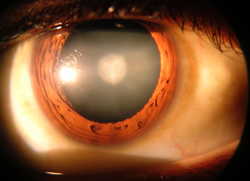
Keratoconus (KC) is a disorder of the eye that results in progressive thinning of the cornea. This may result in blurry vision, double vision, nearsightedness, irregular astigmatism, and light sensitivity leading to poor quality-of-life. Usually both eyes are affected. In more severe cases a scarring or a circle may be seen within the cornea.

Scanning laser ophthalmoscopy (SLO) is a method of examination of the eye. It uses the technique of confocal laser scanning microscopy for diagnostic imaging of the retina or cornea of the human eye.
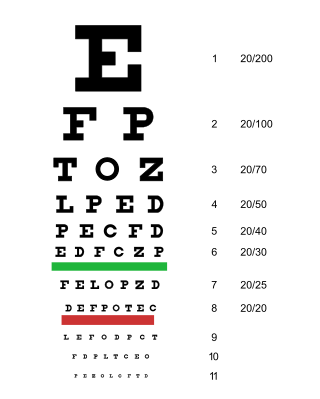
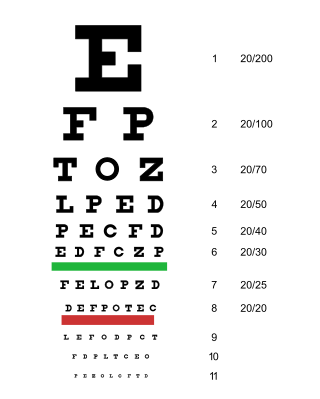
An eye examination is a series of tests performed to assess vision and ability to focus on and discern objects. It also includes other tests and examinations pertaining to the eyes. Eye examinations are primarily performed by an optometrist, ophthalmologist, or an orthoptist. Health care professionals often recommend that all people should have periodic and thorough eye examinations as part of routine primary care, especially since many eye diseases are asymptomatic.

Fuchs dystrophy, also referred to as Fuchs endothelial corneal dystrophy (FECD) and Fuchs endothelial dystrophy (FED), is a slowly progressing corneal dystrophy that usually affects both eyes and is slightly more common in women than in men. Although early signs of Fuchs dystrophy are sometimes seen in people in their 30s and 40s, the disease rarely affects vision until people reach their 50s and 60s.
Eye banks recover, prepare and deliver donated eyes for cornea transplants and research. The first successful cornea transplant was performed in 1905 and the first eye bank was founded in 1944. Currently, in the United States, eye banks provide tissue for over 80,000 cornea transplants each year to treat conditions such as keratoconus and corneal scarring. In some cases, the white of the eye (sclera) is used to surgically repair recipient eyes. Unlike other organs and tissues, corneas are in adequate supply for transplants in the United States, and excess tissue is exported internationally, where there are shortages in many countries, due to greater demand and a less-developed eye banking infrastructure.

In ophthalmology, gonioscopy is a routine procedure that measures the angle between the iris and the cornea, using a goniolens together with a slit lamp or operating microscope. Its use is important in diagnosing and monitoring various eye conditions associated with glaucoma.

Corneal topography, also known as photokeratoscopy or videokeratography, is a non-invasive medical imaging technique for mapping the anterior curvature of the cornea, the outer structure of the eye. Since the cornea is normally responsible for some 70% of the eye's refractive power, its topography is of critical importance in determining the quality of vision and corneal health.

Corneal ulcer, also called keratitis, is an inflammatory or, more seriously, infective condition of the cornea involving disruption of its epithelial layer with involvement of the corneal stroma. It is a common condition in humans particularly in the tropics and in farming. In developing countries, children afflicted by vitamin A deficiency are at high risk for corneal ulcer and may become blind in both eyes persisting throughout life. In ophthalmology, a corneal ulcer usually refers to having an infection, while the term corneal abrasion refers more to a scratch injury.
Scanning laser polarimetry is the use of polarised light to measure the thickness of the retinal nerve fiber layer (RNFL) as part of a glaucoma workup. The GDx-VCC is one example.

Fundus photography involves photographing the rear of an eye, also known as the fundus. Specialized fundus cameras consisting of an intricate microscope attached to a flash enabled camera are used in fundus photography. The main structures that can be visualized on a fundus photo are the central and peripheral retina, optic disc and macula. Fundus photography can be performed with colored filters, or with specialized dyes including fluorescein and indocyanine green.
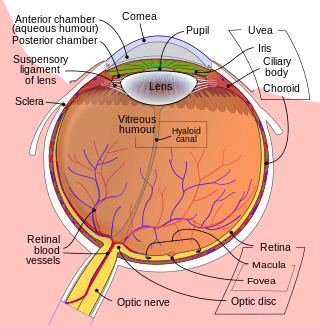
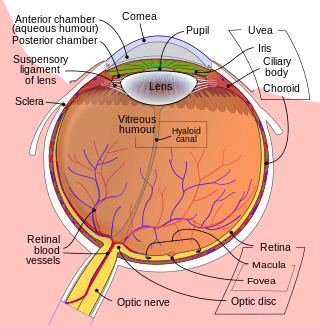
Intraocular hemorrhage is bleeding inside the eye. Bleeding can occur from any structure of the eye where there is vasculature or blood flow, including the anterior chamber, vitreous cavity, retina, choroid, suprachoroidal space, or optic disc.

