Related Research Articles

The limbic system, also known as the paleomammalian cortex, is a set of brain structures located on both sides of the thalamus, immediately beneath the medial temporal lobe of the cerebrum primarily in the forebrain.
Capgras delusion or Capgras syndrome is a psychiatric disorder in which a person holds a delusion that a friend, spouse, parent, another close family member, or pet has been replaced by an identical impostor. It is named after Joseph Capgras (1873–1950), the French psychiatrist who first described the disorder.

A phantom limb is the sensation that an amputated or missing limb is still attached. Approximately 80–100% of individuals with an amputation experience sensations in their amputated limb. However, only a small percentage will experience painful phantom limb sensation. These sensations are relatively common in amputees and usually resolve within two to three years without treatment. Research continues to explore the underlying mechanisms of phantom limb pain (PLP) and effective treatment options.

Vilayanur Subramanian Ramachandran is an Indian-American neuroscientist. He is known for his wide-ranging experiments and theories in behavioral neurology, including the invention of the mirror box. Ramachandran is a distinguished professor in UCSD's Department of Psychology, where he is the director of the Center for Brain and Cognition.
Anosognosia is a condition in which a person with a disability is cognitively unaware of having it due to an underlying physical condition. Anosognosia results from physiological damage to brain structures, typically to the parietal lobe or a diffuse lesion on the fronto-temporal-parietal area in the right hemisphere, and is thus a neuropsychiatric disorder. A deficit of self-awareness, it was first named by the neurologist Joseph Babinski in 1914.

Hemispatial neglect is a neuropsychological condition in which, after damage to one hemisphere of the brain, a deficit in attention and awareness towards the side of space opposite brain damage is observed. It is defined by the inability of a person to process and perceive stimuli towards the contralesional side of the body or environment. Hemispatial neglect is very commonly contralateral to the damaged hemisphere, but instances of ipsilesional neglect have been reported.
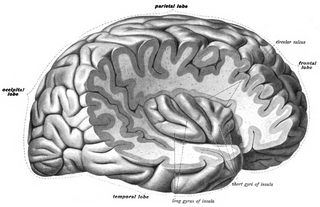
The insular cortex is a portion of the cerebral cortex folded deep within the lateral sulcus within each hemisphere of the mammalian brain.
The pedunculopontine nucleus (PPN) or pedunculopontine tegmental nucleus is a collection of neurons located in the upper pons in the brainstem. It lies caudal to the substantia nigra and adjacent to the superior cerebellar peduncle. It has two divisions of subnuclei; the pars compacta containing mainly cholinergic neurons, and the pars dissipata containing mainly glutamatergic neurons and some non-cholinergic neurons. The pedunculopontine nucleus is one of the main components of the reticular activating system. It was first described in 1909 by Louis Jacobsohn-Lask, a German neuroanatomist.
Reduplicative paramnesia is the delusional belief that a place or location has been duplicated, existing in two or more places simultaneously, or that it has been 'relocated' to another site. It is one of the delusional misidentification syndromes; although rare, it is most commonly associated with acquired brain injury, particularly simultaneous damage to the right cerebral hemisphere and to both frontal lobes.
Pseudoathetosis is abnormal writhing movements, usually of the fingers, caused by a failure of joint position sense (proprioception) and indicates disruption of the proprioceptive pathway, from nerve to parietal cortex.
Monoplegia is paralysis of a single limb, usually an arm. Common symptoms associated with monoplegic patients are weakness, numbness, and pain in the affected limb. Monoplegia is a type of paralysis that falls under hemiplegia. While hemiplegia is paralysis of half of the body, monoplegia is localized to a single limb or to a specific region of the body. Monoplegia of the upper limb is sometimes referred to as brachial monoplegia, and that of the lower limb is called crural monoplegia. Monoplegia in the lower extremities is not as common of an occurrence as in the upper extremities. Monoparesis is a similar, but less severe, condition because one limb is very weak, not paralyzed. For more information, see paresis.
Mirrored-self misidentification is the delusional belief that one's reflection in the mirror is another person – typically a younger or second version of one's self, a stranger, or a relative. This delusion occurs most frequently in patients with dementia and an affected patient maintains the ability to recognize others' reflections in the mirror. It is caused by right hemisphere cranial dysfunction that results from traumatic brain injury, stroke, or general neurological illness. It is an example of a monothematic delusion, a condition in which all abnormal beliefs have one common theme, as opposed to a polythematic delusion, in which a variety of unrelated delusional beliefs exist. This delusion is also classified as one of the delusional misidentification syndromes (DMS). A patient with a DMS condition consistently misidentifies places, objects, persons, or events. DMS patients are not aware of their psychological condition, are resistant to correction and their conditions are associated with brain disease – particularly right hemisphere brain damage and dysfunction.
A monothematic delusion is a delusional state that concerns only one particular topic. This is contrasted by what is sometimes called multi-thematic or polythematic delusions where the person has a range of delusions. These disorders can occur within the context of schizophrenia or dementia or they can occur without any other signs of mental illness. When these disorders are found outside the context of mental illness, they are often caused by organic dysfunction as a result of traumatic brain injury, stroke, or neurological illness.

