’s symptoms to a psychiatric problem when such symptoms actually suggest a comorbid condition. Diagnostic overshadowing occurs when a healthcare professional assumes that a patient's complaint is due to their disability or coexisting mental health condition rather than fully exploring the cause of the patient's symptoms. Often, once a patient has a confirmed diagnosis, there is a tendency to attribute all new behaviors or symptoms to the original diagnosis. Diagnostic overshadowing increases the risk of further health complications and delay in accurate treatment. An example of diagnostic overshadowing may be a patient being diagnosed with a psychiatric problem and prescribed medication due to head banging behavior, but the patient actually has communication challenges and can't express pain in their mouth due to a dental abscess.

Olive Webb is a New Zealand clinical psychologist and former president of the New Zealand Psychological Society from 1993 until 1995. Webb's experiences of poor patient conditions and treatment while working at Sunnyside Hospital in the 1970s inspired her to become a disability advocate. She received the New Zealand Order of Merit in 2008, for services to people with intellectual disabilities. Webb is the longest-serving member of the Canterbury District Health Board, holding a position on the board from 2001 to 2013.
References
- ↑ "Patient Abuse". Stop Fraud Colorado. Colorado Attorney General's Office. Archived from the original on 26 October 2017. Retrieved 25 October 2017.
- 1 2 Goodman, Octavia (2020). Preventing Patient Abuse: Why Abuse Happens and How to Stop It (PDF). The International Association for Healthcare Security and Safety – Foundation.
- ↑ "Medicaid Fraud Definitions". Office of the Attorney General. State of Ohio. Retrieved 25 October 2017.
- ↑ Slavin, Erik (16 January 2010). "Doctor faces court-martial in patient abuse case". Stars & Stripes. Retrieved 25 October 2017.
- ↑ "Patient abuse – nurse struck off". BBC News. 30 April 2003. Retrieved 25 October 2017.
- ↑ Krell, Alexis (9 October 2017). "Doctor charged with sex crimes at Bremerton clinic is at center of women's lawsuit". The News Tribune. Retrieved 25 October 2017.
- ↑ Gorman, Anna (6 January 2015). "When Home Caregivers Kill the Elderly With Neglect". The Atlantic. Retrieved 25 October 2017.
- ↑ The GMC's fitness to practise procedures (PDF). General Medical Council.
- ↑ Fyson, Rachel; Patterson, Anne (2020). "Staff understandings of abuse and poor practice in residential settings for adults with intellectual disabilities". Journal of Applied Research in Intellectual Disabilities. 33 (3): 354–363. doi:10.1111/jar.12677. ISSN 1360-2322. S2CID 204756513.
- ↑ Yon, Yongjie; Ramiro-Gonzalez, Maria; Mikton, Christopher R.; Huber, Manfred; Sethi, Dinesh (2019). "The prevalence of elder abuse in institutional settings: a systematic review and meta-analysis". European Journal of Public Health. 29 (1): 58–67. doi:10.1093/eurpub/cky093. PMC 6359898 . PMID 29878101 . Retrieved 2023-03-12.
- 1 2 AbuDagga, Azza; Carome, Michael; Wolfe, Sidney M. (July 2019). "Time to End Physician Sexual Abuse of Patients: Calling the U.S. Medical Community to Action". Journal of General Internal Medicine. 34 (7): 1330–1333. doi:10.1007/s11606-019-05014-6. ISSN 0884-8734. PMC 6614523 . PMID 31044409.
- 1 2 Dickeson, Edward; Roberts, Rachel; Smout, Matthew F. (2020). "Predicting boundary violation propensity among mental health professionals". Clinical Psychology & Psychotherapy. 27 (6): 814–825. doi:10.1002/cpp.2465. ISSN 1063-3995. S2CID 216595139.
- ↑ Fyson, Rachel; Patterson, Anne (2020). "Staff understandings of abuse and poor practice in residential settings for adults with intellectual disabilities". Journal of Applied Research in Intellectual Disabilities. 33 (3): 354–363. doi:10.1111/jar.12677. ISSN 1360-2322. PMID 31621174. S2CID 204756513.
- 1 2 Phelvin, Andrew (2014-11-26). "Winterbourne View hospital and the social psychology of abuse: Andrew Phelvin analyses accounts of the mistreatment of people with learning disabilities in light of findings from the Stanford prison experiment and events at Abu Ghraib prison, in Iraq". Learning Disability Practice. 17 (10): 25–29. doi:10.7748/ldp.17.10.25.e1581. ISSN 1465-8712.
- ↑ McDonnell, Andrew; Breen, Emma; Deveau, Roy; Goulding, Eimear; Smyth, John (2014-05-28). "How nurses and carers can avoid the slippery slope to abuse: Andrew McDonnell and colleagues outline ways to prevent multiple mistreatment of people with learning disabilities in residential accommodation". Learning Disability Practice. 17 (5): 36–39. doi:10.7748/ldp.17.5.36.e1516. ISSN 1465-8712.
- 1 2 George, Steve (2019-08-02). "Abuse of patients in mental health care in England: history repeating itself". British Journal of Mental Health Nursing. 8 (3): 110–113. doi:10.12968/bjmh.2019.8.3.110. ISSN 2049-5919. S2CID 201171270.
- ↑ Pring, John (2005-06-01). "Why it took so long to expose the abusive regime at Longcare". The Journal of Adult Protection. 7 (1): 15–23. doi:10.1108/14668203200500003. ISSN 1466-8203.
- ↑ Murphy, Glynis (2019-07-23). "Whorlton Hall: a predictable tragedy?". BMJ. 366: l4705. doi:10.1136/bmj.l4705. ISSN 0959-8138. PMID 31337610. S2CID 198191618.
- ↑ "Edenfield Centre: Staff sacked over abuse at hospital". BBC. 2022-10-14. Retrieved 2023-09-01.