Related Research Articles

Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. Cognitive behavioral therapy is one of the most effective means of treatment for substance abuse and co-occurring mental health disorders. CBT focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include many issues and the treatment of many mental health conditions, including anxiety, substance use disorders, marital problems, ADHD, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.
Drug rehabilitation is the process of medical or psychotherapeutic treatment for dependency on psychoactive substances such as alcohol, prescription drugs, and street drugs such as cannabis, cocaine, heroin or amphetamines. The general intent is to enable the patient to confront substance dependence, if present, and stop substance misuse to avoid the psychological, legal, financial, social, and physical consequences that can be caused.

Anger management is a psycho-therapeutic program for anger prevention and control. It has been described as deploying anger successfully. Anger is frequently a result of frustration, or of feeling blocked or thwarted from something the subject feels is important. Anger can also be a defensive response to underlying fear or feelings of vulnerability or powerlessness. Anger management programs consider anger to be a motivation caused by an identifiable reason which can be logically analyzed and addressed.
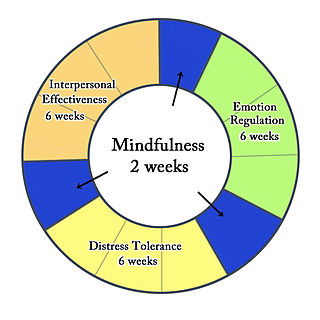
Dialectical behavior therapy (DBT) is an evidence-based psychotherapy that began with efforts to treat personality disorders and interpersonal conflicts. Evidence suggests that DBT can be useful in treating mood disorders and suicidal ideation as well as for changing behavioral patterns such as self-harm and substance use. DBT evolved into a process in which the therapist and client work with acceptance and change-oriented strategies and ultimately balance and synthesize them—comparable to the philosophical dialectical process of thesis and antithesis, followed by synthesis.
Mindfulness-based cognitive therapy (MBCT) is an approach to psychotherapy that uses cognitive behavioral therapy (CBT) methods in conjunction with mindfulness meditative practices and similar psychological strategies. The origins to its conception and creation can be traced back to the traditional approaches from East Asian formative and functional medicine, philosophy and spirituality, birthed from the basic underlying tenets from classical Taoist, Buddhist and Traditional Chinese medical texts, doctrine and teachings.

In applied psychology, interventions are actions performed to bring about change in people. A wide range of intervention strategies exist and they are directed towards various types of issues. Most generally, it means any activities used to modify behavior, emotional state, or feelings. Psychological interventions have many different applications and the most common use is for the treatment of mental disorders, most commonly using psychotherapy. The ultimate goal behind these interventions is not only to alleviate symptoms but also to target the root cause of mental disorders.
Cognitive therapy (CT) is a type of psychotherapy developed by American psychiatrist Aaron T. Beck. CT is one therapeutic approach within the larger group of cognitive behavioral therapies (CBT) and was first expounded by Beck in the 1960s. Cognitive therapy is based on the cognitive model, which states that thoughts, feelings and behavior are all connected, and that individuals can move toward overcoming difficulties and meeting their goals by identifying and changing unhelpful or inaccurate thinking, problematic behavior, and distressing emotional responses. This involves the individual working with the therapist to develop skills for testing and changing beliefs, identifying distorted thinking, relating to others in different ways, and changing behaviors. A cognitive case conceptualization is developed by the cognitive therapist as a guide to understand the individual's internal reality, select appropriate interventions and identify areas of distress.
SMART Recovery is an international community of peer support groups that help people recover from addictive and problematic behaviors, using a self-empowering and evidence-informed program. SMART stands for Self-Management and Recovery Training. The SMART approach is secular and research-based. SMART has a global reach, with a presence established in more than 30 countries. SMART Recovery is effective with a range of addictive and problematic behaviors

Polysubstance dependence refers to a type of substance use disorder in which an individual uses at least three different classes of substances indiscriminately and does not have a favorite substance that qualifies for dependence on its own. Although any combination of three substances can be used, studies have shown that alcohol is commonly used with another substance. This is supported by one study on polysubstance use that separated participants who used multiple substances into groups based on their preferred substance. The results of a longitudinal study on substance use led the researchers to observe that excessively using or relying on one substance increased the probability of excessively using or relying on another substance.
