Lichen planus (LP) is a chronic inflammatory and autoimmune disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, but is named for its appearance. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. The hue may be gray-brown in people with darker skin. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

Angiokeratoma is a benign cutaneous lesion of capillaries, resulting in small marks of red to blue color and characterized by hyperkeratosis. Angiokeratoma corporis diffusum refers to Fabry's disease, but this is usually considered a distinct condition.
Palisaded neutrophilic and granulomatous dermaititis (PNGS) is usually associated with a well-defined connective tissue disease, lupus erythematosus or rheumatoid arthritis most commonly, and often presents with eroded or ulcerated symmetrically distributed umbilicated papules or nodules on the elbows.
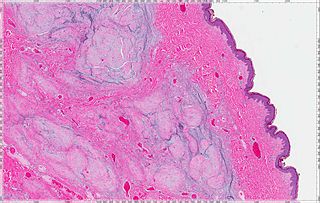
Eccrine angiomatous hamartoma (EAH), first described by Lotzbeck in 1859, is a rare benign vascular hamartoma characterized histologically by a proliferation of eccrine and vascular components. EAH exists on a spectrum of cutaneous tumors that include eccrine nevus, mucinous eccrine nevus and EAH. Each diagnostic subtype is characterized by an increase in the number as well as size of mature eccrine glands or ducts, with EAH being distinguished by the added vascular component.

Acrokeratoelastoidosis of Costa or Acrokeratoelastoidosis is a hereditary form of marginal keratoderma, and can be defined as a palmoplantar keratoderma. It is distinguished by tiny, firm pearly or warty papules on the sides of the hands and, occasionally, the feet. It is less common than the hereditary type of marginal keratoderma, keratoelastoidosis marginalis.
Microvenular hemangioma is an acquired benign vascular tumor that presents as an asymptomatic, slowly growing, 0.5- to 2.0 cm reddish lesion on the forearms or other sites of young to middle-aged adults. The cause of microvenular hemangioma is unknown, however it has been associated with immunosuppression.

Nevus lipomatosus superficialis is characterized by soft, yellowish papules or cerebriform plaques, usually of the buttock or thigh, less often of the ear or scalp, with a wrinkled rather than warty surface. It is usually congenital in origin or appears within the first three decades.
Targetoid hemosiderotic hemangioma, also known as a hobnail hemangioma is a skin condition characterized by a central brown or purplish papule that is surrounded by an ecchymotic halo. It may appear similar to melanoma. It was first described by Santa Cruz and Aronberg in 1988.

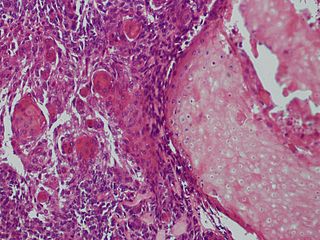
Atypical fibroxanthoma (AFX) of the skin is a low-grade malignancy related to malignant fibrous histiocytoma, which it resembles histologically. Atypical fibroxanthoma manifests as a hard, pink or red papule or nodule that grows over the course of several months and may bleed or ulcerate. They typically occur on the head and neck. Atypical fibroxanthoma is usually asymptomatic.
A cutaneous myxoma, or superficial angiomyxoma, consists of a multilobulated myxoid mass containing stellate or spindled fibroblasts with pools of mucin forming cleft-like spaces. There is often a proliferation of blood vessels and an inflammatory infiltrate. Staining is positive for vimentin, negative for cytokeratin and desmin, and variable for CD34, Factor VIIIa, SMA, MSA and S-100.

