Related Research Articles

The endocrine system is a messenger system comprising feedback loops of the hormones released by internal glands of an organism directly into the circulatory system, regulating distant target organs. In vertebrates, the hypothalamus is the neural control center for all endocrine systems. In humans, the major endocrine glands are the thyroid gland and the adrenal glands. The study of the endocrine system and its disorders is known as endocrinology.

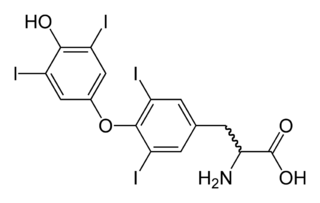
The thyroid, or thyroid gland, is an endocrine gland in vertebrates. In humans it is in the neck and consists of two connected lobes. The lower two thirds of the lobes are connected by a thin band of tissue called the thyroid isthmus. The thyroid is located at the front of the neck, below the Adam's apple. Microscopically, the functional unit of the thyroid gland is the spherical thyroid follicle, lined with follicular cells (thyrocytes), and occasional parafollicular cells that surround a lumen containing colloid. The thyroid gland secretes three hormones: the two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – and a peptide hormone, calcitonin. The thyroid hormones influence the metabolic rate and protein synthesis, and in children, growth and development. Calcitonin plays a role in calcium homeostasis. Secretion of the two thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is secreted from the anterior pituitary gland. TSH is regulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus.

In vertebrate anatomy, the pituitary gland, or hypophysis, is an endocrine gland, about the size of a pea and weighing 0.5 grams (0.018 oz) in humans. It is a protrusion off the bottom of the hypothalamus at the base of the brain. The hypophysis rests upon the hypophysial fossa of the sphenoid bone in the center of the middle cranial fossa and is surrounded by a small bony cavity covered by a dural fold. The anterior pituitary is a lobe of the gland that regulates several physiological processes. The intermediate lobe synthesizes and secretes melanocyte-stimulating hormone. The posterior pituitary is a lobe of the gland that is functionally connected to the hypothalamus by the median eminence via a small tube called the pituitary stalk.
Hypothyroidism is a disorder of the endocrine system in which the thyroid gland does not produce enough thyroid hormone. It can cause a number of symptoms, such as poor ability to tolerate cold, a feeling of tiredness, constipation, slow heart rate, depression, and weight gain. Occasionally there may be swelling of the front part of the neck due to goiter. Untreated cases of hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby or congenital iodine deficiency syndrome.

Thyrotropin-releasing hormone (TRH) is a hypophysiotropic hormone produced by neurons in the hypothalamus that stimulates the release of thyroid-stimulating hormone (TSH) and prolactin from the anterior pituitary.
Thyroid-stimulating hormone (also known as thyrotropin, thyrotropic hormone, or abbreviated TSH) is a pituitary hormone that stimulates the thyroid gland to produce thyroxine (T4), and then triiodothyronine (T3) which stimulates the metabolism of almost every tissue in the body. It is a glycoprotein hormone produced by thyrotrope cells in the anterior pituitary gland, which regulates the endocrine function of the thyroid.
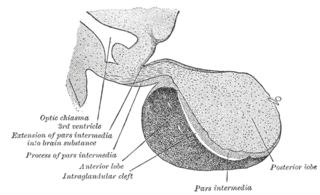
A major organ of the endocrine system, the anterior pituitary is the glandular, anterior lobe that together with the posterior lobe makes up the pituitary gland (hypophysis). The anterior pituitary regulates several physiological processes, including stress, growth, reproduction, and lactation. Proper functioning of the anterior pituitary and of the organs it regulates can often be ascertained via blood tests that measure hormone levels.
The posterior pituitary is the posterior lobe of the pituitary gland which is part of the endocrine system. The posterior pituitary is not glandular as is the anterior pituitary. Instead, it is largely a collection of axonal projections from the hypothalamus that terminate behind the anterior pituitary, and serve as a site for the secretion of neurohypophysial hormones directly into the blood. The hypothalamic–neurohypophyseal system is composed of the hypothalamus, posterior pituitary, and these axonal projections.

