Anemia or anaemia is a blood disorder in which the blood has a reduced ability to carry oxygen due to a lower than normal number of red blood cells, or a reduction in the amount of hemoglobin. When anemia comes on slowly, the symptoms are often vague, such as tiredness, weakness, shortness of breath, headaches, and a reduced ability to exercise. When anemia is acute, symptoms may include confusion, feeling like one is going to pass out, loss of consciousness, and increased thirst. Anemia must be significant before a person becomes noticeably pale. Symptoms of anemia depend on how quickly hemoglobin decreases. Additional symptoms may occur depending on the underlying cause. Preoperative anemia can increase the risk of needing a blood transfusion following surgery. Anemia can be temporary or long term and can range from mild to severe.

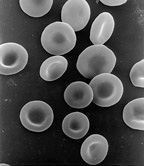
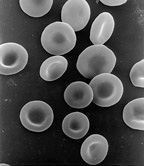
Spherocytosis is the presence of spherocytes in the blood, i.e. erythrocytes that are sphere-shaped rather than bi-concave disk shaped as normal. Spherocytes are found in all hemolytic anemias to some degree. Hereditary spherocytosis and autoimmune hemolytic anemia are characterized by having only spherocytes.
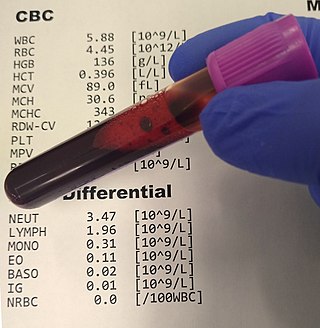
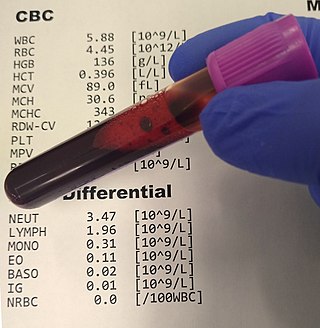
A complete blood count (CBC), also known as a full blood count (FBC), is a set of medical laboratory tests that provide information about the cells in a person's blood. The CBC indicates the counts of white blood cells, red blood cells and platelets, the concentration of hemoglobin, and the hematocrit. The red blood cell indices, which indicate the average size and hemoglobin content of red blood cells, are also reported, and a white blood cell differential, which counts the different types of white blood cells, may be included.

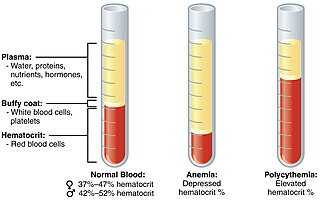
The hematocrit, also known by several other names, is the volume percentage (vol%) of red blood cells (RBCs) in blood, measured as part of a blood test. The measurement depends on the number and size of red blood cells. It is normally 40.7–50.3% for males and 36.1–44.3% for females. It is a part of a person's complete blood count results, along with hemoglobin concentration, white blood cell count and platelet count.
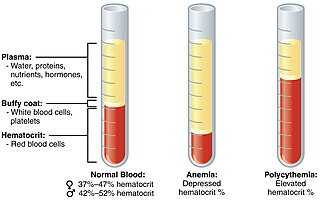
Polycythemia is a laboratory finding in which the hematocrit and/or hemoglobin concentration are increased in the blood. Polycythemia is sometimes called erythrocytosis, and there is significant overlap in the two findings, but the terms are not the same: polycythemia describes any increase in hematocrit and/or hemoglobin, while erythrocytosis describes an increase specifically in the number of red blood cells in the blood.
Iron-deficiency anemia is anemia caused by a lack of iron. Anemia is defined as a decrease in the number of red blood cells or the amount of hemoglobin in the blood. When onset is slow, symptoms are often vague such as feeling tired, weak, short of breath, or having decreased ability to exercise. Anemia that comes on quickly often has more severe symptoms, including confusion, feeling like one is going to pass out or increased thirst. Anemia is typically significant before a person becomes noticeably pale. Children with iron deficiency anemia may have problems with growth and development. There may be additional symptoms depending on the underlying cause.

Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis foetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.
Hemolytic disease of the newborn (anti-Kell1) is the second most common cause of severe hemolytic disease of the newborn (HDN) after Rh disease. Anti-Kell1 is becoming relatively more important as prevention of Rh disease is also becoming more effective.
Hemolytic disease of the newborn (anti-Rhc) can range from a mild to a severe disease. It is the third most common cause of severe HDN. Rh disease is the most common and hemolytic disease of the newborn (anti-Kell) is the second most common cause of severe HDN. It occurs more commonly in women who are Rh D negative.
Epoetin alfa is a human erythropoietin produced in cell culture using recombinant DNA technology. Authorised by the European Medicines Agency on 28 August 2007, it stimulates erythropoiesis and is used to treat anemia, commonly associated with chronic kidney failure and cancer chemotherapy.
An exchange transfusion is a blood transfusion in which the patient's blood or components of it are exchanged with other blood or blood products. The patient's blood is removed and replaced by donated blood or blood components. This exchange transfusion can be performed manually or using a machine (apheresis).
Anemia of prematurity (AOP) refers to a form of anemia affecting preterm infants with decreased hematocrit. AOP is a normochromic, normocytic hypoproliferative anemia. The primary mechanism of AOP is a decrease in erythropoietin (EPO), a red blood cell growth factor.
Hemolytic disease of the newborn (anti-RhE) is caused by the anti-RhE antibody of the Rh blood group system. The anti-RhE antibody can be naturally occurring, or arise following immune sensitization after a blood transfusion or pregnancy.
Patient Blood Management (PBM) is a set of medical practices designed to optimise the care of patients who might need a blood transfusion. Patient blood management programs use an organized framework to improve blood health, thus increasing patient safety and quality of life, reducing costs, and improving clinical outcomes. Some strategies to accomplish this include ensuring that anemia is treated prior to a surgical operation, using surgical techniques that limit blood loss, and returning blood lost during surgery to the patient via intraoperative blood salvage.
Hemoglobin H Disease, also called alpha-thalassemia intermedia, is a disease affecting hemoglobin, the oxygen carrying molecule within red blood cells. It is a form of Alpha-thalassemia which most commonly occurs due to deletion of 3 out of 4 of the α-globin genes.
Neonates are defined as babies up to 28 days after birth. Most extremely preterm babies require at least one red cell transfusion; this is partly due to the amount of blood removed with blood samples compared to the baby's total blood volume and partly due to anemia of prematurity. Most transfusions are given as small volume top-up transfusions to increase the baby's hemoglobin above a certain pre-defined level, or because the baby is unwell due to the anemia. Possible side-effects of anemia in babies can be poor growth, lethargy and episodes of apnea. Exchange blood transfusion is used to treat a rapidly rising bilirubin that does not respond to treatment with phototherapy or intravenous immunoglobulin. This is usually due to hemolytic disease of the newborn, but may also be due to other causes, e.g., G6PD deficiency.
Anemia is a condition in which blood has a lower-than-normal amount of red blood cells or hemoglobin. Anemia in pregnancy is a decrease in the total red blood cells (RBCs) or hemoglobin in the blood during pregnancy. Anemia is an extremely common condition in pregnancy world-wide, conferring a number of health risks to mother and child. While anemia in pregnancy may be pathologic, in normal pregnancies, the increase in RBC mass is smaller than the increase in plasma volume, leading to a mild decrease in hemoglobin concentration referred to as physiologic anemia. Maternal signs and symptoms are usually non-specific, but can include: fatigue, pallor, dyspnea, palpitations, and dizziness. There are numerous well-known maternal consequences of anemia including: maternal cardiovascular strain, reduced physical and mental performance, reduced peripartum blood reserves, increased risk for peripartum blood product transfusion, and increased risk for maternal mortality.
An Intrauterine transfusion (IUT) is a procedure that provides blood to a fetus, most commonly through the umbilical cord. It is used in cases of severe fetal anemia, such as when fetal red blood cells are being destroyed by maternal antibodies. IUTs are performed by perinatologists at hospitals or specialized centers.

Transfusion-dependent anemia is a form of anemia characterized by the need for continuous blood transfusion. It is a condition that results from various diseases, and is associated with decreased survival rates. Regular transfusion is required to reduce the symptoms of anemia by increasing functional red blood cells and hemoglobin count. Symptoms may vary based on the severity of the condition and the most common symptom is fatigue. Various diseases can lead to transfusion-dependent anemia, most notably myelodysplastic syndromes (MDS) and thalassemia. Due to the number of diseases that can cause transfusion-dependent anemia, diagnosing it is more complicated. Transfusion dependence occurs when an average of more than 2 units of blood transfused every 28 days is required over a period of at least 3 months. Myelodysplastic syndromes is often only diagnosed when patients become anemic, and transfusion-dependent thalassemia is diagnosed based on gene mutations. Screening for heterozygosity in the thalassemia gene is an option for early detection.
Hemolytic jaundice, also known as prehepatic jaundice, is a type of jaundice arising from hemolysis or excessive destruction of red blood cells, when the byproduct bilirubin is not excreted by the hepatic cells quickly enough. Unless the patient is concurrently affected by hepatic dysfunctions or is experiencing hepatocellular damage, the liver does not contribute to this type of jaundice.