Related Research Articles

An antacid is a substance which neutralizes stomach acidity and is used to relieve heartburn, indigestion or an upset stomach. Some antacids have been used in the treatment of constipation and diarrhea. Marketed antacids contain salts of aluminium, calcium, magnesium, or sodium. Some preparations contain a combination of two salts, such as magnesium carbonate and aluminium hydroxide.
An antiplatelet drug (antiaggregant), also known as a platelet agglutination inhibitor or platelet aggregation inhibitor, is a member of a class of pharmaceuticals that decrease platelet aggregation and inhibit thrombus formation. They are effective in the arterial circulation where classical Vitamin K antagonist anticoagulants have minimal effect.
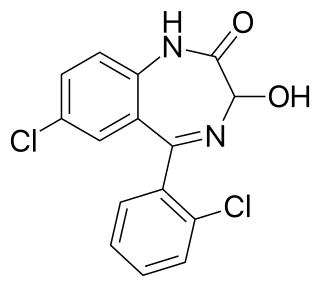
Lorazepam, sold under the brand name Ativan among others, is a benzodiazepine medication. It is used to treat anxiety disorders, trouble sleeping, severe agitation, active seizures including status epilepticus, alcohol withdrawal, and chemotherapy-induced nausea and vomiting. It is also used during surgery to interfere with memory formation and to sedate those who are being mechanically ventilated. It is also used, along with other treatments, for acute coronary syndrome due to cocaine use. It can be given by mouth or as an injection into a muscle or vein. When given by injection, onset of effects is between one and thirty minutes and effects last for up to a day.

Propofol, marketed as Diprivan, among other names, also known as 2,6-Diisopropylphenol, is a short-acting medication that results in a decreased level of consciousness and a lack of memory for events. Its uses include the induction and maintenance of general anesthesia, sedation for mechanically ventilated adults, and procedural sedation. It is also used for status epilepticus if other medications have not worked. It is given by injection into a vein, and the maximum effect takes about two minutes to occur and typically lasts five to ten minutes. Propofol is also used for euthanasia in Canada.
Dyslipidemia is an abnormal amount of lipids in the blood. Dyslipidemia is a risk factor for the development of atherosclerotic cardiovascular disease (ASCVD). ASCVD includes coronary artery disease, cerebrovascular disease, and peripheral artery disease. Although dyslipidemia is a risk factor for ASCVD, abnormal levels don't mean that lipid lowering agents need to be started. Other factors, such as comorbid conditions and lifestyle in addition to dyslipidemia, is considered in a cardiovascular risk assessment. In developed countries, most dyslipidemias are hyperlipidemias; that is, an elevation of lipids in the blood. This is often due to diet and lifestyle. Prolonged elevation of insulin resistance can also lead to dyslipidemia. Likewise, increased levels of O-GlcNAc transferase (OGT) may cause dyslipidemia.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke, heart failure, kidney failure and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21%, and can reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.
Postoperative nausea and vomiting (PONV) is the phenomenon of nausea, vomiting, or retching experienced by a patient in the postanesthesia care unit (PACU) or within 24 hours following a surgical procedure. PONV affects about 10% of the population undergoing general anaesthesia each year. PONV can be unpleasant and lead to a delay in mobilization and food, fluid, and medication intake following surgery.
Antipruritics, abirritants, or anti-itch drugs, are medications that inhibit the itching often associated with sunburns, allergic reactions, eczema, psoriasis, chickenpox, fungal infections, insect bites and stings like those from mosquitoes, fleas, and mites, and contact dermatitis and urticaria caused by plants such as poison ivy or stinging nettle. It can also be caused by chronic kidney disease and related conditions.
Drug interactions occur when a drug's mechanism of action is affected by the concomitant administration of substances such as foods, beverages, or other drugs. The cause is often inhibition of, or less effective action, of the specific receptors available to the drug. This influences drug molecules to bind to secondary targets, which may result in an array of unwanted side-effects.
An adverse effect is an undesired harmful effect resulting from a medication or other intervention, such as surgery. An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. The term complication is similar to adverse effect, but the latter is typically used in pharmacological contexts, or when the negative effect is expected or common. If the negative effect results from an unsuitable or incorrect dosage or procedure, this is called a medical error and not an adverse effect. Adverse effects are sometimes referred to as "iatrogenic" because they are generated by a physician/treatment. Some adverse effects occur only when starting, increasing or discontinuing a treatment. Adverse effects can also be caused by placebo treatments . Using a drug or other medical intervention which is contraindicated may increase the risk of adverse effects. Adverse effects may cause complications of a disease or procedure and negatively affect its prognosis. They may also lead to non-compliance with a treatment regimen. Adverse effects of medical treatment resulted in 142,000 deaths in 2013 up from 94,000 deaths in 1990 globally.