Foix–Chavany–Marie Syndrome (FCMS), also known as bilateral opercular syndrome, is a neuropathological disorder characterized by paralysis of the facial, tongue, pharynx, and masticatory muscles of the mouth that aid in chewing. The disorder is primarily caused by thrombotic and embolic strokes, which cause a deficiency of oxygen in the brain. As a result, bilateral lesions may form in the junctions between the frontal lobe and temporal lobe, the parietal lobe and cortical lobe, or the subcortical region of the brain. FCMS may also arise from defects existing at birth that may be inherited or nonhereditary. Symptoms of FCMS can be present in a person of any age and it is diagnosed using automatic-voluntary dissociation assessment, psycholinguistic testing, neuropsychological testing, and brain scanning. Treatment for FCMS depends on the onset, as well as on the severity of symptoms, and it involves a multidisciplinary approach.
Todd's paresis is focal weakness in a part or all of the body after a seizure. This weakness typically affects the limbs and is localized to either the left or right side of the body. It usually subsides completely within 48 hours. Todd's paresis may also affect speech, eye position (gaze), or vision.
Ideomotor Apraxia, often IMA, is a neurological disorder characterized by the inability to correctly imitate hand gestures and voluntarily mime tool use, e.g. pretend to brush one's hair. The ability to spontaneously use tools, such as brushing one's hair in the morning without being instructed to do so, may remain intact, but is often lost. The general concept of apraxia and the classification of ideomotor apraxia were developed in Germany in the late 19th and early 20th centuries by the work of Hugo Liepmann, Adolph Kussmaul, Arnold Pick, Paul Flechsig, Hermann Munk, Carl Nothnagel, Theodor Meynert, and linguist Heymann Steinthal, among others. Ideomotor apraxia was classified as "ideo-kinetic apraxia" by Liepmann due to the apparent dissociation of the idea of the action with its execution. The classifications of the various subtypes are not well defined at present, however, owing to issues of diagnosis and pathophysiology. Ideomotor apraxia is hypothesized to result from a disruption of the system that relates stored tool use and gesture information with the state of the body to produce the proper motor output. This system is thought to be related to the areas of the brain most often seen to be damaged when ideomotor apraxia is present: the left parietal lobe and the premotor cortex. Little can be done at present to reverse the motor deficit seen in ideomotor apraxia, although the extent of dysfunction it induces is not entirely clear.
Body schema is an organism's internal model of its own body, including the position of its limbs. The neurologist Sir Henry Head originally defined it as a postural model of the body that actively organizes and modifies 'the impressions produced by incoming sensory impulses in such a way that the final sensation of body position, or of locality, rises into consciousness charged with a relation to something that has happened before'. As a postural model that keeps track of limb position, it plays an important role in control of action.
Asomatognosia is a neurological disorder characterized as loss of recognition or awareness of part of the body. The failure to acknowledge, for example, a limb, may be expressed verbally or as a pattern of neglect. The limb may also be attributed to another person, a delusion known as somatoparaphrenia. However, they can be shown their limb and this error is temporarily corrected. Some authors have focused on the prevalence of hemispatial neglect in such patients.
Corticobasal syndrome (CBS) is a rare, progressive atypical Parkinsonism syndrome and is a tauopathy related to frontotemporal dementia. CBS is typically caused by the deposit of tau proteins forming in different areas of the brain.

