Related Research Articles

In anatomy, the atlas (C1) is the most superior (first) cervical vertebra of the spine and is located in the neck.

In anatomy, the axis or epistropheus is the second cervical vertebra (C2) of the spine, immediately inferior to the atlas, upon which the head rests.

Cervical spine disorders are illnesses that affect the cervical spine, which is made up of the upper first seven vertebrae, encasing and shielding the spinal cord. This fragment of the spine starts from the region above the shoulder blades and ends by supporting and connecting the skull.

Clearing the cervical spine is the process by which medical professionals determine whether cervical spine injuries exist, mainly regarding cervical fracture. It is generally performed in cases of major trauma. This process can take place in the emergency department or in the field by appropriately trained EMS personnel.
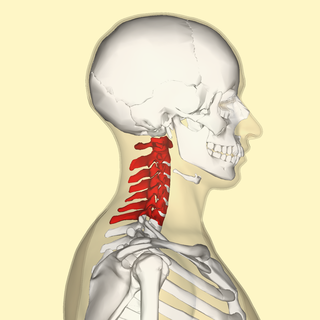
In tetrapods, cervical vertebrae are the vertebrae of the neck, immediately below the skull. Truncal vertebrae lie caudal of cervical vertebrae. In sauropsid species, the cervical vertebrae bear cervical ribs. In lizards and saurischian dinosaurs, the cervical ribs are large; in birds, they are small and completely fused to the vertebrae. The vertebral transverse processes of mammals are homologous to the cervical ribs of other amniotes. Most mammals have seven cervical vertebrae, with the only three known exceptions being the manatee with six, the two-toed sloth with five or six, and the three-toed sloth with nine.

A cervical fracture, commonly called a broken neck, is a fracture of any of the seven cervical vertebrae in the neck. Examples of common causes in humans are traffic collisions and diving into shallow water. Abnormal movement of neck bones or pieces of bone can cause a spinal cord injury, resulting in loss of sensation, paralysis, or usually death soon thereafter, primarily via compromising neurological supply to the respiratory muscles as well as innervation to the heart.

The vertebral arteries are major arteries of the neck. Typically, the vertebral arteries originate from the subclavian arteries. Each vessel courses superiorly along each side of the neck, merging within the skull to form the single, midline basilar artery. As the supplying component of the vertebrobasilar vascular system, the vertebral arteries supply blood to the upper spinal cord, brainstem, cerebellum, and posterior part of brain.
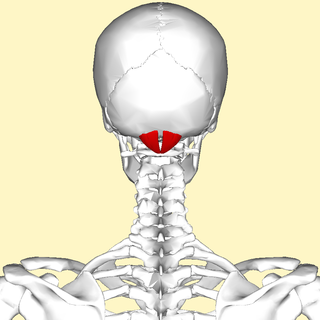
The rectus capitis posterior minor is a muscle in the upper back part of the neck. It is one of the suboccipital muscles. Its inferior attachment is at the posterior arch of atlas; its superior attachment is onto the occipital bone at and below the inferior nuchal line. The muscle is innervated by the suboccipital nerve. The muscle acts as a weak extensor of the head.
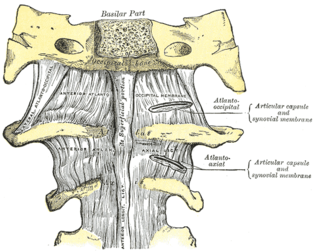
The atlanto-axial joint is a joint in the upper part of the neck between the atlas bone and the axis bone, which are the first and second cervical vertebrae. It is a pivot joint.
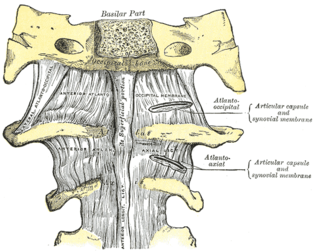
The atlanto-occipital joint is an articulation between the atlas bone and the occipital bone. It consists of a pair of condyloid joints. It is a synovial joint.