Hypopituitarism is the decreased (hypo) secretion of one or more of the eight hormones normally produced by the pituitary gland at the base of the brain. If there is decreased secretion of one specific pituitary hormone, the condition is known as selective hypopituitarism. If there is decreased secretion of most or all pituitary hormones, the term panhypopituitarism is used.
Optic nerve hypoplasia (ONH) is a medical condition arising from the underdevelopment of the optic nerve(s). This condition is the most common congenital optic nerve anomaly. The optic disc appears abnormally small, because not all the optic nerve axons have developed properly. It is often associated with endocrinopathies, developmental delay, and brain malformations. The optic nerve, which is responsible for transmitting visual signals from the retina to the brain, has approximately 1.2 million nerve fibers in the average person. In those diagnosed with ONH, however, there are noticeably fewer nerves.

Endocrine glands are ductless glands of the endocrine system that secrete their products, hormones, directly into the blood. The major glands of the endocrine system include the pineal gland, pituitary gland, pancreas, ovaries, testes, thyroid gland, parathyroid gland, hypothalamus and adrenal glands. The hypothalamus and pituitary glands are neuroendocrine organs.
Neuroendocrine cells are cells that receive neuronal input and, as a consequence of this input, release message molecules (hormones) into the blood. In this way they bring about an integration between the nervous system and the endocrine system, a process known as neuroendocrine integration. An example of a neuroendocrine cell is a cell of the adrenal medulla, which releases adrenaline to the blood. The adrenal medullary cells are controlled by the sympathetic division of the autonomic nervous system. These cells are modified postganglionic neurons. Autonomic nerve fibers lead directly to them from the central nervous system. The adrenal medullary hormones are kept in vesicles much in the same way neurotransmitters are kept in neuronal vesicles. Hormonal effects can last up to ten times longer than those of neurotransmitters. Sympathetic nerve fiber impulses stimulate the release of adrenal medullary hormones. In this way the sympathetic division of the autonomic nervous system and the medullary secretions function together.
Releasing hormones and inhibiting hormones are hormones whose main purpose is to control the release of other hormones, either by stimulating or inhibiting their release. They are also called liberins and statins (respectively), or releasing factors and inhibiting factors. The examples are hypothalamic-pituitary hormones that can be classified from several viewpoints: they are hypothalamic hormones, they are hypophysiotropic hormones, and they are tropic hormones.
Neuroendocrinology is the branch of biology which studies the interaction between the nervous system and the endocrine system; i.e. how the brain regulates the hormonal activity in the body. The nervous and endocrine systems often act together in a process called neuroendocrine integration, to regulate the physiological processes of the human body. Neuroendocrinology arose from the recognition that the brain, especially the hypothalamus, controls secretion of pituitary gland hormones, and has subsequently expanded to investigate numerous interconnections of the endocrine and nervous systems.

The hypophyseal portal system is a system of blood vessels in the microcirculation at the base of the brain, connecting the hypothalamus with the anterior pituitary. Its main function is to quickly transport and exchange hormones between the hypothalamus arcuate nucleus and anterior pituitary gland. The capillaries in the portal system are fenestrated which allows a rapid exchange between the hypothalamus and the pituitary. The main hormones transported by the system include gonadotropin-releasing hormone, corticotropin-releasing hormone, growth hormone–releasing hormone, and thyrotropin-releasing hormone.