The stereo, stereoscopic or dissecting microscope is an optical microscope variant designed for low magnification observation of a sample, typically using light reflected from the surface of an object rather than transmitted through it. The instrument uses two separate optical paths with two objectives and eyepieces to provide slightly different viewing angles to the left and right eyes. This arrangement produces a three-dimensional visualization of the sample being examined. Stereomicroscopy overlaps macrophotography for recording and examining solid samples with complex surface topography, where a three-dimensional view is needed for analyzing the detail.

Meesmann corneal dystrophy (MECD) is a rare hereditary autosomal dominant disease that is characterized as a type of corneal dystrophy and a keratin disease. MECD is characterized by the formation of microcysts in the outermost layer of the cornea, known as the anterior corneal epithelium. The anterior corneal epithelium also becomes fragile. This usually affects both eyes rather than a single eye and worsens over time. There are two phenotypes, Meesmann corneal dystrophy 1 (MECD1) and Meesmann corneal dystrophy 2 (MECD2), which affect the genes KRT3 and KRT12, respectively. A heterozygous mutation in either of these genes will lead to a single phenotype. Many with Meesmann corneal dystrophy are asymptomatic or experience mild symptoms.

Keratoprosthesis is a surgical procedure where a diseased cornea is replaced with an artificial cornea. Traditionally, keratoprosthesis is recommended after a person has had a failure of one or more donor corneal transplants. More recently, a less invasive, non-penetrating artificial cornea has been developed which can be used in more routine cases of corneal blindness. While conventional cornea transplant uses donor tissue for transplant, an artificial cornea is used in the keratoprosthesis procedure. The surgery is performed to restore vision in patients with severely damaged cornea due to congenital birth defects, infections, injuries and burns.

OCT Biomicroscopy is the use of optical coherence tomography (OCT) in place of slit lamp biomicroscopy to examine the transparent axial tissues of the eye. Traditionally, ophthalmic biomicroscopy has been completed with a slit lamp biomicroscope that uses slit beam illumination and an optical microscope to enable stereoscopic, magnified, cross-sectional views of transparent tissues in the eye, with or without the aid of an additional lens. Like slit lamp biomicroscopy, OCT does not penetrate opaque tissues well but enables detailed, cross-sectional views of transparent tissues, often with greater detail than is possible with a slit lamp. Ultrasound biomicroscopy (UBM) is much better at imaging through opaque tissues since it uses high energy sound waves. Because of its limited depth of penetration, UBM's main use within ophthalmology has been to visualize anterior structures such as the angle and ciliary body. Both ultrasound and OCT biomicroscopy produce an objective image of ocular tissues from which measurements can be made. Unlike UBM, OCT biomicroscopy can image tissues with high axial resolution as far posteriorly as the choroid.

Gholam A. Peyman is an Iranian American ophthalmologist, retina surgeon, and inventor. He is best known for his invention of LASIK eye surgery, a vision correction procedure designed to allow people to see clearly without glasses. He was awarded the first US patent for the procedure in 1989.
The aim of an accurate intraocular lens power calculation is to provide an intraocular lens (IOL) that fits the specific needs and desires of the individual patient. The development of better instrumentation for measuring the eye's axial length (AL) and the use of more precise mathematical formulas to perform the appropriate calculations have significantly improved the accuracy with which the surgeon determines the IOL power.
The Van Herick technique is an eye examination method used to determine the size of the anterior chamber angle of the eye.

A corneal button is a replacement cornea to be transplanted in the place of a damaged, diseased or opacified cornea, normally approximately 8.5–9.0mm in diameter. It is used in a corneal transplantation procedure whereby the whole, or part, of a cornea is replaced. The donor tissue can now be held for days to even weeks of the donor's death and is normally a small, rounded shape. The main use of the corneal button is during procedures where the entirety of the cornea needs to be replaced, also known as penetrating keratoplasty.

The Heidelberg Retinal Tomography is a diagnostic procedure used in ophthalmology. The Heidelberg Retina Tomograph (HRT) is an ophthalmological confocal point scanning laser ophthalmoscope for examining the cornea and certain areas of the retina using different diagnostic modules. However, the most widely used area of application for HRT is the inspection of the optic nerve head (papilla) for early detection and follow-up of glaucoma. The procedure has established itself as an integral part of routine glaucoma diagnostics alongside the visual field examination (perimetry), the chamber angle examination (gonioscopy) and the measurement of intraocular pressure (tonometry). The HRT is the most widely used application of confocal scanning laser ophthalmoscopy.