Related Research Articles

Antidepressants are a class of medications used to treat major depressive disorder, anxiety disorders, chronic pain, and addiction.
An anxiolytic is a medication or other intervention that reduces anxiety. This effect is in contrast to anxiogenic agents which increase anxiety. Anxiolytic medications are used for the treatment of anxiety disorders and their related psychological and physical symptoms.

Monoamine oxidase inhibitors (MAOIs) are a class of drugs that inhibit the activity of one or both monoamine oxidase enzymes: monoamine oxidase A (MAO-A) and monoamine oxidase B (MAO-B). They are best known as effective antidepressants, especially for treatment-resistant depression and atypical depression. They are also used to treat panic disorder, social anxiety disorder, Parkinson's disease, and several other disorders.
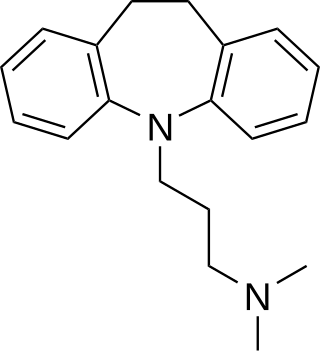
Tricyclic antidepressants (TCAs) are a class of medications that are used primarily as antidepressants. TCAs were discovered in the early 1950s and were marketed later in the decade. They are named after their chemical structure, which contains three rings of atoms. Tetracyclic antidepressants (TeCAs), which contain four rings of atoms, are a closely related group of antidepressant compounds.

Psychopharmacology is the scientific study of the effects drugs have on mood, sensation, thinking, behavior, judgment and evaluation, and memory. It is distinguished from neuropsychopharmacology, which emphasizes the correlation between drug-induced changes in the functioning of cells in the nervous system and changes in consciousness and behavior.

Akathisia is a movement disorder characterized by a subjective feeling of inner restlessness accompanied by mental distress and an inability to sit still. Usually, the legs are most prominently affected. Those affected may fidget, rock back and forth, or pace, while some may just have an uneasy feeling in their body. The most severe cases may result in poor adherence to medications, exacerbation of psychiatric symptoms, and, because of this, aggression, violence, and/or suicidal thoughts. Akathisia is also associated with threatening behaviour and physical aggression in mentally disordered patients. However, the attempts to find potential links between akathisia and emerging suicidal or homicidal behaviour were not systematic and were mostly based on a limited number of case reports and small case series. Apart from these few low-quality studies, there is another more recent and better quality study that concludes akathisia cannot be reliably linked to the presence of suicidal behaviour in patients treated with antipsychotic medication.
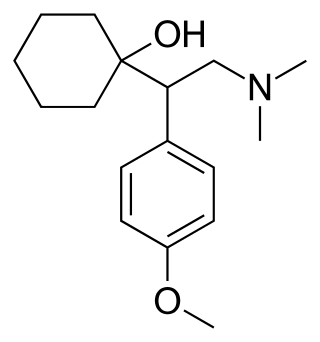
Venlafaxine, sold under the brand name Effexor among others, is an antidepressant medication of the serotonin–norepinephrine reuptake inhibitor (SNRI) class. It is used to treat major depressive disorder, generalized anxiety disorder, panic disorder, and social anxiety disorder. Studies have shown that venlafaxine improves post-traumatic stress disorder (PTSD). It may also be used for chronic pain. It is taken by mouth. It is also available as the salt venlafaxine besylate in an extended-release formulation.

Serotonin–norepinephrine reuptake inhibitors (SNRIs) are a class of antidepressant medications used to treat major depressive disorder (MDD), anxiety disorders, social phobia, chronic neuropathic pain, fibromyalgia syndrome (FMS), and menopausal symptoms. Off-label uses include treatments for attention-deficit hyperactivity disorder (ADHD), obsessive–compulsive disorder (OCD), and migraine prevention. SNRIs are monoamine reuptake inhibitors; specifically, they inhibit the reuptake of serotonin and norepinephrine. These neurotransmitters are thought to play an important role in mood regulation. SNRIs can be contrasted with the selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibitors (NRIs), which act upon single neurotransmitters.
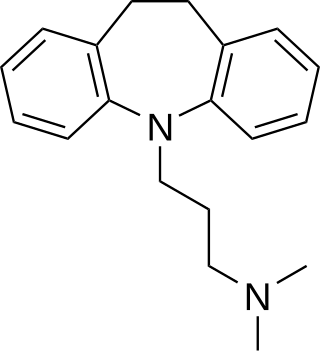
Imipramine, sold under the brand name Tofranil, among others, is a tricyclic antidepressant (TCA) mainly used in the treatment of depression. It is also effective in treating anxiety and panic disorder. Imipramine is taken by mouth.