The hypothalamic–pituitary–thyroid axis is part of the neuroendocrine system responsible for the regulation of metabolism and also responds to stress.
Euthyroid sick syndrome (ESS) is a state of adaptation or dysregulation of thyrotropic feedback control wherein the levels of T3 and/or T4 are abnormal, but the thyroid gland does not appear to be dysfunctional. This condition may result from allostatic responses of hypothalamus-pituitary-thyroid feedback control, dyshomeostatic disorders, drug interferences, and impaired assay characteristics in critical illness.
Autoimmune hypophysitis is defined as inflammation of the pituitary gland due to autoimmunity.
Hypothalamic–pituitary hormones are hormones that are produced by the hypothalamus and pituitary gland. Although the organs in which they are produced are relatively small, the effects of these hormones cascade throughout the body. They can be classified as a hypothalamic–pituitary axis of which the adrenal (HPA), gonadal (HPG), thyroid (HPT), somatotropic (HPS), and prolactin (HPP) axes are branches.
Prior to the availability of sensitive TSH assays, thyrotropin releasing hormone or TRH stimulation tests were relied upon for confirming and assessing the degree of suppression in suspected hyperthyroidism. Typically, this stimulation test involves determining basal TSH levels and levels 15 to 30 minutes after an intravenous bolus of TRH. Normally, TSH would rise into the concentration range measurable with less sensitive TSH assays. Third generation TSH assays do not have this limitation and thus TRH stimulation is generally not required when third generation TSH assays are used to assess degree of suppression.
References
- 1 2 3 4 5 6 Sylvia L., A. (2004). Hypothalamic disease. In Editor-in-Chief: Luciano Martini (Ed.), Encyclopedia of endocrine diseases (pp. 678-687). New York: Elsevier. doi : 10.1016/B0-12-475570-4/00714-9
- 1 2 3 MedlinePlus Encyclopedia : Hypothalamic dysfunction
- ↑ Rehan, K. (2011). An Overview of the Hypothalamus The Endocrine System’s Link to the Nervous System. Retrieved from http://www.endocrineweb.com/endocrinology/overview-hypothalamus
- ↑ Carmichael, J. D., & Braunstein, G. D. (2009). Diseases of Hypothalamic Origin. In D. W. Pfaff, A. P. Arnold, S. E. Fahrbach, A. M. Etgen & R. T. Rubin (Eds.), Hormones, Brain and Behavior (3005-3048). Los Angeles, CA: Academic Press
- 1 2 3 Rose, S. R., & Auble, B. A. (2011). Endocrine changes after pediatric traumatic brain injury. Pituitary, doi : 10.1007/s11102-011-0360-x
- 1 2 Maghnie, M., Altobelli, M., Di Iorgi, N., Genovese, E., Meloni, G., Manca-Bitti, M. L., . . . Bernasconi, S. (2004). Idiopathic central diabetes insipidus is associated with abnormal blood supply to the posterior pituitary gland caused by vascular impairment of the inferior hypophyseal artery system. The Journal of Clinical Endocrinology and Metabolism, 89(4), 1891-1896.
- 1 2 Martin, J. B., & Riskind, P. N. (1992). Neurologic manifestations of hypothalamic disease. Progress in Brain Research, 93, 31-40; discussion 40-2.
- ↑ Chiamolera, M. I., & Wondisford, F. E. (2009). Minireview: Thyrotropin-releasing hormone and the thyroid hormone feedback mechanism. Endocrinology, 150(3), 1091-1096. doi : 10.1210/en.2008-1795
- ↑ Pinkney, J. (2000). Obesity and pituitary disease. Pituitary News, 17. Retrieved from http://www.pituitary.org.uk/content/view/166/122/ Archived 2012-01-20 at the Wayback Machine
- ↑ Stores G (2003). "Misdiagnosing sleep disorders as primary psychiatric conditions". Advances in Psychiatric Treatment. 9 (1): 69–77. doi: 10.1192/apt.9.1.69 .
- ↑ Stores G (2007). "Clinical diagnosis and misdiagnosis of sleep disorders". J. Neurol. Neurosurg. Psychiatry. 78 (12): 1293–7. doi:10.1136/jnnp.2006.111179. PMC 2095611 . PMID 18024690.