The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of the heart. Their function in the respiratory system is to extract oxygen from the air and transfer it into the bloodstream, and to release carbon dioxide from the bloodstream into the atmosphere, in a process of gas exchange. The pleurae, which are thin, smooth, and moist, serve to reduce friction between the lungs and chest wall during breathing, allowing for easy and effortless movements of the lungs.

Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV) is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Oxygen toxicity is a condition resulting from the harmful effects of breathing molecular oxygen at increased partial pressures. Severe cases can result in cell damage and death, with effects most often seen in the central nervous system, lungs, and eyes. Historically, the central nervous system condition was called the Paul Bert effect, and the pulmonary condition the Lorrain Smith effect, after the researchers who pioneered the discoveries and descriptions in the late 19th century. Oxygen toxicity is a concern for underwater divers, those on high concentrations of supplemental oxygen, and those undergoing hyperbaric oxygen therapy.

Infantile respiratory distress syndrome (IRDS), also called respiratory distress syndrome of newborn, or increasingly surfactant deficiency disorder (SDD), and previously called hyaline membrane disease (HMD), is a syndrome in premature infants caused by developmental insufficiency of pulmonary surfactant production and structural immaturity in the lungs. It can also be a consequence of neonatal infection and can result from a genetic problem with the production of surfactant-associated proteins.

Liquid breathing is a form of respiration in which a normally air-breathing organism breathes an oxygen-rich liquid (such as a perfluorocarbon), rather than breathing air, by selecting a liquid that can hold a large amount of oxygen and is capable of CO2 gas exchange.
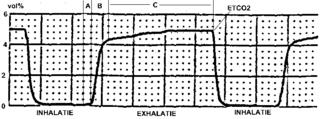
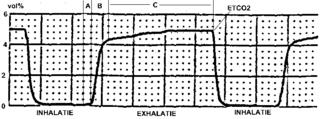
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide (CO
2) in the respiratory gases. Its main development has been as a monitoring tool for use during anesthesia and intensive care. It is usually presented as a graph of CO
2 (measured in kilopascals, "kPa" or millimeters of mercury, "mmHg") plotted against time, or, less commonly, but more usefully, expired volume (known as volumetric capnography). The plot may also show the inspired CO
2, which is of interest when rebreathing systems are being used. When the measurement is taken at the end of a breath (exhaling), it is called "end tidal" CO
2 (PETCO2).

Neonatology is a subspecialty of pediatrics that consists of the medical care of newborn infants, especially the ill or premature newborn. It is a hospital-based specialty and is usually practised in neonatal intensive care units (NICUs). The principal patients of neonatologists are newborn infants who are ill or require special medical care due to prematurity, low birth weight, intrauterine growth restriction, congenital malformations, sepsis, pulmonary hypoplasia, or birth asphyxia.

A neonatal intensive care unit (NICU), also known as an intensive care nursery (ICN), is an intensive care unit (ICU) specializing in the care of ill or premature newborn infants. The NICU is divided into several areas, including a critical care area for babies who require close monitoring and intervention, an intermediate care area for infants who are stable but still require specialized care, and a step down unit where babies who are ready to leave the hospital can receive additional care before being discharged.
Pulmonary hemorrhage is an acute bleeding from the lung, from the upper respiratory tract and the trachea, and the pulmonary alveoli. When evident clinically, the condition is usually massive. The onset of pulmonary hemorrhage is characterized by a cough productive of blood (hemoptysis) and worsening of oxygenation leading to cyanosis. Treatment should be immediate and should include tracheal suction, oxygen, positive pressure ventilation, and correction of underlying abnormalities such as disorders of coagulation. A blood transfusion may be necessary.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.

