The spermatic cord is the cord-like structure in males formed by the vas deferens and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an extension of the peritoneum that passes through the transversalis fascia. Each testicle develops in the lower thoracic and upper lumbar region and migrates into the scrotum. During its descent it carries along with it the vas deferens, its vessels, nerves etc. There is one on each side.

The cremaster muscle is a paired structure made of thin layers of striated and smooth muscle that covers the testicles and the spermatic cords in human males. It consists of the lateral and medial parts. Cremaster is an involuntary muscle, responsible for the cremasteric reflex; a protective and physiologic superficial reflex of the testicles. The reflex raises and lowers the testicles in order to keep them protected. Along with the dartos muscle of the scrotum, it regulates testicular temperature, thus aiding the process of spermatogenesis.

The genitofemoral nerve is a mixed branch of the lumbar plexus derived from anterior rami of L1-L2. It splits a genital branch and a femoral branch. It provides sensory innervation to the upper anterior thigh, as well as the skin of the anterior scrotum in males and mons pubis in females. It also provides motor innervation to the cremaster muscle.
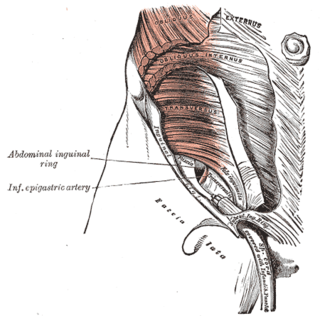
An inguinal hernia or groin hernia is a hernia (protrusion) of abdominal cavity contents through the inguinal canal. Symptoms, which may include pain or discomfort especially with or following coughing, exercise, or bowel movements, are absent in about a third of patients. Symptoms often get worse throughout the day and improve when lying down. A bulging area may occur that becomes larger when bearing down. Inguinal hernias occur more often on the right than left side. The main concern is strangulation, where the blood supply to part of the intestine is blocked. This usually produces severe pain and tenderness of the area.

The inguinal ligament, also known as Poupart's ligament or groin ligament, is a band running from the pubic tubercle to the anterior superior iliac spine. It forms the base of the inguinal canal through which an indirect inguinal hernia may develop.

The external iliac arteries are two major arteries which bifurcate off the common iliac arteries anterior to the sacroiliac joint of the pelvis.
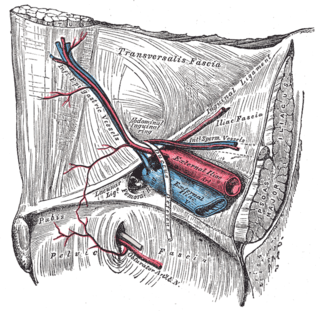
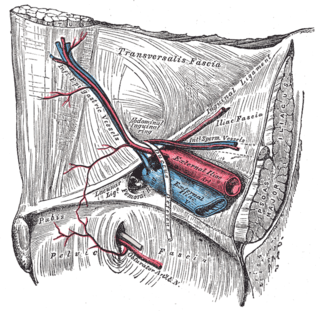
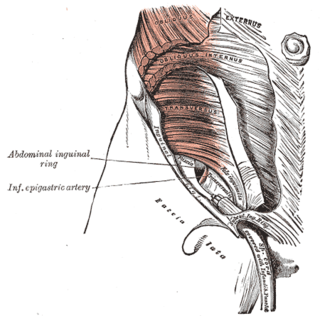
In human anatomy, the inferior epigastric artery is an artery that arises from the external iliac artery. It is accompanied by the inferior epigastric vein; inferiorly, these two inferior epigastric vessels together travel within the lateral umbilical fold The inferior epigastric artery then traverses the arcuate line of rectus sheath to enter the rectus sheath, then anastomoses with the superior epigastric artery within the rectus sheath.

The lumbar plexus is a web of nerves in the lumbar region of the body which forms part of the larger lumbosacral plexus. It is formed by the divisions of the first four lumbar nerves (L1-L4) and from contributions of the subcostal nerve (T12), which is the last thoracic nerve. Additionally, the ventral rami of the fourth lumbar nerve pass communicating branches, the lumbosacral trunk, to the sacral plexus. The nerves of the lumbar plexus pass in front of the hip joint and mainly support the anterior part of the thigh.

The ilioinguinal nerve is a branch of the first lumbar nerve (L1). It separates from the first lumbar nerve along with the larger iliohypogastric nerve. It emerges from the lateral border of the psoas major just inferior to the iliohypogastric, and passes obliquely across the quadratus lumborum and iliacus. The ilioinguinal nerve then perforates the transversus abdominis near the anterior part of the iliac crest, and communicates with the iliohypogastric nerve between the transversus and the internal oblique muscle.

The conjoint tendon is a sheath of connective tissue formed from the lower part of the common aponeurosis of the abdominal internal oblique muscle and the transversus abdominis muscle, joining the muscle to the pelvis. It forms the medial part of the posterior wall of the inguinal canal.
In human anatomy, the inguinal region refers to either the groin or the lower lateral regions of the abdomen. It may also refer to:
The transversalis fascia is the fascial lining of the anterolateral abdominal wall situated between the inner surface of the transverse abdominal muscle, and the preperitoneal fascia. It is directly continuous with the iliac fascia, the internal spermatic fascia, and pelvic fascia.

The fascia of Scarpa is the deep membranous layer (stratum membranosum) of the superficial fascia of the abdomen. It is a layer of the anterior abdominal wall. It is found deep to the fascia of Camper and superficial to the external oblique muscle.

The fascia of Camper is a thick superficial layer of the anterior abdominal wall.

The lateral umbilical fold is an elevation of the peritoneum lining the inner/posterior surface of the lower anterior abdominal wall formed by the underlying inferior epigastric artery and inferior epigastric vein which the peritoneum covers. Superiorly, the lateral umbilical fold ends where the vessels reach and enter the rectus sheath at the arcuate line of rectus sheath; in spite of the name, the lateral umbilical folds do not extend as far superiorly as the umbilicus. Inferiorly, it extends to just medial to the deep inguinal ring.

The cremasteric artery is a branch of the inferior epigastric artery which accompanies the spermatic cord to supply the cremaster muscle as well as other coverings of the spermatic cord in the male.

The medial umbilical ligament, cord of umbilical artery, or obliterated umbilical artery is a paired structure found in human anatomy. It is on the deep surface of the anterior abdominal wall, and is covered by the medial umbilical folds. It is different from the median umbilical ligament, a structure that represents the remnant of the embryonic urachus.
The cremasteric fascia is a fascia in the scrotum. As the cremaster descends, it forms a series of loops which differ in thickness and length in different subjects. At the upper part of the cord the loops are short, but they become in succession longer and longer, the longest reaching down as low as the testis, where a few are inserted into the tunica vaginalis. These loops are united together by areolar tissue, and form a thin covering over the cord and testis, the cremasteric fascia.

The superficial inguinal ring is bounded below by the crest of the pubis; on either side by the margins of the opening in the aponeurosis, which are called the crura of the ring; and above, by a series of curved intercrural fibers.

The genital branch of the genitofemoral nerve, also known as the external spermatic nerve in males, is a nerve in the abdomen that arises from the genitofemoral nerve. The genital branch supplies the cremaster muscle and anterior scrotal skin in males, and the skin of the mons pubis and labia majora in females.