Anthracyclines are a class of drugs used in cancer chemotherapy that are extracted from Streptomyces bacterium. These compounds are used to treat many cancers, including leukemias, lymphomas, breast, stomach, uterine, ovarian, bladder cancer, and lung cancers. The first anthracycline discovered was daunorubicin, which is produced naturally by Streptomyces peucetius, a species of Actinomycetota. Clinically the most important anthracyclines are doxorubicin, daunorubicin, epirubicin and idarubicin.

Epirubicin is an anthracycline drug used for chemotherapy. It can be used in combination with other medications to treat breast cancer in patients who have had surgery to remove the tumor. It is marketed by Pfizer under the trade name Ellence in the US and Pharmorubicin or Epirubicin Ebewe elsewhere.

Dolasetron (trade name Anzemet) is a serotonin 5-HT3 receptor antagonist used to treat nausea and vomiting following chemotherapy. Its main effect is to reduce the activity of the vagus nerve, which is a nerve that activates the vomiting center in the medulla oblongata. It does not have much antiemetic effect when symptoms are due to motion sickness. This drug does not have any effect on dopamine receptors or muscarinic receptors.
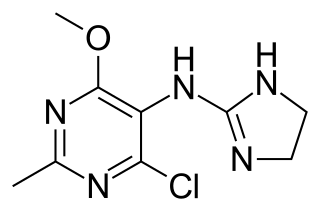
Moxonidine (INN) is a new-generation alpha-2/imidazoline receptor agonist antihypertensive drug licensed for the treatment of mild to moderate essential hypertension. It may have a role when thiazides, beta-blockers, ACE inhibitors, and calcium channel blockers are not appropriate or have failed to control blood pressure. In addition, it demonstrates favourable effects on parameters of the insulin resistance syndrome, apparently independent of blood pressure reduction. It is also a growth hormone releaser. It is manufactured by Solvay Pharmaceuticals under the brand name Physiotens & Moxon.

Acamprosate, sold under the brand name Campral, is a medication used along with counseling to treat alcohol use disorder.
Chemical antagonists impede the normal function of a system. They function to invert the effects of other molecules. The effects of antagonists can be seen after they have encountered an agonist, and as a result, the effects of the agonist is neutralized. Antagonists such as dopamine antagonist slow down movement in lab rats. Although they hinder the joining of enzymes to substrates, Antagonists can be beneficial. For example, not only do angiotensin receptor blockers, and angiotensin-converting enzyme (ACE) inhibitors work to lower blood pressure, but they also counter the effects of renal disease in diabetic and non-diabetic patients. Chelating agents, such as calcium di sodium defeated, fall into the category of antagonists and operate to minimize the lethal effects of heavy metals such as mercury or lead.

The sigma-2 receptor (σ2R) is a sigma receptor subtype that has attracted attention due to its involvement in diseases such as cancer and neurological diseases. It is currently under investigation for its potential diagnostic and therapeutic uses.