In psychology and neuroscience, executive dysfunction, or executive function deficit, is a disruption to the efficacy of the executive functions, which is a group of cognitive processes that regulate, control, and manage other cognitive processes. Executive dysfunction can refer to both neurocognitive deficits and behavioural symptoms. It is implicated in numerous psychopathologies and mental disorders, as well as short-term and long-term changes in non-clinical executive control. Executive dysfunction is the mechanism underlying ADHD Paralysis, and in a broader context, it can encompass other cognitive difficulties like planning, organizing, initiating tasks and regulating emotions. It is a core characteristic of ADHD and can elucidate numerous other recognized symptoms.
Cognitive remediation is designed to improve neurocognitive abilities such as attention, working memory, cognitive flexibility and planning, and executive functioning which leads to improved psychosocial functioning.
Attentional retraining is the retraining of automatic attentional processes. The method of retraining varies but has typically employed computerized training programs. The term originally indicated retraining of attention to rehabilitate individuals after a brain injury who had neurological disorders of attention including hemineglect, perseveration, limited attention span, and even ADHD. However, in more recent research and clinical applications attentional retraining has also been applied as a type of cognitive bias modification. In this application, attentional retraining refers to the retraining of automatic attentional biases that have been observed in high levels of anxiety.
PTSD or post-traumatic stress disorder, is a psychiatric disorder characterised by intrusive thoughts and memories, dreams or flashbacks of the event; avoidance of people, places and activities that remind the individual of the event; ongoing negative beliefs about oneself or the world, mood changes and persistent feelings of anger, guilt or fear; alterations in arousal such as increased irritability, angry outbursts, being hypervigilant, or having difficulty with concentration and sleep.
About 1 in 7 Americans suffer from active addiction to a particular substance. Addiction can cause physical, psychological, and emotional harm to those who are affected by it. The American Society of Addiction Medicine defines addiction as "a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual's life experiences. People with addiction use substances or engage in behaviors that become compulsive and often continue despite harmful consequences." In the world of psychology and medicine, there are two models that are commonly used in understanding the psychology behind addiction itself. One model is referred to as the disease model of addiction. The disease model suggests that addiction is a diagnosable disease similar to cancer or diabetes. This model attributes addiction to a chemical imbalance in an individual's brain that could be caused by genetics or environmental factors. The second model is the choice model of addiction, which holds that addiction is a result of voluntary actions rather than some dysfunction of the brain. Through this model, addiction is viewed as a choice and is studied through components of the brain such as reward, stress, and memory. Substance addictions relate to drugs, alcohol, and smoking. Process addictions relate to non-substance-related behaviors such as gambling, spending money, sexual activity, gaming, spending time on the internet, and eating.
Cognitive emotional behavioral therapy (CEBT) is an extended version of cognitive behavioral therapy (CBT) aimed at helping individuals to evaluate the basis of their emotional distress and thus reduce the need for associated dysfunctional coping behaviors. This psychotherapeutic intervention draws on a range of models and techniques including dialectical behavior therapy (DBT), mindfulness meditation, acceptance and commitment therapy (ACT), and experiential exercises.
Relapse prevention (RP) is a cognitive-behavioral approach to relapse with the goal of identifying and preventing high-risk situations such as unhealthy substance use, obsessive-compulsive behavior, sexual offending, obesity, and depression. It is an important component in the treatment process for alcohol use disorder, or alcohol dependence. This model founding is attributed to Terence Gorski's 1986 book "Staying Sober."
Trauma focused cognitive behavioral therapy (TF-CBT) is an evidence-based psychotherapy or counselling that aims at addressing the needs of children and adolescents with post traumatic stress disorder (PTSD) and other difficulties related to traumatic life events. This treatment was developed and proposed by Drs. Anthony Mannarino, Judith Cohen, and Esther Deblinger in 2006. The goal of TF-CBT is to provide psychoeducation to both the child and non-offending caregivers, then help them identify, cope, and re-regulate maladaptive emotions, thoughts, and behaviors. Research has shown TF-CBT to be effective in treating childhood PTSD and with children who have experienced or witnessed traumatic events, including but not limited to physical or sexual victimization, child maltreatment, domestic violence, community violence, accidents, natural disasters, and war. More recently, TF-CBT has been applied to and found effective in treating complex posttraumatic stress disorder.
