Related Research Articles

Ameloblastoma is a rare, benign or cancerous tumor of odontogenic epithelium much more commonly appearing in the lower jaw than the upper jaw. It was recognized in 1827 by Cusack. This type of odontogenic neoplasm was designated as an adamantinoma in 1885 by the French physician Louis-Charles Malassez. It was finally renamed to the modern name ameloblastoma in 1930 by Ivey and Churchill.

Cementoblastoma, or benign cementoblastoma, is a relatively rare benign neoplasm of the cementum of the teeth. It is derived from ectomesenchyme of odontogenic origin. Cementoblastomas represent less than 0.69–8% of all odontogenic tumors.
Epulis fissuratum is a benign hyperplasia of fibrous connective tissue which develops as a reactive lesion to chronic mechanical irritation produced by the flange of a poorly fitting denture. More simply, epulis fissuratum is where excess folds of firm tissue form inside the mouth, as a result of rubbing on the edge of dentures that do not fit well. It is a harmless condition and does not represent oral cancer. Treatment is by simple surgical removal of the lesion, and also by adjustment of the denture or provision of a new denture.
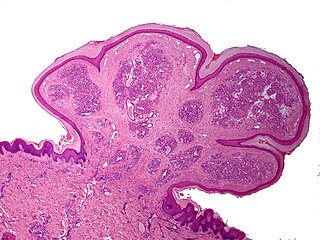
Inflammatory papillary hyperplasia (IPH) is a benign lesion of the oral mucosa which is characterized by the growth of one or more nodular lesions, measuring about 2mm or less. The lesion almost exclusively involves the hard palate, and in rare instances, it also has been seen on the mandible. The lesion is mostly asymptomatic and color of the mucosa may vary from pink to red.
A pyogenic granuloma or lobular capillary hemangioma is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. It is often found to involve the gums, skin, or nasal septum, and has also been found far from the head, such as in the thigh.
Peripheral giant-cell granuloma (PGCG) is an oral pathologic condition that appears in the mouth as an overgrowth of tissue due to irritation or trauma. Because of its overwhelming incidence on the gingiva, the condition is associated with two other diseases, pyogenic granuloma and peripheral ossifying fibroma. These three diseases are associated because they appear frequently on gingiva. Due to its similar microscopic appearance, peripheral giant-cell granuloma is considered to be the soft tissue equivalent of central giant-cell granuloma.
A peripheral ossifying fibroma, also known as ossifying fibrous epulis, is “a gingival nodule which is composed of a cellular fibroblastic connective tissue stroma which is associated with the formation of randomly dispersed foci of mineralised products, which consists of bone, cementum-like tissue, or a dystrophic calcification. The lesion is considered part of an ossifying fibroma, but that is usually considered to be a jaw tumor. Because of its overwhelming incidence on the gingiva, the condition is associated with two other diseases, though not because they occur together. Instead, the three are associated with each other because they appear frequently on gingiva: pyogenic granuloma and peripheral giant cell granuloma. Some researchers believe peripheral ossifying fibromas to be related to pyogenic fibromas and, in some instances, are the result of a pyogenic granuloma which has undergone fibrosis and calcification.

A dentigerous cyst, also known as a follicular cyst, is an epithelial-lined developmental cyst formed by accumulation of fluid between the reduced enamel epithelium and the crown of an unerupted tooth. It is formed when there is an alteration in the reduced enamel epithelium and encloses the crown of an unerupted tooth at the cemento-enamel junction. Fluid is accumulated between reduced enamel epithelium and the crown of an unerupted tooth.

Central giant-cell granuloma (CGCG) is a localised benign condition of the jaws. It is twice as common in females and is more likely to occur before age 30. Central giant-cell granulomas are more common in the anterior mandible, often crossing the midline and causing painless swellings.

