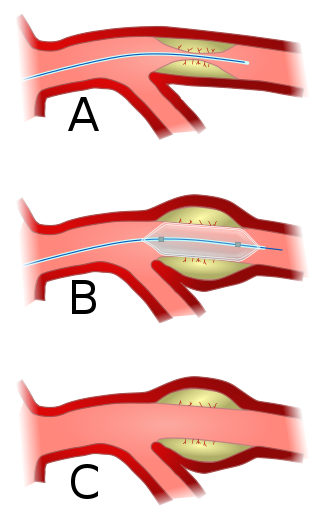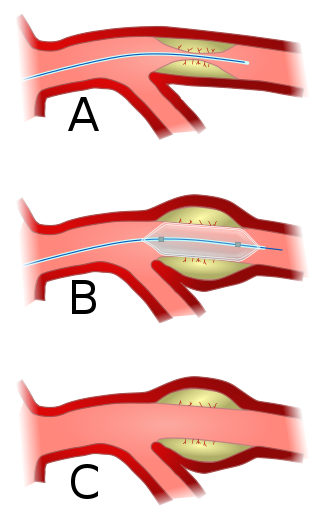
Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. A deflated balloon attached to a catheter is passed over a guide-wire into the narrowed vessel and then inflated to a fixed size. The balloon forces expansion of the blood vessel and the surrounding muscular wall, allowing an improved blood flow. A stent may be inserted at the time of ballooning to ensure the vessel remains open, and the balloon is then deflated and withdrawn. Angioplasty has come to include all manner of vascular interventions that are typically performed percutaneously.

Coronary artery bypass surgery, also known as coronary artery bypass graft, is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic heart.

Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.

Interventional cardiology is a branch of cardiology that deals specifically with the catheter based treatment of structural heart diseases. Andreas Gruentzig is considered the father of interventional cardiology after the development of angioplasty by interventional radiologist Charles Dotter.

Coronary thrombosis is defined as the formation of a blood clot inside a blood vessel of the heart. This blood clot may then restrict blood flow within the heart, leading to heart tissue damage, or a myocardial infarction, also known as a heart attack.

Acute coronary syndrome (ACS) is a syndrome due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally located pressure-like chest pain, often radiating to the left shoulder or angle of the jaw, and associated with nausea and sweating. Many people with acute coronary syndromes present with symptoms other than chest pain, particularly women, older people, and people with diabetes mellitus.

Percutaneous coronary intervention (PCI) is a minimally invasive non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The procedure is used to place and deploy coronary stents, a permanent wire-meshed tube, to open narrowed coronary arteries. PCI is considered 'non-surgical' as it uses a small hole in a peripheral artery (leg/arm) to gain access to the arterial system, an equivalent surgical procedure would involve the opening of the chest wall to gain access to the heart area. The term 'coronary angioplasty with stent' is synonymous with PCI. The procedure visualises the blood vessels via fluoroscopic imaging and contrast dyes. PCI is performed by an interventional cardiologists in a catheterization laboratory setting.
The intra-aortic balloon pump (IABP) is a mechanical device that increases myocardial oxygen perfusion and indirectly increases cardiac output through afterload reduction. It consists of a cylindrical polyurethane balloon that sits in the aorta, approximately 2 centimeters (0.79 in) from the left subclavian artery. The balloon inflates and deflates via counter pulsation, meaning it actively deflates in systole and inflates in diastole. Systolic deflation decreases afterload through a vacuum effect and indirectly increases forward flow from the heart. Diastolic inflation increases blood flow to the coronary arteries via retrograde flow. These actions combine to decrease myocardial oxygen demand and increase myocardial oxygen supply.

A drug-eluting stent (DES) is a thin tube that is used to treat narrowed arteries in medical procedures. It releases drugs to prevent the growth of scar tissue and reduce the risk of stent restenosis, which is the narrowing of the stented area of an artery after treatment. A drug-eluting stent is different from other types of stents because it has a coating that delivers medication directly to the arterial wall. A DES is often made of metal alloys and can be inserted into blocked or narrowed arteries through a catheter placed in a peripheral artery, such as in the arm or leg. DES is fully integrated with a catheter delivery system and is viewed as one integrated medical device.