Pentylenetetrazol, also known as pentylenetetrazole, leptazol, metrazol, pentetrazol (INN), pentamethylenetetrazol, Corazol, Cardiazol, Deumacard, or PTZ, is a drug formerly used as a circulatory and respiratory stimulant. High doses cause convulsions, as discovered by Hungarian-American neurologist and psychiatrist Ladislas J. Meduna in 1934. It has been used in convulsive therapy, and was found to be effective—primarily for depression—but side effects such as uncontrolled seizures were difficult to avoid. In 1939, pentylenetetrazol was replaced by electroconvulsive therapy, which is easier to administer, as the preferred method for inducing seizures in England's mental hospitals. In the US, its approval by the Food and Drug Administration was revoked in 1982. It is used in Italy as a cardio-respiratory stimulant in combination with codeine in a cough suppressant drug.
A steroidogenesis inhibitor, also known as a steroid biosynthesis inhibitor, is a type of drug which inhibits one or more of the enzymes that are involved in the process of steroidogenesis, the biosynthesis of endogenous steroids and steroid hormones. They may inhibit the production of cholesterol and other sterols, sex steroids such as androgens, estrogens, and progestogens, corticosteroids such as glucocorticoids and mineralocorticoids, and neurosteroids. They are used in the treatment of a variety of medical conditions that depend on endogenous steroids.