An odontogenic keratocyst is a rare and benign but locally aggressive developmental cyst. It most often affects the posterior mandible and most commonly presents in the third decade of life. Odontogenic keratocysts make up around 19% of jaw cysts.
“Lateral periodontal cysts (LPCs) are defined as non-keratinised and non-inflammatory developmental cysts located adjacent or lateral to the root of a vital tooth.” LPCs are a rare form of jaw cysts, with the same histopathological characteristics as gingival cysts of adults (GCA). Hence LPCs are regarded as the intraosseous form of the extraosseous GCA. They are commonly found along the lateral periodontium or within the bone between the roots of vital teeth, around mandibular canines and premolars. Standish and Shafer reported the first well-documented case of LPCs in 1958, followed by Holder and Kunkel in the same year although it was called a periodontal cyst. Since then, there has been more than 270 well-documented cases of LPCs in literature.
Botryoid odontogenic cyst (BOC) is a type of developmental odontogenic cyst that is extremely rare. It is thought to be a lateral periodontal cyst (LPC) variant with a higher risk of recurrence. Weathers and Waldron coined the term BOC in 1973. Adults over the age of 50 are the most affected. BOC appears as a slow-growing lesion that is symptomatic in approximately 70% of cases.

Calcifying odontogenic cyst (COC) is a rare developmental lesion that comes from odontogenic epithelium. It is also known as a calcifying cystic odontogenic tumor, which is a proliferation of odontogenic epithelium and scattered nest of ghost cells and calcifications that may form the lining of a cyst, or present as a solid mass.

A glandular odontogenic cyst (GOC) is a rare and usually benign odontogenic cyst developed at the odontogenic epithelium of the mandible or maxilla. Originally, the cyst was labeled as "sialo-odontogenic cyst" in 1987. However, the World Health Organization (WHO) decided to adopt the medical expression "glandular odontogenic cyst". Following the initial classification, only 60 medically documented cases were present in the population by 2003. GOC was established as its own biological growth after differentiation from other jaw cysts such as the "central mucoepidermoid carcinoma (MEC)", a popular type of neoplasm at the salivary glands. GOC is usually misdiagnosed with other lesions developed at the glandular and salivary gland due to the shared clinical signs. The presence of osteodentin supports the concept of an odontogenic pathway. This odontogenic cyst is commonly described to be a slow and aggressive development. The inclination of GOC to be large and multilocular is associated with a greater chance of remission. GOC is an infrequent manifestation with a 0.2% diagnosis in jaw lesion cases. Reported cases show that GOC mainly impacts the mandible and male individuals. The presentation of GOC at the maxilla has a very low rate of incidence. The GOC development is more common in adults in their fifth and sixth decades.

An ameloblastic fibroma is a fibroma of the ameloblastic tissue, that is, an odontogenic tumor arising from the enamel organ or dental lamina. It may be either truly neoplastic or merely hamartomatous. In neoplastic cases, it may be labeled an ameloblastic fibrosarcoma in accord with the terminological distinction that reserves the word fibroma for benign tumors and assigns the word fibrosarcoma to malignant ones. It is more common in the first and second decades of life, when odontogenesis is ongoing, than in later decades. In 50% of cases an unerupted tooth is involved.
The calcifying epithelial odontogenic tumor (CEOT), also known as a Pindborg tumor, is an odontogenic tumor first recognized by the Danish pathologist Jens Jørgen Pindborg in 1955. It was previously described as an adenoid adamantoblastoma, unusual ameloblastoma and a cystic odontoma. Like other odontogenic neoplasms, it is thought to arise from the epithelial element of the enamel origin. It is a typically benign and slow growing, but invasive neoplasm.
Epulis is any tumor like enlargement situated on the gingival or alveolar mucosa. The word literally means "(growth) on the gingiva", and describes only the location of the mass and has no further implications on the nature of the lesion. There are three types: fibromatous, ossifying and acanthomatous. The related term parulis refers to a mass of inflamed granulation tissue at the opening of a draining sinus on the alveolus over the root of an infected tooth. Another closely related term is gingival enlargement, which tends to be used where the enlargement is more generalized over the whole gingiva rather than a localized mass.
Reverse smoking is a kind of smoking where the burnt end of a hand rolled tobacco leaf is put in the mouth rather than the unlit end of the cigar. It is practiced in some parts of Andhra Pradesh, India, Lusaka, Zambia and the Philippines. Reverse smoking is considered to be a risk factor for oral cancer.