Bivalirudin (Bivalitroban), sold under the brand names Angiomax and Angiox and manufactured by The Medicines Company, is a specific and reversible direct thrombin inhibitor (DTI).

Myocardial rupture is a laceration of the ventricles or atria of the heart, of the interatrial or interventricular septum, or of the papillary muscles. It is most commonly seen as a serious sequela of an acute myocardial infarction.
Door-to-balloon is a time measurement in emergency cardiac care (ECC), specifically in the treatment of ST segment elevation myocardial infarction. The interval starts with the patient's arrival in the emergency department, and ends when a catheter guidewire crosses the culprit lesion in the cardiac cath lab. Because of the adage that "time is muscle", meaning that delays in treating a myocardial infarction increase the likelihood and amount of cardiac muscle damage due to localised hypoxia, ACC/AHA guidelines recommend a door-to-balloon interval of no more than 90 minutes. As of 2006 in the United States, fewer than half of STEMI patients received reperfusion with primary percutaneous coronary intervention (PCI) within the guideline-recommended timeframe. It has become a core quality measure for the Joint Commission on Accreditation of Healthcare Organizations (TJC).
The history of invasive and interventional cardiology is complex, with multiple groups working independently on similar technologies. Invasive and interventional cardiology is currently closely associated with cardiologists, though the development and most of its early research and procedures were performed by diagnostic and interventional radiologists.

A coronary stent is a tube-shaped device placed in the coronary arteries that supply blood to the heart, to keep the arteries open in patients suffering from coronary heart disease. The vast majority of stents used in modern interventional cardiology are drug-eluting stents (DES) It is used in a medical procedure called percutaneous coronary intervention (PCI). Coronary stents are divided into two broad types - drug-eluting and bare metal stents, as of 2023 drug-eluting stents were used in more than 90% of all PCI procedures. Stents reduce angina and have been shown to improve survival and decrease adverse events after a patient has suffered a heart attack - medically termed an acute myocardial infarction.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops in one of the coronary arteries of the heart, causing infarction to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat, feeling tired, and decreased level of consciousness. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.
Myocardial infarction complications may occur immediately following a heart attack, or may need time to develop. After an infarction, an obvious complication is a second infarction, which may occur in the domain of another atherosclerotic coronary artery, or in the same zone if there are any live cells left in the infarct.

Management of acute coronary syndrome is targeted against the effects of reduced blood flow to the affected area of the heart muscle, usually because of a blood clot in one of the coronary arteries, the vessels that supply oxygenated blood to the myocardium. This is achieved with urgent hospitalization and medical therapy, including drugs that relieve chest pain and reduce the size of the infarct, and drugs that inhibit clot formation; for a subset of patients invasive measures are also employed. Basic principles of management are the same for all types of acute coronary syndrome. However, some important aspects of treatment depend on the presence or absence of elevation of the ST segment on the electrocardiogram, which classifies cases upon presentation to either ST segment elevation myocardial infarction (STEMI) or non-ST elevation acute coronary syndrome (NST-ACS); the latter includes unstable angina and non-ST elevation myocardial infarction (NSTEMI). Treatment is generally more aggressive for STEMI patients, and reperfusion therapy is more often reserved for them. Long-term therapy is necessary for prevention of recurrent events and complications.
Prof. Aly Saad, is a professor of cardiology at Zagazig University and a Member of higher committee of promotion of professors and Assistant professors of cardiovascular diseases and Critical care Subspecialty in Egypt.
Remote ischemic conditioning (RIC) is an experimental medical procedure that aims to reduce the severity of ischaemic injury to an organ such as the heart or the brain, most commonly in the situation of a heart attack or a stroke, or during procedures such as heart surgery when the heart may temporary suffer ischaemia during the operation, by triggering the body's natural protection against tissue injury. Although noted to have some benefits in experimental models in animals, this is still an experimental procedure in humans and initial evidence from small studies have not been replicated in larger clinical trials. Successive clinical trials have failed to identify evidence supporting a protective role in humans.
Alfredo E. Rodríguez is an Argentine interventional cardiologist, clinical researcher, and author. He is the Chief of Interventional Cardiology Service at Otamendi Hospital and Director and Founder of the Cardiovascular Research Center (CECI) a non -profit Research Organization in Buenos Aires Argentina.