A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

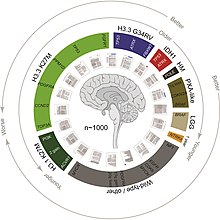
A glioma is a type of tumor that starts in the glial cells of the brain or the spine. Gliomas comprise about 30 percent of all brain tumors and central nervous system tumours, and 80 percent of all malignant brain tumours.

Oligodendrogliomas are a type of glioma that are believed to originate from the oligodendrocytes of the brain or from a glial precursor cell. They occur primarily in adults but are also found in children.

Glioblastoma, previously known as glioblastoma multiforme (GBM), is the most aggressive and most common type of cancer that originates in the brain, and has very poor prognosis for survival. Initial signs and symptoms of glioblastoma are nonspecific. They may include headaches, personality changes, nausea, and symptoms similar to those of a stroke. Symptoms often worsen rapidly and may progress to unconsciousness.

Astrocytoma is a type of brain tumor. Astrocytomas originate from a specific kind of star-shaped glial cell in the cerebrum called an astrocyte. This type of tumor does not usually spread outside the brain and spinal cord and it does not usually affect other organs. After glioblastomas, astrocytomas are the second most common glioma and can occur in most parts of the brain and occasionally in the spinal cord.
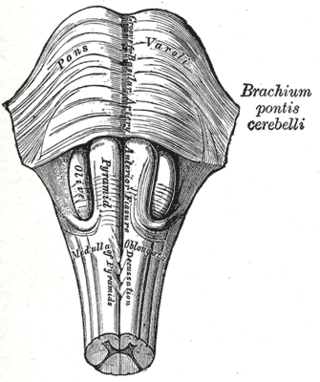
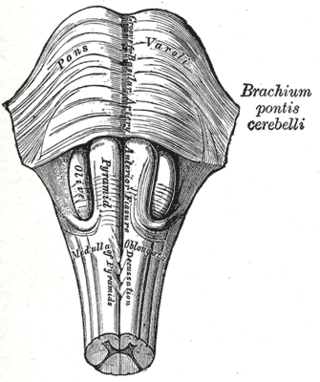
Central neurogenic hyperventilation (CNH) is an abnormal pattern of breathing characterized by deep and rapid breaths at a rate of at least 25 breaths per minute. Increasing irregularity of this respiratory rate generally is a sign that the patient will enter into coma. CNH is unrelated to other forms of hyperventilation, like Kussmaul's respirations. CNH is the human body's response to reduced carbon dioxide levels in the blood. This reduction in carbon dioxide is caused by contraction of cranial arteries from damage caused by lesions in the brain stem. However, the mechanism by which CNH arises as a result from these lesions is still very poorly understood. Current research has yet to provide an effective means of treatment for the rare number of patients who are diagnosed with this condition.

Pilocytic astrocytoma is a brain tumor that occurs most commonly in children and young adults. They usually arise in the cerebellum, near the brainstem, in the hypothalamic region, or the optic chiasm, but they may occur in any area where astrocytes are present, including the cerebral hemispheres and the spinal cord. These tumors are usually slow growing and benign, corresponding to WHO malignancy grade 1.

Medulloblastoma is a common type of primary brain cancer in children. It originates in the part of the brain that is towards the back and the bottom, on the floor of the skull, in the cerebellum, or posterior fossa.

Primary central nervous system lymphoma (PCNSL), also termed primary diffuse large B-cell lymphoma of the central nervous system (DLBCL-CNS), is a primary intracranial tumor appearing mostly in patients with severe immunodeficiency. It is a subtype and one of the most aggressive of the diffuse large B-cell lymphomas.

Lomustine is an alkylating nitrosourea compound used in chemotherapy. It is closely related to semustine and is in the same family as streptozotocin. It is a highly lipid-soluble drug, thus it crosses the blood–brain barrier. This property makes it ideal for treating brain tumors, which is its primary use, although it is also used to treat Hodgkin lymphoma as a second-line option. It has also been used in veterinary practice as a treatment for cancers in cats and dogs.

