Conceptual development
Influential earlier concepts
A detailed case report in 1809 by John Haslam concerning James Tilly Matthews, [14] and a separate account by Philippe Pinel also published in 1809, are often regarded as the earliest cases of schizophrenia in the medical and psychiatric literature. [8] The Latinized term dementia praecox entered psychiatry in 1886 in a textbook by asylum physician Heinrich Schüle (1840–1916) of the Illenau asylum in Baden. He used the term to refer to hereditarily predisposed individuals who were "wrecked on the cliffs of puberty" and developed acute dementia, while others developed the chronic condition of hebephrenia. Emil Kraepelin had cited Schüle's 1886 textbook in the 1887 second edition of his own textbook, Psychiatrie, and hence was familiar with this term at least six years before he himself adopted it. [15] [16] It later appeared in 1891 in a case report by Arnold Pick which argued that hebephrenia should be regarded as a form of dementia praecox. Kraepelin first used the term in 1893. In 1899 Emil Kraepelin introduced a broad new distinction in the classification of mental disorders between dementia praecox and mood disorder (termed manic depression and including both unipolar and bipolar depression). Kraepelin believed that dementia praecox was caused by a lifelong, smoldering systemic or "whole body" process of a metabolic nature that would eventually affect the functioning of the brain in a final decisive cascade. Hence, he believed the entire body—all the organs, glands and peripheral nervous system—was implicated in the natural disease process. [17] Although he used the term "dementia," Kraepelin seemed to use the term synonymously with "mental weakness," mental defect," and "mental deterioration," but distinguished it from other uses of the term dementia, such as in Alzheimer's disease, which typically occur later in life. [18] In 1853 Bénédict Morel used the term démence précoce (precocious or early dementia) to describe a group of young patients who were affected by "stupor". [19] It is sometimes argued that this first use of the term signals the medical discovery of schizophrenia. However, Morel employed the phrase in a purely descriptive sense and he did not intend to delineate a new diagnostic category. Moreover, his traditional conception of dementia differed significantly from that employed in the latter half of the nineteenth-century. Finally, there is no evidence that Morel's démence précoce had any influence on the later development of the dementia praecox concept by either Arnold Pick or Emil Kraepelin. [5]
Kraepelin's classification slowly gained acceptance. There were objections to the use of the term "dementia" despite cases of recovery, and some defence of diagnoses it replaced such as adolescent insanity. [20] The concept of adolescent insanity or developmental insanity had been advanced by Scottish psychiatrist Sir Thomas Clouston in 1873, describing a psychotic condition which generally affected those aged 18–24 years, particularly males, and in 30% of cases proceeded to 'a secondary dementia'. [21]
Coinage in 1908 and after

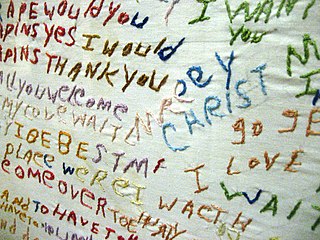
Paul Eugen Bleuler first used the term "schizophreniegruppe", on April 24, 1908, during a lecture at a meeting of the German Psychiatric Association in Berlin. [22] The word schizophrenia translates as "split mind" from the Greek roots schizein (σχίζειν, "to split") and phrēn, phren- (φρήν, φρεν-, "mind"). [23] Bleuler coined the term to more aptly describe the separation of function between personality, thinking, memory, and perception in his patients. [24] Bleuler later published his treatise on the subject, Dementia Praecox oder Gruppe der Schizophrenien, in 1911, [25] [26] which is recognised as his magnum opus. Bleuler's treatise describes the fundamental symptoms of the disorder of as four A's: [27] flattened Affect, Autism, impaired Association of ideas and Ambivalence. [24] Bleuler sought to differentiate schizophrenia as not a form of dementia, but an entirely separate disorder since his subjects did not suffer from loss or distortion of their memories. [28] [27] Bleuler wrote in 1911 of his terminology: [22]
I call dementia precox schizophrenia because, as I hope to show, the splitting of the different psychic functions is one of its most important features. In each case there is a more or less clear splitting of the psychological functions: as the disease becomes distinct, the personality loses its unity.
Attribution of credit for the origination of the concept
From the creation of the new term, at least two schools of thought arose after the acceptance of the idea. Some considered Bleuler had a lesser position of influence with the creation of a novel reality, and instead continued his own thoughts from the initial tradition of Kraeplin, that is, Bleuler inherited the idea, which he then developed. Others, finding Bleuler the greater of the two individuals, finds he discovered in fact the reality of the disorder anew, using Kraeplin's indication of the existence of disorder but that there was no knowably existing indication by Kraeplin of the new concept in the former earlier doctor's written observations and thoughts. [29]
First-rank symptoms
In the early 20th century, the psychiatrist Kurt Schneider listed the forms of psychotic symptoms that he thought distinguished schizophrenia from other psychotic disorders. He termed these as first-rank symptoms. They include delusions of being controlled by an external force; the belief that thoughts are being inserted into or withdrawn from one's conscious mind; the belief that one's thoughts are being broadcast to other people; and hearing hallucinatory voices that comment on one's thoughts or actions or that have a conversation with other hallucinated voices. [30] Although they have significantly contributed to the current diagnostic criteria, the specificity of first-rank symptoms has been questioned. A review of the diagnostic studies conducted between 1970 and 2005 found that they allow neither a reconfirmation nor a rejection of Schneider's claims, and suggested that first-rank symptoms should be de-emphasized in future revisions of diagnostic systems. [31]
Deviation from the intended meaning
Many people after the 1908 inception of the term did not accept that schizo-, splitting or dissociation was an appropriate description, and the term would later have more significance as a source of confusion and social stigma than scientific meaning. [28] In popular culture, the term schizophrenia is often thought to mean that affected persons have a "split personality". But for contemporary psychiatry, schizophrenia does not involve a person changing among distinct multiple personalities. The stigmatising confusion arises in part due to Bleuler's own use of the term schizophrenia, which for many signalled a split mind, and his documenting of a number of cases with split personalities within his classic 1911 description of schizophrenia. The earliest known use of the term to mean "split personality" was by psychologist G. Stanley Hall in 1916, and many early 20th-century psychiatrists and psychologists can also be found using the term in this sense (some reference Jekyll and Hyde) before a later rejection of this usage took place. The term schizophrenia used to be associated with split personality by the general population but that usage went into decline when split personality became known as a separate disorder, first as multiple personality disorder, and later as dissociative identity disorder. [32]