Clomipramine, sold under the brand name Anafranil among others, is a tricyclic antidepressant (TCA). It is used in the treatment of various conditions, most-notably obsessive–compulsive disorder but also many other disorders, including panic disorder, major depressive disorder, trichotilomania, body dysmorphic disorder and chronic pain. It has also been notably used to treat premature ejaculation and the cataplexy associated with narcolepsy.
Biological psychiatry or biopsychiatry is an approach to psychiatry that aims to understand mental disorder in terms of the biological function of the nervous system. It is interdisciplinary in its approach and draws on sciences such as neuroscience, psychopharmacology, biochemistry, genetics, epigenetics and physiology to investigate the biological bases of behavior and psychopathology. Biopsychiatry is the branch of medicine which deals with the study of the biological function of the nervous system in mental disorders.

Isocarboxazid is a non-selective, irreversible monoamine oxidase inhibitor (MAOI) of the hydrazine class used as an antidepressant. Along with phenelzine and tranylcypromine, it is one of only three classical MAOIs still available for clinical use in the treatment of psychiatric disorders in the United States, though it is not as commonly employed in comparison to the others.

Trimipramine, sold under the brand name Surmontil among others, is a tricyclic antidepressant (TCA) which is used to treat depression. It has also been used for its sedative, anxiolytic, and weak antipsychotic effects in the treatment of insomnia, anxiety disorders, and psychosis, respectively. The drug is described as an atypical or "second-generation" TCA because, unlike other TCAs, it seems to be a fairly weak monoamine reuptake inhibitor. Similarly to other TCAs, however, trimipramine does have antihistamine, antiserotonergic, antiadrenergic, antidopaminergic, and anticholinergic activities.
Antidepressant discontinuation syndrome, also called antidepressant withdrawal syndrome, is a condition that can occur following the interruption, reduction, or discontinuation of antidepressant medication following its continuous use of at least a month. The symptoms may include flu-like symptoms, trouble sleeping, nausea, poor balance, sensory changes, akathisia, intrusive thoughts, depersonalization and derealization, mania, anxiety, and depression. The problem usually begins within three days and may last for several weeks or months. Rarely psychosis may occur.
Treatment-resistant depression (TRD) is a term used in psychiatry to describe people with major depressive disorder (MDD) who do not respond adequately to a course of appropriate antidepressant medication within a certain time. Definitions of treatment-resistant depression vary, and they do not include a resistance to psychotherapy. Inadequate response has most commonly been defined as less than 50% reduction in depressive symptoms following treatment with at least one antidepressant medication, although definitions vary widely. Some other factors that may contribute to inadequate treatment are: a history of repeated or severe adverse childhood experiences, early discontinuation of treatment, insufficient dosage of medication, patient noncompliance, misdiagnosis, cognitive impairment, low income and other socio-economic variables, and concurrent medical conditions, including comorbid psychiatric disorders. Cases of treatment-resistant depression may also be referred to by which medications people with treatment-resistant depression are resistant to. In treatment-resistant depression adding further treatments such as psychotherapy, lithium, or aripiprazole is weakly supported as of 2019.
Mental disorders are classified as a psychological condition marked primarily by sufficient disorganization of personality, mind, and emotions to seriously impair the normal psychological and often social functioning of the individual. Individuals diagnosed with certain mental disorders can be unable to function normally in society. Mental disorders may consist of several affective, behavioral, cognitive and perceptual components. The acknowledgement and understanding of mental health conditions has changed over time and across cultures. There are still variations in the definition, classification, and treatment of mental disorders.
Psychoneuroendocrinology is the clinical study of hormone fluctuations and their relationship to human behavior. It may be viewed from the perspective of psychiatry, where in certain mood disorders, there are associated neuroendocrine or hormonal changes affecting the brain. It may also be viewed from the perspective of endocrinology, where certain endocrine disorders can be associated with negative health outcomes and psychiatric illness. Brain dysfunctions associated with the hypothalamus-pituitary-adrenal axis HPA axis can affect the endocrine system, which in turn can result in physiological and psychological symptoms. This complex blend of psychiatry, psychology, neurology, biochemistry, and endocrinology is needed to comprehensively understand and treat symptoms related to the brain, endocrine system (hormones), and psychological health..

