The Diagnostic and Statistical Manual of Mental Disorders is a publication by the American Psychiatric Association (APA) for the classification of mental disorders using a common language and standard criteria. It is the main book for the diagnosis and treatment of mental disorders in the United States and Australia, while in other countries it may be used in conjunction with other documents. The DSM-5 is considered one of the principal guides of psychiatry, along with the International Classification of Diseases ICD, CCMD, and the Psychodynamic Diagnostic Manual. However, not all providers rely on the DSM-5 as a guide, since the ICD's mental disorder diagnoses are used around the world and scientific studies often measure changes in symptom scale scores rather than changes in DSM-5 criteria to determine the real-world effects of mental health interventions.
Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.

Schizophrenia is a mental disorder characterized by reoccurring episodes of psychosis that are correlated with a general misperception of reality. Other common signs include hallucinations, delusions, disorganized thinking, social withdrawal, and flat affect. Symptoms develop gradually and typically begin during young adulthood and are never resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a psychiatric history that includes the person's reported experiences, and reports of others familiar with the person. For a diagnosis of schizophrenia, the described symptoms need to have been present for at least six months or one month. Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders, anxiety disorders, and obsessive–compulsive disorder.

Paul Eugen Bleuler was a Swiss psychiatrist and humanist most notable for his contributions to the understanding of mental illness. He coined several psychiatric terms including "schizophrenia", "schizoid", "autism", depth psychology and what Sigmund Freud called "Bleuler's happily chosen term ambivalence".
Schizotypal personality disorder, also known as schizotypal disorder, is a cluster A personality disorder. The Diagnostic and Statistical Manual of Mental Disorders (DSM) classification describes the disorder specifically as a personality disorder characterized by thought disorder, paranoia, a characteristic form of social anxiety, derealization, transient psychosis, and unconventional beliefs. People with this disorder feel pronounced discomfort in forming and maintaining social connections with other people, primarily due to the belief that other people harbor negative thoughts and views about them. Peculiar speech mannerisms and socially unexpected modes of dress are also characteristic. Schizotypal people may react oddly in conversations, not respond, or talk to themselves. They frequently interpret situations as being strange or having unusual meanings for them; paranormal and superstitious beliefs are common. Schizotypal people usually disagree with the suggestion that their thoughts and behaviors are a 'disorder' and seek medical attention for depression or anxiety instead. Schizotypal personality disorder occurs in approximately 3% of the general population and is more commonly diagnosed in males.

Jim van Os is a Dutch academic and psychiatrist. He is Professor of Psychiatry and medical manager of the Brain Center at Utrecht University Medical Center, the Netherlands.
The trauma model of mental disorders, or trauma model of psychopathology, emphasises the effects of physical, sexual and psychological trauma as key causal factors in the development of psychiatric disorders, including depression and anxiety as well as psychosis, whether the trauma is experienced in childhood or adulthood. It conceptualises people as having understandable reactions to traumatic events rather than suffering from mental illness.
The biopsychiatry controversy is a dispute over which viewpoint should predominate and form a basis of psychiatric theory and practice. The debate is a criticism of a claimed strict biological view of psychiatric thinking. Its critics include disparate groups such as the antipsychiatry movement and some academics.
Risk factors of schizophrenia include many genetic and environmental phenomena. The prevailing model of schizophrenia is that of a special neurodevelopmental disorder with no precise boundary or single cause. Schizophrenia is thought to develop from very complex gene–environment interactions with vulnerability factors. The interactions of these risk factors are intricate, as numerous and diverse medical insults from conception to adulthood can be involved. The combination of genetic and environmental factors leads to deficits in the neural circuits that affect sensory input and cognitive functions. Historically, this theory has been broadly accepted but impossible to prove given ethical limitations. The first definitive proof that schizophrenia arises from multiple biological changes in the brain was recently established in human tissue grown from patient stem cells, where the complexity of disease was found to be "even more complex than currently accepted" due to cell-by-cell encoding of schizophrenia-related neuropathology.
In genetic epidemiology, endophenotype is a term used to separate behavioral symptoms into more stable phenotypes with a clear genetic connection. By seeing the EP notion as a special case of a larger collection of multivariate genetic models, which may be fitted using currently accessible methodology, it is possible to maximize its valuable potential lessons for etiological study in psychiatric disorders. The concept was coined by Bernard John and Kenneth R. Lewis in a 1966 paper attempting to explain the geographic distribution of grasshoppers. They claimed that the particular geographic distribution could not be explained by the obvious and external "exophenotype" of the grasshoppers, but instead must be explained by their microscopic and internal "endophenotype". The endophenotype idea represents the influence of two important conceptual currents in biology and psychology research. An adequate technology would be required to perceive the endophenotype, which represents an unobservable latent entity that cannot be directly observed with the unaided naked eye. In the investigation of anxiety and affective disorders, the endophenotype idea has gained popularity.