Bronchopulmonary dysplasia is a chronic lung disease in which premature infants, usually those who were treated with supplemental oxygen, require long-term oxygen. The alveoli that are present tend to not be mature enough to function normally. It is more common in infants with low birth weight (LBW) and those who receive prolonged mechanical ventilation to treat respiratory distress syndrome (RDS). It results in significant morbidity and mortality. The definition of BPD has continued to evolve primarily due to changes in the population, such as more survivors at earlier gestational ages, and improved neonatal management including surfactant, antenatal glucocorticoid therapy, and less aggressive mechanical ventilation.
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
Apnea of prematurity is defined as cessation of breathing by a premature infant that lasts for more than 20 seconds and/or is accompanied by hypoxia or bradycardia. Apnea is traditionally classified as either obstructive, central, or mixed. Obstructive apnea may occur when the infant's neck is hyperflexed or conversely, hyperextended. It may also occur due to low pharyngeal muscle tone or to inflammation of the soft tissues, which can block the flow of air though the pharynx and vocal cords. Central apnea occurs when there is a lack of respiratory effort. This may result from central nervous system immaturity, or from the effects of medications or illness. Many episodes of apnea of prematurity may start as either obstructive or central, but then involve elements of both, becoming mixed in nature.
Wilson–Mikity syndrome, a form of chronic lung disease (CLD) that exists only in premature infants, leads to progressive or immediate development of respiratory distress. This rare condition affects low birth babies and is characterized by rapid development of lung emphysema after birth, requiring prolonged ventilation and oxygen supplementation. It is closely related to bronchopulmonary dysplasia (BPD), differing mainly in the lack of prior ventilatory support. All the initial patients described with Wilson–Mikity syndrome were very low birth weight infants that had no history of mechanical ventilation, yet developed a syndrome that clinically resembled BPD. Upon the death of some of these infants, autopsies showed histologic changes similar to those seen in BPD.

Pneumopericardium is a medical condition where air enters the pericardial cavity. This condition has been recognized in preterm neonates, in which it is associated with severe lung pathology, after vigorous resuscitation, or in the presence of assisted ventilation. This is a serious complication, which if untreated may lead to cardiac tamponade and death. Pneumomediastinum, which is the presence of air in the mediastinum, may mimic and also coexist with pneumopericardium.
Ventilator-associated lung injury (VALI) is an acute lung injury that develops during mechanical ventilation and is termed ventilator-induced lung injury (VILI) if it can be proven that the mechanical ventilation caused the acute lung injury. In contrast, ventilator-associated lung injury (VALI) exists if the cause cannot be proven. VALI is the appropriate term in most situations because it is virtually impossible to prove what actually caused the lung injury in the hospital.

Subcutaneous emphysema occurs when gas or air accumulates and seeps under the skin, where normally no gas should be present. Subcutaneous refers to the subcutaneous tissue, and emphysema refers to trapped air pockets. Since the air generally comes from the chest cavity, subcutaneous emphysema usually occurs around the upper torso, such as on the chest, neck, face, axillae and arms, where it is able to travel with little resistance along the loose connective tissue within the superficial fascia. Subcutaneous emphysema has a characteristic crackling-feel to the touch, a sensation that has been described as similar to touching warm Rice Krispies. This sensation of air under the skin is known as subcutaneous crepitation, a form of crepitus.
Alveolar capillary dysplasia (ACD) is a rare, congenital diffuse lung disease characterized by abnormal blood vessels in the lungs that cause highly elevated pulmonary blood pressure and an inability to effectively oxygenate and remove carbon dioxide from the blood. ACD typically presents in newborn babies within hours of birth as rapid and labored breathing, blue-colored lips or skin, quickly leading to respiratory failure and death. Atypical forms of ACD have been reported with initially milder symptoms and survival of many months before the onset of respiratory failure or lung transplantation.

Emphysema is any air-filled enlargement in the body's tissues. Most commonly emphysema refers to the enlargement of air spaces (alveoli) in the lungs, and is also known as pulmonary emphysema.

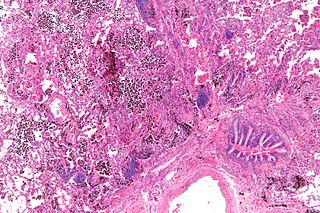
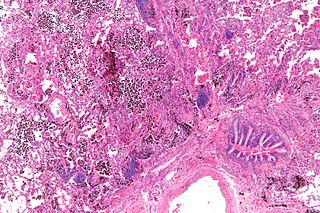
Smoking-related interstitial fibrosis (SRIF) is an abnormality in the lungs characterized by excessive collagen deposition within the walls of the air sacs. This abnormality can be seen with a microscope and diagnosed by pathologists. It is caused by cigarette smoking.