In anatomy, the transverse ligament of the atlas is a broad, though ligament which arches across the ring of the atlas posterior to the dens to keep the dens in contact with the atlas. It forms the transverse component of the cruciform ligament of atlas

Vertebral artery dissection (VAD) is a flap-like tear of the inner lining of the vertebral artery, which is located in the neck and supplies blood to the brain. After the tear, blood enters the arterial wall and forms a blood clot, thickening the artery wall and often impeding blood flow. The symptoms of vertebral artery dissection include head and neck pain and intermittent or permanent stroke symptoms such as difficulty speaking, impaired coordination, and visual loss. It is usually diagnosed with a contrast-enhanced CT or MRI scan.

Hangman's fracture is the colloquial name given to a fracture of both pedicles, or partes interarticulares, of the axis vertebra (C2).

The occipital condyles are undersurface protuberances of the occipital bone in vertebrates, which function in articulation with the superior facets of the atlas vertebra.
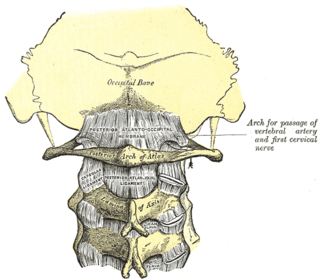
The posterior atlantooccipital membrane is a broad but thin membrane extending between the to the posterior margin of the foramen magnum above, and posterior arch of atlas below. It forms the floor of the suboccipital triangle.

The cruciate ligament of the atlas is a cross-shaped ligament in the neck forming part of the atlanto-axial joint. It consists of the transverse ligament of atlas, a superior longitudinal band, and an inferior longitudinal band.

A spinal fracture, also called a vertebral fracture or a broken back, is a fracture affecting the vertebrae of the spinal column. Most types of spinal fracture confer a significant risk of spinal cord injury. After the immediate trauma, there is a risk of spinal cord injury if the fracture is unstable, that is, likely to change alignment without internal or external fixation.