Madhouse: A Tragic Tale of Megalomania and Modern Medicine is a 2005 book by the psychiatric sociologist Andrew Scull which discusses the work of the controversial psychiatrist Henry Cotton at Trenton State Hospital in New Jersey in the 1920s.
The word schizophrenia was coined by the Swiss psychiatrist Eugen Bleuler in 1908, and was intended to describe the separation of function between personality, thinking, memory, and perception. Bleuler introduced the term on 24 April 1908 in a lecture given at a psychiatric conference in Berlin and in a publication that same year. Bleuler later expanded his new disease concept into a monograph in 1911, which was finally translated into English in 1950.
Political abuse of psychiatry, also commonly referred to as punitive psychiatry, is the misuse of psychiatry, including diagnosis, detention, and treatment, for the purposes of obstructing the human rights of individuals and/or groups in a society. In other words, abuse of psychiatry is the deliberate action of having citizens psychiatrically diagnosed who need neither psychiatric restraint nor psychiatric treatment. Psychiatrists have been involved in human rights abuses in states across the world when the definitions of mental disease were expanded to include political disobedience. As scholars have long argued, governmental and medical institutions code menaces to authority as mental diseases during political disturbances. Nowadays, in many countries, political prisoners are sometimes confined and abused in psychiatric hospitals.
Childhood schizophrenia is similar in characteristics of schizophrenia that develops at a later age, but has an onset before the age of 13 years, and is more difficult to diagnose. Schizophrenia is characterized by positive symptoms that can include hallucinations, delusions, and disorganized speech; negative symptoms, such as blunted affect and avolition and apathy, and a number of cognitive impairments. Differential diagnosis is problematic since several other neurodevelopmental disorders, including autism spectrum disorder, language disorder, and attention deficit hyperactivity disorder, also have signs and symptoms similar to childhood-onset schizophrenia.
The diagnosis of schizophrenia, a psychotic disorder, is based on criteria in either the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, or the World Health Organization's International Classification of Diseases (ICD). Clinical assessment of schizophrenia is carried out by a mental health professional based on observed behavior, reported experiences, and reports of others familiar with the person. Diagnosis is usually made by a psychiatrist. Associated symptoms occur along a continuum in the population and must reach a certain severity and level of impairment before a diagnosis is made. Schizophrenia has a prevalence rate of 0.3-0.7% in the United States

The Kraepelinian dichotomy is the division of the major endogenous psychoses into the disease concepts of dementia praecox, which was reformulated as schizophrenia by Eugen Bleuler by 1908, and manic-depressive psychosis, which has now been reconceived as bipolar disorder. This division was formally introduced in the sixth edition of Emil Kraepelin's psychiatric textbook Psychiatrie. Ein Lehrbuch für Studirende und Aerzte, published in 1899. It has been highly influential on modern psychiatric classification systems, the DSM and ICD, and is reflected in the taxonomic separation of schizophrenia from affective psychosis. However, there is also a diagnosis of schizoaffective disorder to cover cases that seem to show symptoms of both.