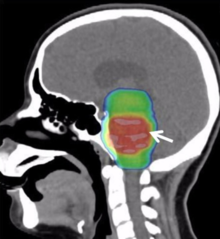
A brainstem glioma is a cancerous glioma tumor in the brainstem. Around 75% are diagnosed in children and young adults under the age of twenty, but have been known to affect older adults as well. Brainstem gliomas start in the brain or spinal cord tissue and typically spread throughout the nervous system.
Neuro-oncology is the study of brain and spinal cord neoplasms, many of which are very dangerous and life-threatening. Among the malignant brain cancers, gliomas of the brainstem and pons, glioblastoma multiforme, and high-grade astrocytoma/oligodendroglioma are among the worst. In these cases, untreated survival usually amounts to only a few months, and survival with current radiation and chemotherapy treatments may extend that time from around a year to a year and a half, possibly two or more, depending on the patient's condition, immune function, treatments used, and the specific type of malignant brain neoplasm. Surgery may in some cases be curative, but, as a general rule, malignant brain cancers tend to regenerate and emerge from remission easily, especially highly malignant cases. In such cases, the goal is to excise as much of the mass and as much of the tumor margin as possible without endangering vital functions or other important cognitive abilities. The Journal of Neuro-Oncology is the longest continuously published journal in the field and serves as a leading reference to those practicing in the area of neuro-oncology.

Plus Therapeutics, Inc. is a clinical-stage pharmaceutical company developing innovative, targeted radiotherapeutics for adults and children with rare and difficult-to-treat cancers. The company is headquartered in Austin, Texas, United States.
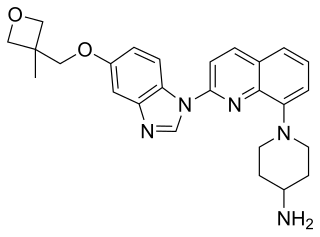
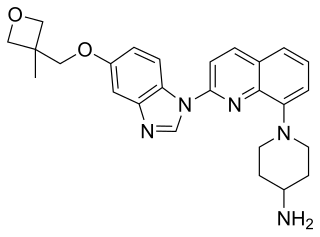
Crenolanib besylate is an investigational inhibitor being developed by AROG Pharmaceuticals, LLC. The compound is currently being evaluated for safety and efficacy in clinical trials for various types of cancer, including acute myeloid leukemia (AML), gastrointestinal stromal tumor (GIST), and glioma. Crenolanib is an orally bioavailable benzimidazole that selectively and potently inhibits signaling of wild-type and mutant isoforms of class III receptor tyrosine kinases (RTK) FLT3, PDGFR α, and PDGFR β. Unlike most RTK inhibitors, crenolanib is a type I mutant-specific inhibitor that preferentially binds to phosphorylated active kinases with the ‘DFG in’ conformation motif.
Ren Michael Pedersen OAM 4 February 1971, Atherton, North Queensland, Australia), is a prominent international advocate for children's brain cancer research.
Clinica 0-19 is a medical clinic in Monterrey, Mexico that claims to treat diffuse intrinsic pontine glioma (DIPG). Although DIPG is currently regarded as one of the most devastating pediatric cancers, with a survival rate of <1% over five years, the clinic states that their treatment, which can cost hundreds of thousands of dollars, has resulted in some patients no longer having any evidence of disease. However, there is no credible evidence to support their claims and at least some of their patients were found to have tumor growth a few months later. Oncologists and others have criticized the clinic's lead doctors, Alberto Siller and Alberto Garcia, for their lack of transparency, for not publishing their treatment protocol or survival rates, for the high costs of treatment, and for discouraging their patients from using radiation therapy.
A central nervous system tumor is an abnormal growth of cells from the tissues of the brain or spinal cord. CNS tumor is a generic term encompassing over 120 distinct tumor types. Common symptoms of CNS tumors include vomiting, headache, changes in vision, nausea, and seizures. A CNS tumor can be detected and classified via neurological examination, medical imaging, such as x-ray imaging, magnetic resonance imaging (MRI) or computed tomography (CT), or after analysis of a biopsy.

Crystal L. Mackall is an American physician and immunologist. She is currently the Ernest and Amelia Gallo Family Professor of Pediatrics and Medicine at Stanford University. She is the founding director of the Stanford Center for Cancer Cell Therapy.

Michelle Leigh Monje-Deisseroth is a neuroscientist and neuro-oncologist. She is a professor of neurology at Stanford University and an investigator with the Howard Hughes Medical Institute. She develops new treatments for diffuse intrinsic pontine glioma.

Zotiraciclib (TG02) is a potent oral spectrum selective kinase inhibitor for the treatment of cancer. It was discovered in Singapore by S*BIO Pte Ltd and falls under the category of small molecule macrocycles. It crosses the blood brain barrier and acts by depleting Myc through the inhibition of cyclin-dependent kinase 9 (CDK9). It is one of a number of CDK inhibitors under investigation; others targeting CDK9 for the treatment of acute myeloid leukemia include alvocidib and atuveciclib. Myc overexpression is a known factor in many cancers, with 80 percent of glioblastomas characterized by this property. Zotiraciclib has been granted orphan drug designation by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for the treatment of gliomas.