In applied psychology, interventions are actions performed to bring about change in people. A wide range of intervention strategies exist and they are directed towards various types of issues. Most generally, it means any activities used to modify behavior, emotional state, or feelings. Psychological interventions have many different applications and the most common use is for the treatment of mental disorders, most commonly using psychotherapy. The ultimate goal behind these interventions is not only to alleviate symptoms but also to target the root cause of mental disorders.

Selective serotonin reuptake inhibitors (SSRIs) are a class of drugs that are typically used as antidepressants in the treatment of major depressive disorder, anxiety disorders, and other psychological conditions.
References
- ↑ Rose, Nikolas (2010). "Chapter 2 Historical changes in mental health practice". Historical changes in mental health practice. Oxford University Press. doi:10.1093/med/9780199565498.003.0012. ISBN 9780199565498.
- ↑ Grob, Gerald N. (2010). "Chapter 3 Mental health policy in modern America". Mental health policy in modern America. Oxford University Press. doi:10.1093/med/9780199565498.003.0014. ISBN 9780199565498.
- ↑ Becker, Thomas; Koesters, Markus (2010). "Chapter 16 Psychiatric outpatient clinics". Psychiatric outpatient clinics. Oxford University Press. doi:10.1093/med/9780199565498.003.0086. ISBN 9780199565498.
- ↑ Shaywitz, Jonathan; Marder, Stephen (2010). "Chapter 22 Medication treatment for anxiety, depression, schizophrenia, and bipolar disorder in the community setting". Medication treatment for anxiety, depression, schizophrenia, and bipolar disorder in the community setting. Oxford University Press. doi:10.1093/med/9780199565498.003.0109. ISBN 9780199565498.
- ↑ Jaramillo-Gonzalez, Luis Eduardo; Sanchez-Pedraza, Ricardo; Herazo, Maria Isabel (2014). "The frequency of rehospitalization and associated factors in Colombian psychiatric patients: a cohort study". BMC Psychiatry. 14: 161. doi: 10.1186/1471-244X-14-161 . PMC 4059735 . PMID 24888262.
- ↑ Oyffe I, Kurs R, Gelkopf M, Melamed Y, Bleich A (2009). "Revolving-door patients in a public psychiatric hospital in Israel: cross sectional study". Croat Med J. 50 (6): 575–82. doi:10.3325/cmj.2009.50.575. PMC 2802091 . PMID 20017226.
- ↑ Frick U, Frick H, Langguth B, Landgrebe M, Hübner-Liebermann B, Hajak G (2013). "The revolving door phenomenon revisited: time to readmission in 17'145 [corrected] patients with 37'697 hospitalisations at a German psychiatric hospital". PLOS ONE. 8 (10): e75612. doi: 10.1371/journal.pone.0075612 . PMC 3792950 . PMID 24116059.
- ↑ "Are There Schizophrenics for Whom Drugs May be Unnecessary or Contraindicated?". Authors Rappaport M, Hopkins HK, Hall, Belleza and Silverman. International Pharmacopsychiatry (Neuropsychobiology) 13:100–111 (1978)
- ↑ "The Julius Axelrod Papers". National Library of Medicine. Retrieved 6 May 2013.
- ↑ Martin, Emily; Rhodes, Lorna A. "Resources on the History of Psychiatry" (PDF). National Library of Medicine. Retrieved 6 May 2013.
- ↑ Stroman, Duane (2003). The Disability Rights Movement: From Deinstitutionalization to Self-determination. University Press of America.
- ↑ Eisenberg, Leon; Guttmacher, Laurence (August 2010). "Were we all asleep at the switch? A personal reminiscence of psychiatry from 1940 to 2010". Acta Psychiatrica Scandinavica . 122 (2): 89–102. doi: 10.1111/j.1600-0447.2010.01544.x . PMID 20618173.
- ↑ Top 25 Psychiatric Medication Prescriptions for 2013 Author John M. Grohol, Psy.D..Psych Central.
- ↑ Murray, Bridget (October 2003). "A Brief History of RxP". APA Monitor. Retrieved 11 April 2007.
- ↑ DeVane, C. Lindsay. "New Methods for the Administration of Psychiatric Medicine". Medscape. Retrieved 6 May 2013.