Doctoring the Mind: Why psychiatric treatments fail is a 2009 book by Richard Bentall, his thesis is critical of contemporary Western psychiatry. Bentall, a professor of clinical psychology, argues that recent scientific research shows that the medical approach to mental illness is fatally flawed. According to Bentall, it seems there is no "evidence that psychiatry has made a positive impact on human welfare" and "patients are doing no better today than they did a hundred years ago".
Evolutionary psychiatry, also known as Darwinian psychiatry, is a theoretical approach to psychiatry that aims to explain psychiatric disorders in evolutionary terms. As a branch of the field of evolutionary medicine, it is distinct from the medical practice of psychiatry in its emphasis on providing scientific explanations rather than treatments for mental disorder. This often concerns questions of ultimate causation. For example, psychiatric genetics may discover genes associated with mental disorders, but evolutionary psychiatry asks why those genes persist in the population. Other core questions in evolutionary psychiatry are why heritable mental disorders are so common how to distinguish mental function and dysfunction, and whether certain forms of suffering conveyed an adaptive advantage. Disorders commonly considered are depression, anxiety, schizophrenia, autism, eating disorders, and others. Key explanatory concepts are of evolutionary mismatch and the fact that evolution is guided by reproductive success rather than health or wellbeing. Rather than providing an alternative account of the cause of mental disorder, evolutionary psychiatry seeks to integrate findings from traditional schools of psychology and psychiatry such as social psychology, behaviourism, biological psychiatry and psychoanalysis into a holistic account related to evolutionary biology. In this sense, it aims to meet the criteria of a Kuhnian paradigm shift.
Psychiatry is, and has historically been, viewed as controversial by those under its care, as well as sociologists and psychiatrists themselves. There are a variety of reasons cited for this controversy, including the subjectivity of diagnosis, the use of diagnosis and treatment for social and political control including detaining citizens and treating them without consent, the side effects of treatments such as electroconvulsive therapy, antipsychotics and historical procedures like the lobotomy and other forms of psychosurgery or insulin shock therapy, and the history of racism within the profession in the United States.
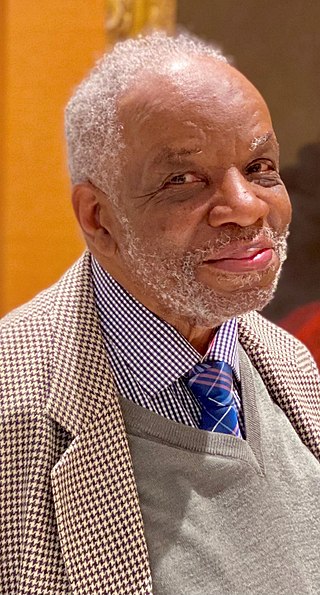
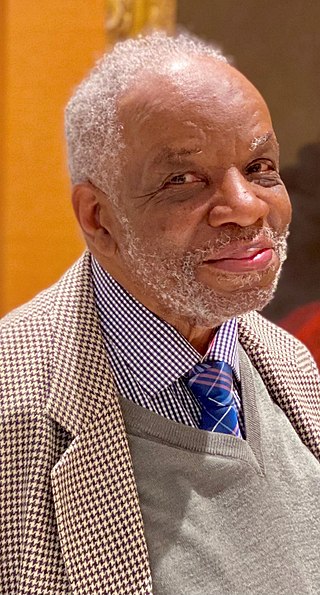
Aggrey Washington Burke FRCPsych is a British retired psychiatrist and academic, born in Jamaica, who spent the majority of his medical career at St George's Hospital in London, UK, specialising in transcultural psychiatry and writing literature on changing attitudes towards black people and mental health. He has carried out extensive research on racism and mental illness and is the first black consultant psychiatrist appointed by Britain's National Health Service (NHS).