An antiarthritic is any member of the group of drugs used to relieve or prevent arthritic symptoms, such as joint pain and joint stiffness. Depending on the antiarthritic drug class, it can be responsible for managing pain, reducing inflammation and/or acting as an immunosuppressant. These drugs are typically given orally, topically or through administration by injection. The choice of antiarthritic medication is often determined by the type/nature of arthritis, the severity of symptoms as well as other factors, such as the tolerability of side effects.
References
- ↑ Government of Canada, Canadian Centre for Occupational Health and Safety (2019). "Synergism and related terms : OSH Answers". www.ccohs.ca. Retrieved 2022-03-26.
- ↑ Rowland, M., & Tozer, T. (2011). Clinical pharmacokinetics and pharmacodynamics [electronic resource] : Concepts and applications (4th ed.). Philadelphia: Wolters Kluwer Health/Lippincott William & Wilkins.
- 1 2 3 4 Cascorbi, Ingolf (2012). "Drug interactions--principles, examples and clinical consequences". Deutsches Ärzteblatt International. 109 (33–34): 546–555, quiz 556. doi:10.3238/arztebl.2012.0546. ISSN 1866-0452. PMC 3444856 . PMID 23152742.
- ↑ Greco, W. R.; Bravo, G.; Parsons, J. C. (1995). "The search for synergy: a critical review from a response surface perspective". Pharmacological Reviews. 47 (2): 331–385. ISSN 0031-6997. PMID 7568331.
- ↑ Maton, P. N.; Burton, M. E. (1999). "Antacids revisited: a review of their clinical pharmacology and recommended therapeutic use". Drugs. 57 (6): 855–870. doi:10.2165/00003495-199957060-00003. ISSN 0012-6667. PMID 10400401. S2CID 46960343.
- ↑ Brohan, Janette; Goudra, Basavana G. (2017-10-01). "The Role of GABA Receptor Agonists in Anesthesia and Sedation". CNS Drugs. 31 (10): 845–856. doi:10.1007/s40263-017-0463-7. ISSN 1179-1934. PMID 29039138. S2CID 207486777.
- ↑ Sanna, E., Garau, F., & Harris, R. (1995). Novel properties of homomeric beta 1 gamma-aminobutyric acid type A receptors: Actions of the anesthetics propofol and pentobarbital. Molecular Pharmacology, 47(2), 213.
- ↑ Jones, M., Harrison, N., Pritchett, D., & Hales, T. (1995). Modulation of the GABAA receptor by propofol is independent of the gamma subunit. The Journal of Pharmacology and Experimental Therapeutics, 274(2), 962-968.
- ↑ Lam, Dennis W; Reynolds, James N (1998). "Modulatory and direct effects of propofol on recombinant GABAA receptors expressed in Xenopus oocytes: Influence of α- and γ2-subunits". Brain Research. 784 (1–2): 179–187. doi:10.1016/s0006-8993(97)01334-6. ISSN 0006-8993. PMID 9518600. S2CID 140204274.
- ↑ Garcia, Paul; Kolesky, Scott; Jenkins, Andrew (2010-03-01). "General Anesthetic Actions on GABAA Receptors". Current Neuropharmacology. 8 (1): 2–9. doi:10.2174/157015910790909502. ISSN 1570-159X. PMC 2866459 . PMID 20808541.
- ↑ Harris, R.; Lazar, O.; Johansen, J.; Sebel, P. (2006-06-01). "Interaction of Propofol and Sevoflurane on Loss of Consciousness and Movement to Skin Incision during General Anesthesia". Anesthesiology. 104 (6): 1170–1175. doi:10.1097/00000542-200606000-00011. ISSN 0003-3022. PMID 16732087. S2CID 7164486.
- ↑ Novaes, Rômulo Dias; Sartini, Marcus Vinicius Pessoa; Rodrigues, João Paulo Ferreira; Gonçalves, Reggiani Vilela; Santos, Eliziária Cardoso; Souza, Raquel Lopes Martins; Caldas, Ivo Santana (2016). "Curcumin Enhances the Anti-Trypanosoma cruzi Activity of Benznidazole-Based Chemotherapy in Acute Experimental Chagas Disease". Antimicrobial Agents and Chemotherapy. 60 (6): 3355–3364. doi:10.1128/AAC.00343-16. ISSN 0066-4804. PMC 4879395 . PMID 27001816.
- ↑ Allam, Gamal (2009). "Immunomodulatory effects of curcumin treatment on murine schistosomiasis mansoni". Immunobiology. 214 (8): 712–727. doi:10.1016/j.imbio.2008.11.017. PMID 19249123.
- ↑ Jagetia, Ganesh Chandra; Aggarwal, Bharat B. (2007-01-25). ""Spicing Up" of the Immune System by Curcumin". Journal of Clinical Immunology. 27 (1): 19–35. doi:10.1007/s10875-006-9066-7. ISSN 0271-9142. PMID 17211725. S2CID 21586221.
- ↑ Nandakumar, Dalavaikodihalli Nanjaiah; Nagaraj, Viswanathan Arun; Vathsala, Palakkod Govindan; Rangarajan, Pundi; Padmanaban, Govindarajan (2006). "Curcumin-Artemisinin Combination Therapy for Malaria". Antimicrobial Agents and Chemotherapy. 50 (5): 1859–1860. doi:10.1128/AAC.50.5.1859-1860.2006. ISSN 0066-4804. PMC 1472230 . PMID 16641461.
- ↑ Dang, Jingyi; Fu, Jun; Zhang, Zhao; Liu, Dong; Cheng, Debin; Fan, Hongbin (2021). "Comparison between trabectedin and doxorubicin in soft-tissue sarcomas: a systematic review and meta-analysis". Annals of Translational Medicine. 9 (24): 1764. doi: 10.21037/atm-21-6033 . ISSN 2305-5839. PMC 8756232 . PMID 35071458.