- ↑ Brissos, Sofia; Veguilla, Miguel Ruiz; Taylor, David; Balanzá-Martinez, Vicent (2014). "The role of long-acting injectable antipsychotics in schizophrenia: a critical appraisal". Therapeutic Advances in Psychopharmacology. 4 (5): 198–219. doi:10.1177/2045125314540297. ISSN 2045-1253. PMC 4212490 . PMID 25360245.
- ↑ Moncrieff, Joanna (23 March 2006). "Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse". Acta Psychiatrica Scandinavica. 114 (1): 3–13. doi:10.1111/j.1600-0447.2006.00787.x. ISSN 1600-0447. PMID 16774655. S2CID 6267180. Archived from the original on 5 January 2013. Retrieved 3 May 2009.
- ↑ Michael S Ritsner (2013) "Polypharmacy in Psychiatry Practice, Volume I: Multiple Medication Use Strategies"
- ↑ Michael S Ritsner (2013) "Polypharmacy in Psychiatry Practice, Volume II: Use of Polypharmacy in the "Real World""
- ↑ Otto Benkert, Wolfgang Maier, Karl Rickels (2012) "Methodology of the Evaluation of Psychotropic Drugs"
- ↑ Schatzberg, A.F. (2000). "New indications for antidepressants". Journal of Clinical Psychiatry. 61 (11): 9–17. PMID 10926050.
- 1 2 3 Stahl, S. M. (2008). Stahl's Essential Psychopharmacology: Neuroscientific basis and practical applications . Cambridge University Press.
- ↑ Stephen M. Stahl, M.D.; et al. (2004). "A Review of the Neuropharmacology of Bupropion, a Dual Norepinephrine and Dopamine Reuptake Inhibitor" (PDF). Journal of Clinical Psychiatry; 6(04) 159-166 2004 PHYSICIANS POSTGRADUATE PRESS, INC. Retrieved 2006-09-02.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Ashton, Heather (July 1994). "Guidelines for the rational use of benzodiazepines. When and what to use". Drugs. 48 (1): 25–40. doi:10.2165/00003495-199448010-00004. PMID 7525193. S2CID 46966796.
- ↑ Martin, Hannah (2020-08-14). "Euthanasia referendum: What drugs are used in assisted dying, and how do they work?". www.stuff.co.nz. Retrieved 2024-04-14.
- ↑ Pepper, Brianne Marlene; Chan, Hedia; Ward, Michael P.; Quain, Anne (2023-04-27). "Euthanasia of Dogs by Australian Veterinarians: A Survey of Current Practices". Veterinary Sciences. 10 (5): 317. doi: 10.3390/vetsci10050317 . ISSN 2306-7381. PMC 10224218 . PMID 37235400.
- ↑ MacKinnon GL, Parker WA (1982). "Benzodiazepine withdrawal syndrome: a literature review and evaluation". Am J Drug Alcohol Abuse. 9 (1): 19–33. doi:10.3109/00952998209002608. PMID 6133446.
- ↑ Kirk, Stuart (2013). Mad science : psychiatric coercion, diagnosis, and drugs. New Brunswick, N.J: Transaction Publishers. p. 185. ISBN 978-1-4128-4976-0. OCLC 808769553.
- ↑ Kirk, Stuart A. (2013). Mad Science: Psychiatric Coercion, Diagnosis, and Drugs. Transaction Publishers.
- ↑ Szasz, Thomas Stephen (2003). Ceremonial chemistry : the ritual persecution of drugs, addicts, and pushers. Syracuse Univ. Press. ISBN 0-8156-0768-7. OCLC 834790127.
- ↑ Szasz, Thomas S. (October 1974). "The Myth of Psychotherapy". American Journal of Psychotherapy. 28 (4): 517–526. doi:10.1176/appi.psychotherapy.1974.28.4.517. ISSN 0002-9564. PMID 4429160.
- ↑ "Kampf den Vorurteilen - Wie uns Stereotype und Klischees in die Irre führen können". 21 July 2021.
- ↑ Moncrieff, Joanna; Cohen, David (May 29, 2009). "How do psychiatric drugs work?". The BMJ. 338: b1963. doi:10.1136/bmj.b1963. PMC 3230235 . PMID 19482870.
- ↑ Ho, Beng-Choon; Andreasen, Nancy C.; Ziebell, Steven; Pierson, Ronald; Magnotta, Vincent (February 2011). "Long-term Antipsychotic Treatment and Brain Volumes". Archives of General Psychiatry. 68 (2): 128–137. doi:10.1001/archgenpsychiatry.2010.199. ISSN 0003-990X. PMC 3476840 . PMID 21300943.
- ↑ "Antipsychotics and the Shrinking Brain". Psychiatric Times. Psychiatric Times Vol 28 No 4. 28 (4). 4 May 2011. Retrieved 2020-07-25.