Compassion-focused therapy (CFT) is a system of psychotherapy developed by Paul Gilbert that integrates techniques from cognitive behavioral therapy with concepts from evolutionary psychology, social psychology, developmental psychology, Buddhist psychology, and neuroscience. According to Gilbert, "One of its key concerns is to use compassionate mind training to help people develop and work with experiences of inner warmth, safeness and soothing, via compassion and self-compassion."
Donald H. Meichenbaum is an American psychologist and Distinguished Professor Emeritus of Psychology at the University of Waterloo, Ontario. He is a research director of the Melissa Institute for Violence Prevention and Treatment at the University of Miami. Meichenbaum is known for his research and publications on psychotherapy, and contributed to the development of the technique of cognitive-behavioural therapy (CBT). In 1982, a survey of 800 members of the American Psychological Association voted Meichenbaum the tenth most influential psychotherapist of the 20th century. At the time of his retirement from the University of Waterloo in 1998, Meichenbaum was the most-cited psychology researcher at a Canadian university.

Mindfulness-Oriented Recovery Enhancement (MORE) is an evidence-based mind-body therapy program developed by Eric Garland. It is a therapeutic approach grounded in affective neuroscience that combines mindfulness training with reappraisal and savoring skills. Garland developed this approach by combining the key features of mindfulness training, "Third Wave" cognitive-behavioral therapy, and principles from positive psychology.
References
- 1 2 3 Bledowski C, Kaiser J, Rahm B (December 2010). "Basic operations in working memory: contributions from functional imaging studies". Behavioural Brain Research. 214 (2): 172–9. doi:10.1016/j.bbr.2010.05.041. PMID 20678984. S2CID 10918930.
- 1 2 3 4 Adams RC, Sedgmond J, Maizey L, Chambers CD, Lawrence NS (September 2019). "Food Addiction: Implications for the Diagnosis and Treatment of Overeating". Nutrients. 11 (9): 2086. doi: 10.3390/nu11092086 . PMC 6770567 . PMID 31487791.
- 1 2 3 4 5 6 7 8 9 10 11 Nixon SJ, Lewis B (September 2019). "Cognitive training as a component of treatment of alcohol use disorder: A review". Neuropsychology. 33 (6): 822–841. doi:10.1037/neu0000575. PMC 7429442 . PMID 31448949.
- 1 2 Lawrence BJ, Jayakody DM, Henshaw H, Ferguson MA, Eikelboom RH, Loftus AM, Friedland PL (2018-08-10). "Auditory and Cognitive Training for Cognition in Adults With Hearing Loss: A Systematic Review and Meta-Analysis". Trends in Hearing. 22: 2331216518792096. doi:10.1177/2331216518792096. PMC 6088475 . PMID 30092719.
- 1 2 "Cognitive Behavioral Therapy | Psychology Today". www.psychologytoday.com. Retrieved 2020-11-30.
- ↑ Simons DJ, Boot WR, Charness N, Gathercole SE, Chabris CF, Hambrick DZ, Stine-Morrow EA (October 2016). "Do "Brain-Training" Programs Work?". Psychological Science in the Public Interest. 17 (3): 103–186. doi:10.1177/1529100616661983. PMID 27697851. S2CID 13729927.
- ↑ Harvey PD, McGurk SR, Mahncke H, Wykes T (November 2018). "Controversies in Computerized Cognitive Training". Biological Psychiatry. Cognitive Neuroscience and Neuroimaging. 3 (11): 907–915. doi: 10.1016/j.bpsc.2018.06.008 . PMID 30197048.
- 1 2 3 4 Jones A, Hardman CA, Lawrence N, Field M (May 2018). "Cognitive training as a potential treatment for overweight and obesity: A critical review of the evidence". Appetite. 124: 50–67. doi: 10.1016/j.appet.2017.05.032 . hdl: 10871/27978 . PMID 28546010. S2CID 3844999.