Cervicocranial syndrome or is a neurological illness. It is a combination of symptoms that are caused by an abnormality in the neck. The bones of the neck that are affected are cervical vertebrae. This syndrome can be identified by confirming cervical bone shifts, collapsed cervical bones or misalignment of the cervical bone leading to improper functioning of cervical spinal nerves.Greenberg Regenerative Medicine | Bryn Mawr, Pennsylvania Cervicocranial syndrome is either congenital or acquired. Some examples of diseases that could result in cervicocranial syndrome are Chiari disease, Klippel-Feil malformation osteoarthritis, and trauma. Treatment options include neck braces, pain medication and surgery. The quality of life for individuals suffering from CCJ syndrome can improve through surgery.
Craniocervical instability (CCI) is a medical condition where there is excessive movement of the vertebrae at the atlanto-occipital joint and the atlanto-axial joint, that is, between the skull and the top two vertebrae. This can cause neuronal injury and compression of nearby structures including the spinal cord, brain stem, vertebral artery or vagus nerve, causing a constellation of symptoms. It is frequently co-morbid with atlanto-axial instability, Chiari malformation and tethered cord syndrome.
Empty vertebral body sign is a radiological sign used for diagnosing any injury with flexion-distraction mechanism of the vertebrae, particularly Chance fracture of the vertebrae. In Chance fracture, there is disruption and angulation superiorly or inferiorly of posterior elements of the vertebrae. As a result, the affected vertebral body is seen as radiolucent in the anterio-posterior view.
References
- ↑ Theodore, N; Aarabi, B; Dhall, SS; Gelb, DE; Hurlbert, RJ; Rozzelle, CJ; Ryken, TC; Walters, BC; Hadley, MN (March 2013). "The diagnosis and management of traumatic atlanto-occipital dislocation injuries". Neurosurgery. 72 Suppl 2: 114–26. doi:10.1227/NEU.0b013e31827765e0. PMID 23417184.
- ↑ Lee, I. L; Vasquez, L. F; Tyroch, A. H; Trier, T. T (2017). "Association of Atlanto-Occipital Dislocation, Retroclival Hematoma, and Hydrocephalus: Management and Survival in a Pediatric Patient". Journal of Neurological Surgery Reports. 78 (1): e53–e58. doi:10.1055/s-0037-1600914. PMC 5357215 . PMID 28321388.
- ↑ Bisson, E; Schiffern, A; Daubs, MD; Brodke, DS; Patel, AA (15 April 2010). "Combined occipital-cervical and atlantoaxial disassociation without neurologic injury: case report and review of the literature". Spine. 35 (8): E316–21. doi:10.1097/brs.0b013e3181c41d2c. PMID 20308946. S2CID 19468690.
- ↑ Chaput, CD; Walgama, J; Torres, E; Dominguez, D; Hanson, J; Song, J; Rahm, M (20 April 2011). "Defining and detecting missed ligamentous injuries of the occipitocervical complex". Spine. 36 (9): 709–14. doi:10.1097/brs.0b013e3181de4ec1. PMID 21192303. S2CID 20243076.
- ↑ Hanson, JA; Deliganis, AV; Baxter, AB; Cohen, WA; Linnau, KF; Wilson, AJ; Mann, FA (May 2002). "Radiologic and clinical spectrum of occipital condyle fractures: retrospective review of 107 consecutive fractures in 95 patients". AJR. American Journal of Roentgenology. 178 (5): 1261–68. doi:10.2214/ajr.178.5.1781261. PMID 11959743.
- ↑ Chang W, Alexander MT, Mirvis SE (January 2009). "Diagnostic determinants of craniocervical distraction injury in adults". AJR. American Journal of Roentgenology. 192 (1): 52–8. doi:10.2214/ajr.07.3993. PMID 19098179.
- ↑ Theodore, N; Aarabi, B; Dhall, SS; Gelb, DE; Hurlbert, RJ; Rozzelle, CJ; Ryken, TC; Walters, BC; Hadley, MN (March 2013). "The diagnosis and management of traumatic atlanto-occipital dislocation injuries". Neurosurgery. 72 Suppl 2: 114–26. doi:10.1227/NEU.0b013e31827765e0. PMID 23417184.
- ↑ Gutiérrez-González, R; Boto, GR; Pérez-Zamarrón, A; Rivero-Garvía, M (September 2008). "Retropharyngeal pseudomeningocele formation as a traumatic atlanto-occipital dislocation complication: case report and review". European Spine Journal. 17 Suppl 2 (Suppl 2): S253–56. doi:10.1007/s00586-007-0531-7. PMC 2525892 . PMID 17973127.
- ↑ Cooper, Z; Gross, JA; Lacey, JM; Traven, N; Mirza, SK; Arbabi, S (1 May 2010). "Identifying survivors with traumatic craniocervical dissociation: a retrospective study". The Journal of Surgical Research. 160 (1): 3–8. doi:10.1016/j.jss.2009.04.004. PMID 19765722.
- ↑ Brinkman, William; Cohen, Wendy; Manning, Thomas (2003). "Posterior Fossa Subarachnoid Hemorrhage Due to an Atlantooccipital Dislocation". American Journal of Roentgenology. 180 (5): 1476. doi:10.2214/ajr.180.5.1801476. PMID 12704071 . Retrieved 2018-05-14.
- ↑ "Traumatic Atlantooccipital Dislocation with Survival" (PDF). www.ajnr.org. Retrieved 2018-05-14.
- ↑ Park JB, Ha KY, Chang H. Traumatic posterior atlantooccipital dislocation with Jefferson fracture and fracture-dislocation of C6-C7: a case report with survival. Eur Spine J. 2001 Dec;10(6):524-8. doi: 10.1007/s005860100334. PMID 11806394; PMCID: PMC3611534.
- ↑ Chaput, CD; Torres, E; Davis, M; Song, J; Rahm, M (August 2011). "Survival of atlanto-occipital dissociation correlates with atlanto-occipital distraction, injury severity score, and neurologic status". The Journal of Trauma. 71 (2): 393–95. doi:10.1097/ta.0b013e3181eb6a31. PMID 21206289.