Olaf Blanke is a Swiss and German physician, neurologist and neuroscientist. He holds the Bertarelli Foundation Chair in Cognitive Neuroprosthetics at the École Polytechnique Fédérale de Lausanne (EPFL). He directs the Laboratory of Cognitive Neuroscience at the Brain Mind Institute of EPFL and is professor of Neurology at Geneva University Hospitals. Blanke is known for his research on the neurological bases of self-consciousness and out-of-body experiences.
References
- 1 2 3 Feinberg T.; Venneri A.; Simone A.M.; et al. (2010). "The neuroanatomy of asomatognosia and somatoparaphrenia". Journal of Neurology, Neurosurgery & Psychiatry. 81 (3): 276–281. doi:10.1136/jnnp.2009.188946. PMID 19778911. S2CID 4931879.
- ↑ Bottini G.; Bisiach E.; Sterzi R.; Vallar G. (2002). "Feeling touches in someone else's hand". NeuroReport. 13 (2): 249–252. doi:10.1097/00001756-200202110-00015. PMID 11893919. S2CID 32287566.
- ↑ Vallar G., Ronchi R. (2009). "Somatoparaphrenia: a body delusion. A review of the neuropsychological literature". Experimental Brain Research. 192 (3): 533–551. doi:10.1007/s00221-008-1562-y. PMID 18813916. S2CID 206924931.
- ↑ Coltheart M (2005). "Delusional belief". Australian Journal of Psychology. 57 (2): 72. doi:10.1080/00049530500125082.
- ↑ Vallar G., Ronchi R. (2009). "Somatoparaphrenia: A body delusion. A review of the neuropsychological literature". Experimental Brain Research. 192 (3): 533–51. doi:10.1007/s00221-008-1562-y. PMID 18813916. S2CID 206924931.
- ↑ Invernizzi P, Gandola M, Romano D, Zapparoli L, Bottini G, Paulesu E (2013). "What is mine? Behavioral and anatomical dissociations between somatoparaphrenia and anosognosia for hemiplegia". Behav Neurol. 26 (1–2): 139–50. doi: 10.1155/2013/548467 . PMC 5213125 . PMID 22713395.
- 1 2 Ronchi, Roberta; Park, Hyeong-Dong; Blanke, Olaf (2018-01-01), Vallar, Giuseppe; Coslett, H. Branch (eds.), "Chapter 15 - Bodily self-consciousness and its disorders", Handbook of Clinical Neurology, The Parietal Lobe, Elsevier, vol. 151, pp. 313–330, retrieved 2024-01-28
- ↑ Fotopoulou, Aikaterini; Jenkinson, Paul Mark; Tsakiris, Manos; Haggard, Patrick; Rudd, Antony; Kopelman, Michael D. (December 2011). "Mirror-view reverses somatoparaphrenia: dissociation between first- and third-person perspectives on body ownership". Neuropsychologia. 49 (14): 3946–3955. doi:10.1016/j.neuropsychologia.2011.10.011. ISSN 1873-3514. PMID 22023911.
- ↑ Feinberg T. E.; Haber L. D.; Leeds N.E. (1990). "Verbal asomatognosia". Neurology. 40 (9): 1391–1394. doi:10.1212/wnl.40.9.1391. PMID 2392224. S2CID 35409449.
- ↑ Feinberg T. E.; Roane D. M.; Ali J. (2000). "Illusory limb movements in anosognosia for hemiplegia". J Neurol Neurosurg Psychiatry. 68 (4): 511–513. doi:10.1136/jnnp.68.4.511. PMC 1736869 . PMID 10727491.
- ↑ Cereda C.; Ghika J.; Maeder P.; Bogousslavsky J. (2002). "Strokes restricted to the insular cortex". Neurology. 59 (12): 1950–1955. doi:10.1212/01.wnl.0000038905.75660.bd. PMID 12499489. S2CID 22115202.
- ↑ Healton E. B.; Navarro C.; Bressman S.; Brust J. C. (1982). "Subcortical neglect". Neurology. 32 (7): 776–778. doi:10.1212/wnl.32.7.776. PMID 7201116. S2CID 219207359.
- 1 2 Gandola M, Invernizzi P, Sedda A, Ferré ER, Sterzi R, Sberna M, Paulesu E, Bottini G (Oct 2012). "An anatomical account of somatoparaphrenia". Cortex. 48 (9): 1165–78. doi:10.1016/j.cortex.2011.06.012. PMID 21774922. S2CID 37732776.
- ↑ Fotopoulou A., Jenkinson P.M., Tsakiris M., Haggard P., Rudd A., Kopelman M.D. (2011). "Mirror-view reverses somatopharaphrenia: Dissociation between first- and third-person perspectives on body ownership". Neuropsychologia. 49 (14): 3946–3955. doi:10.1016/j.neuropsychologia.2011.10.011. PMID 22023911. S2CID 25892919.
{{cite journal}}: CS1 maint: multiple names: authors list (link)