- 1 2 3 Verdejo-Garcia A, Garcia-Fernandez G, Dom G (September 2019). "Cognition and addiction". Dialogues in Clinical Neuroscience. 21 (3): 281–290. doi:10.31887/DCNS.2019.21.3/gdom. PMC 6829168 . PMID 31749652.
- 1 2 3 4 5 Bickel WK, Moody L, Quisenberry A (2014). "Computerized Working-Memory Training as a Candidate Adjunctive Treatment for Addiction". Alcohol Research. 36 (1): 123–6. PMC 4432851 . PMID 26259006.
- 1 2 Anzman SL, Birch LL (November 2009). "Low inhibitory control and restrictive feeding practices predict weight outcomes". The Journal of Pediatrics. 155 (5): 651–6. doi:10.1016/j.jpeds.2009.04.052. PMC 2764786 . PMID 19595373.
- ↑ Stice E, Lawrence NS, Kemps E, Veling H (November 2016). "Training motor responses to food: A novel treatment for obesity targeting implicit processes". Clinical Psychology Review. 49: 16–27. doi:10.1016/j.cpr.2016.06.005. hdl: 10871/24679 . PMID 27498406.
- 1 2 Snider SE, Deshpande HU, Lisinski JM, Koffarnus MN, LaConte SM, Bickel WK (February 2018). "Working Memory Training Improves Alcohol Users' Episodic Future Thinking: A Rate-Dependent Analysis". Biological Psychiatry. Cognitive Neuroscience and Neuroimaging. 3 (2): 160–167. doi:10.1016/j.bpsc.2017.11.002. PMC 5851289 . PMID 29529411.
- 1 2 Kerst WF, Waters AJ (October 2014). "Attentional retraining administered in the field reduces smokers' attentional bias and craving". Health Psychology. 33 (10): 1232–40. doi:10.1037/a0035708. PMID 24818609.
- ↑ "Our Programs | LearningRx Brain Training Center". LearningRx. Retrieved 2020-11-30.
- ↑ Bae H, Han C, Kim D (March 2015). "Desensitization of triggers and urge reprocessing for pathological gambling: a case series". Journal of Gambling Studies. 31 (1): 331–42. doi:10.1007/s10899-013-9422-5. PMID 24293014. S2CID 12800888.
- ↑ Alavi, Seyyed Salman; Ferdosi, Masoud; Jannatifard, Fereshte; Eslami, Mehdi; Alaghemandan, Hamed; Setare, Mehrdad (April 2012). "Behavioral Addiction versus Substance Addiction: Correspondence of Psychiatric and Psychological Views". International Journal of Preventive Medicine. 3 (4): 290–294. ISSN 2008-7802. PMC 3354400 . PMID 22624087.
- ↑ "Rational Emotive Behavior Therapy | Psychology Today". www.psychologytoday.com. Retrieved 2020-11-25.
- ↑ Martin J, Young DM (February 2003). "Comparison of American Cancer Society versus Internet Based treatment for Smokers" (PDF). San Diego State University Graduate Research. Archived from the original (PDF) on 2013-07-01.
- ↑ Wooley M, Whitlock J (February 2001). "Case Study #1" (PDF). St. Lukes Hospital and Medical Center. San Antonio TX. Archived from the original (PDF) on 2013-07-01.
- ↑ Diabetes Research Group "Cognitive Behavioral Group Training for Patients with Type 1 Diabetes" March 2005
- ↑ Kucyi A, Salomons TV, Davis KD (September 2016). "Cognitive behavioral training reverses the effect of pain exposure on brain network activity" (PDF). Pain. 157 (9): 1895–1904. doi:10.1097/j.pain.0000000000000592. PMID 27101426. S2CID 34665112.
- 1 2 3 4 Lau HM, Smit JH, Fleming TM, Riper H (2017). "Serious Games for Mental Health: Are They Accessible, Feasible, and Effective? A Systematic Review and Meta-analysis". Frontiers in Psychiatry. 7: 209. doi: 10.3389/fpsyt.2016.00209 . PMC 5241302 . PMID 28149281.
- ↑ Gallagher A. "Cognitive behavioral or relaxation training helps women reduce distress during breast cancer treatment". Science Daily.
- ↑ Gold MS. "Stages of Change". Psyche Central.