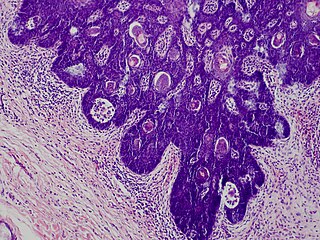
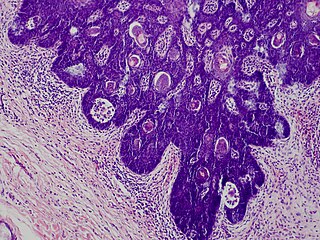
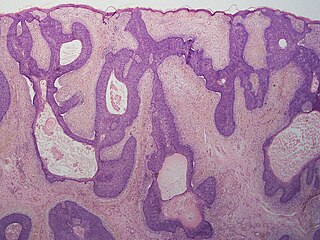
Warty dyskeratoma, also known as an Isolated dyskeratosis follicularis, is a benign epidermal proliferation with distinctive histologic findings that may mimic invasive squamous cell carcinoma and commonly manifests as an umbilicated lesion with a keratotic plug, WD have some histopathologic similarities to viral warts but it's not caused by HPV and the majority of these lesions display overall histopathologic features consistent with a follicular adnexal neoplasm. Usually limited to the head, neck, scalp or face and vulva. Lesions are generally solitary and sporadic and may be associated with a follicular unit. Oral involvement, particularly the hard palate, and genital involvement have been reported. it can also be thought of as one of the manifestations of focal acantholytic dyskeratosis, an epidermal reaction pattern that can be seen in several disorders, including Darier's disease and Grover's disease. But the main Difference between Darier disease and Warty dyskeratoma, is that Darier disease inherited dermatosis consisting of multiple keratotic papules on the face, trunk, and extremities, while WD occurs as an isolated, noninherited, single keratotic nodule mainly confined to the head and neck as mentioned earlier.
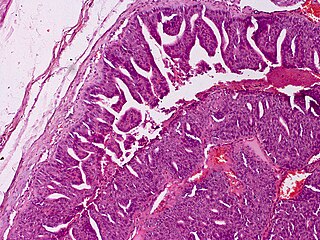
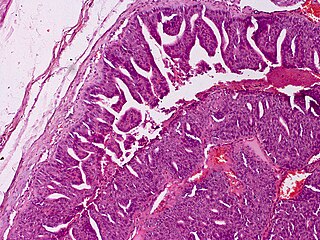
Verruciform xanthoma is an uncommon benign lesion that has a verruciform (wart-like) appearance, but it may appear polypoid, papillomatous, or sessile. The verruciform was first described by Shafer in 1971 on the oral mucosa. Usually found on the oral mucosa of middle-aged persons, verruciform xanthomas have also been reported on the scrotum and penis of middle-aged to elderly Japanese males. While the most common site is the oral mucosa, lesions that occur elsewhere usually arise on the perineum or on the skin with some predisposing factor, such as lymphedema or an epidermal nevus.
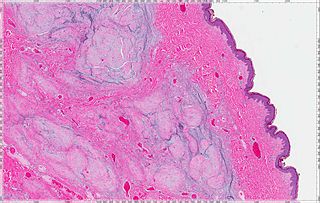
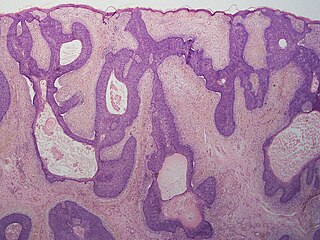
Folliculosebaceous cystic hamartoma abbreviated as (FSCH) is a rare cutaneous hamartoma consisting of dilated folliculosebaceous units invested in mesenchymal elements. it typically affects adults, have a predilection for the central face or scalp, with less than 1.5 cm dimension. Clinically, the lesions are asymptomatic, rubbery to firm in consistency, and usually occur on or above the neck in of cases, Histopathologically, FSCH shares several similar features to sebaceous trichofolliculoma, but it is usually possible to differentiate these two tumors.
Progressive nodular histiocytosis is a cutaneous condition clinically characterized by the development of two types of skin lesions: superficial papules and deeper larger subcutaneous nodules. Progressive nodular histiocytosis was first reported in 1978 by Taunton et al. It is a subclass of non-Langerhans cell histiocytosis and a subgroup of xanthogranuloma.
Indeterminate cell histiocytosis(LCH) is an uncommon proliferative illness where the predominant cells have characteristics from both non-Langerhans cell histiocytosis (NLCH) and Langerhans cell histiocytosis (LCH) in terms of morphology and immunophenotypic characteristics. Wood et al. originally described ICH in 1985 as a neoplastic disease arising from dermal indeterminate cells that lack Birbeck granules but are characteristically positive for S-100 and CD1a.
Aggressive digital papillary adenocarcinoma, also known as digital papillary adenocarcinoma and papillary adenoma is a cutaneous condition characterized by an aggressive malignancy involving the digit between the nailbed and the distal interphalangeal joint spaces. Genetic studies reveal that human papilloma virus HPV42 is the likely driving virus in this cancer.
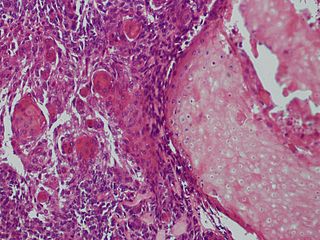
Malignant pilomatricoma is a cutaneous condition characterized by a locally aggressive tumor composed of hair-matrix cells.
Basaloid follicular hamartoma is a cutaneous condition characterized as distinctive benign adnexal tumor that has several described variants. It manifest as small tan or brown coloured papules in the trunk, pubic area, face, scalp, and axilla.
Mucinous nevus is a rare cutaneous condition characterized by hamartoma that can be congenital or acquired. Mucinous nevus presents as multiple skin-coloured or brown asymptomatic papules or plaques. Mucinous nevus is diagnosed based of histological features. Treatment is not needed.
Multinucleate cell angiohistiocytoma (MCAH) is a cutaneous condition that presents as slowly growing, multiple, discrete but grouped, red to violaceous papules