Irritation fibroma is a type of fibroma that occurs on the mucosa of the oral cavity. Irritation fibromas are common benign tumors that are asymptomatic and resemble scarring. They are caused by prolonged irritation in the mouth, such as cheek or lip biting, rubbing from teeth, and dental prostheses.
The ameloblastic fibro-odontoma (AFO) is essentially a benign tumor with the features characteristic of ameloblastic fibroma along with enamel and dentin. Though it is generally regarded as benign, there have been cases of its malignant transformation into ameloblastic fibrosarcoma and odontogenic sarcoma. Cahn LR and Blum T, believed in "maturation theory", which suggested that AFO was an intermediate stage and eventually developed during the period of tooth formation to a complex odontoma thus, being a hamartoma.
References
- ↑ "Giant cell fibroma". DermNet. Retrieved November 23, 2023.
- 1 2 3 "Giant cell fibroma". Pathology Outlines. February 21, 2022. Retrieved November 23, 2023.
- 1 2 Sivaramakrishnan, M; Sabarinath, B; Sivapathasundharam, B (2012). "Giant cell fibroma: A clinicopathological study". Journal of Oral and Maxillofacial Pathology. Medknow. 16 (3): 359–362. doi: 10.4103/0973-029x.102485 . ISSN 0973-029X. PMC 3519210 . PMID 23248467.
- 1 2 Sonalika, Wanjari Ghate; Sahu, Anshuta; Deogade, Suryakant C.; Gupta, Pushkar; Naitam, Dinesh; Chansoria, Harsh; Agarwal, Jatin; Katoch, Shiva (2014). "Giant Cell Fibroma of Tongue: Understanding the Nature of an Unusual Histopathological Entity". Case Reports in Dentistry. Hindawi Limited. 2014: 1–4. doi: 10.1155/2014/864512 . ISSN 2090-6447. PMC 3910466 . PMID 24511398.
- ↑ Radhakrishnan, Raghu; Kulkarni, Spoorti; Chandrashekar, Chetana; Kudva, Ranjani (2017). "Giant-cell fibroma: Understanding the nature of the melanin-laden cells". Journal of Oral and Maxillofacial Pathology. Medknow. 21 (3): 429–433. doi: 10.4103/jomfp.jomfp_209_16 . ISSN 0973-029X. PMC 5763868 . PMID 29391720.
- ↑ Magnusson, Bengt C.; Rasmusson, Lars G. (1995). "The giant cell fibroma A review of 103 cases with immunohistochemical findings". Acta Odontologica Scandinavica. Informa UK Limited. 53 (5): 293–296. doi:10.3109/00016359509005990. ISSN 0001-6357. PMID 8553805 . Retrieved November 22, 2023.
- ↑ Nikitakis, Nikolaos G.; Emmanouil, Dimitris; Maroulakos, Michail P.; Angelopoulou, Matina V. (February 27, 2013). "Giant Cell Fibroma in Children: Report of Two Cases and Literature Review". Journal of Oral and Maxillofacial Research. Stilus Optimus. 4 (1): e5. doi: 10.5037/jomr.2013.4105 . ISSN 2029-283X. PMC 3886105 . PMID 24422028.
- ↑ Weathers, Dwight R.; Callihan, Michael D. (1974). "Giant-cell fibroma". Oral Surgery, Oral Medicine, Oral Pathology. Elsevier BV. 37 (3): 374–384. doi:10.1016/0030-4220(74)90110-8. ISSN 0030-4220. PMID 4521457 . Retrieved November 22, 2023.
- ↑ Houston, Glen D. (1982). "The giant cell fibroma". Oral Surgery, Oral Medicine, Oral Pathology. Elsevier BV. 53 (6): 582–587. doi:10.1016/0030-4220(82)90344-9. ISSN 0030-4220. PMID 6954437 . Retrieved November 22, 2023.