- ↑ Kellogg, G. E.; Scarsdale, J. N.; Fornari, F. A. (1998). "Identification and hydropathic characterization of structural features affecting sequence specificity for doxorubicin intercalation into DNA double-stranded polynucleotides". Nucleic Acids Research. 26 (20): 4721–4732. doi:10.1093/nar/26.20.4721. ISSN 0305-1048. PMC 147880 . PMID 9753742.
- ↑ Zewail-Foote, Maha; Li, Ven-Shun; Kohn, Harold; Bearss, David; Guzman, Mary; Hurley, Laurence H (2001). "The inefficiency of incisions of ecteinascidin 743–DNA adducts by the UvrABC nuclease and the unique structural feature of the DNA adducts can be used to explain the repair-dependent toxicities of this antitumor agent". Chemistry & Biology. 8 (11): 1033–1049. doi: 10.1016/s1074-5521(01)00071-0 . ISSN 1074-5521. PMID 11731295.
- ↑ Hemanta Baruah; Colin G. Barry; Ulrich Bierbach (2004). "Platinum-Intercalator Conjugates: From DNA-Targeted Cisplatin Derivatives to Adenine Binding Complexes as Potential Modulators of Gene Regulation". Current Topics in Medicinal Chemistry. 4 (15): 1537–1549. doi:10.2174/1568026043387313. ISSN 1568-0266. PMID 15579095.
- ↑ Chou, Ting-Chao (2006). "Theoretical Basis, Experimental Design, and Computerized Simulation of Synergism and Antagonism in Drug Combination Studies". Pharmacological Reviews. 58 (3): 621–681. doi:10.1124/pr.58.3.10. ISSN 0031-6997. PMID 16968952. S2CID 7055257.
- ↑ Roell, Kyle R.; Reif, David M.; Motsinger-Reif, Alison A. (2017). "An Introduction to Terminology and Methodology of Chemical Synergy—Perspectives from Across Disciplines". Frontiers in Pharmacology. 8: 158. doi: 10.3389/fphar.2017.00158 . ISSN 1663-9812. PMC 5397413 . PMID 28473769.
- ↑ Government of Canada, Canadian Centre for Occupational Health and Safety (2022). "Synergism and related terms : OSH Answers". www.ccohs.ca. Retrieved 2022-03-16.
- 1 2 Jia, Jia; Zhu, Feng; Ma, Xiaohua; Cao, Zhiwei W.; Li, Yixue X.; Chen, Yu Zong (2009). "Mechanisms of drug combinations: interaction and network perspectives". Nature Reviews Drug Discovery. 8 (2): 111–128. doi:10.1038/nrd2683. ISSN 1474-1776. PMID 19180105. S2CID 54466254.
- ↑ Johnson, Malcolm (2004). "Interactions between corticosteroids and beta2-agonists in asthma and chronic obstructive pulmonary disease". Proceedings of the American Thoracic Society. 1 (3): 200–206. doi:10.1513/pats.200402-010MS. ISSN 1546-3222. PMID 16113435.
- ↑ "Seretide Full Prescribing Information, Dosage & Side Effects | MIMS Hong Kong". www.mims.com. Retrieved 2022-04-18.
- ↑ Volpe, Massimo; Tocci, Giuliano (2012). "Rationale for triple fixed-dose combination therapy with an angiotensin II receptor blocker, a calcium channel blocker, and a thiazide diuretic". Vascular Health and Risk Management. 8: 371–380. doi: 10.2147/VHRM.S28359 . ISSN 1178-2048. PMC 3383291 . PMID 22745561.
- ↑ Kostis, John B. (2010). "Antihypertensive therapy with CCB/ARB combination in older individuals: focus on amlodipine/valsartan combination". American Journal of Therapeutics. 17 (2): 188–196. doi:10.1097/MJT.0b013e3181a2ba2d. ISSN 1536-3686. PMID 19433970. S2CID 205809141.
- ↑ Simons, Leon A. (2002). "Additive effect of plant sterol-ester margarine and cerivastatin in lowering low-density lipoprotein cholesterol in primary hypercholesterolemia". The American Journal of Cardiology. 90 (7): 737–740. doi:10.1016/s0002-9149(02)02600-0. ISSN 0002-9149. PMID 12356387.
- ↑ "Combination Cancer Therapy - Cancer". Merck Manuals Consumer Version. Retrieved 2022-03-16.
- ↑ Shenfield, G. M. (1982). "Fixed combination drug therapy". Drugs. 23 (6): 462–480. doi:10.2165/00003495-198223060-00003. ISSN 0012-6667. PMID 7049658. S2CID 25856967.
- ↑ Leon, Martin B.; Rosing, Douglas R.; Bonow, Robert O.; Epstein, Stephen E. (1985-01-25). "Combination therapy with calcium-channel blockers and beta blockers for chronic stable angina pectoris". American Journal of Cardiology. 55 (3): B69–B80. doi:10.1016/0002-9149(85)90615-0. ISSN 0002-9149. PMID 2857518.
- ↑ Hsiang, Kuo-Wei; Ng, Yee-Yung; Lu, Ching-Liang; Chen, Tseng-Shing; Lin, Hsiao-Yi; Luo, Jiing-Chyuan; Wu, Jia-Min; Lin, Han-Chieh; Chang, Full-Young; Lee, Shou-Dong (2010). "Corticosteroids therapy and peptic ulcer disease in nephrotic syndrome patients: Steroid therapy and peptic ulcer disease". British Journal of Clinical Pharmacology. 70 (5): 756–761. doi:10.1111/j.1365-2125.2010.03752.x. PMC 2997316 .
- ↑ Drina, Musa (2017-06-01). "Peptic ulcer disease and non-steroidal anti-inflammatory drugs". Australian Prescriber. 40 (3): 91–93. doi:10.18773/austprescr.2017.037. PMC 5478398 . PMID 28798512.