The peritoneum is the serous membrane forming the lining of the abdominal cavity or coelom in amniotes and some invertebrates, such as annelids. It covers most of the intra-abdominal organs, and is composed of a layer of mesothelium supported by a thin layer of connective tissue. This peritoneal lining of the cavity supports many of the abdominal organs and serves as a conduit for their blood vessels, lymphatic vessels, and nerves.
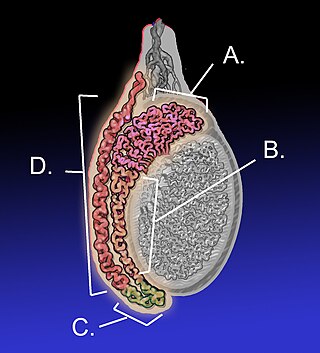
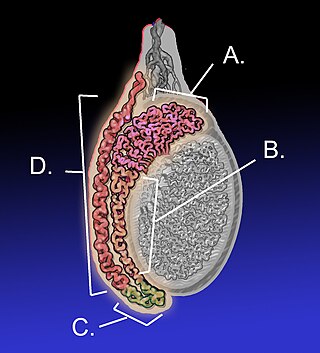
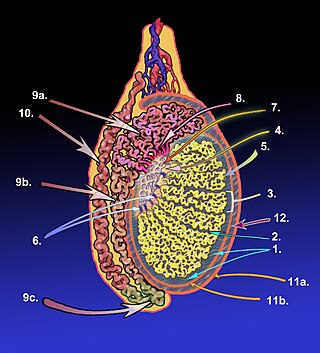
The epididymis is an elongated tubular structure attached to the posterior side of each one of the two male reproductive glands, the testicles. It is a single, narrow, tightly coiled tube in adult humans, 6 to 7 centimetres in length; uncoiled the tube would be approximately 6 m long. It connects the testicle to the vas deferens in the male reproductive system. The epididymis serves as an interconnection between the multiple efferent ducts at the rear of a testicle (proximally), and the vas deferens (distally). Its primary function is the storage, maturation and transport of sperm cells.

The vas deferens, with the more modern name ductus deferens, is part of the male reproductive system of many vertebrates. The ducts transport sperm from the epididymides to the ejaculatory ducts in anticipation of ejaculation. The vas deferens is a partially coiled tube which exits the abdominal cavity through the inguinal canal.

The spermatic cord is the cord-like structure in males formed by the vas deferens and surrounding tissue that runs from the deep inguinal ring down to each testicle. Its serosal covering, the tunica vaginalis, is an extension of the peritoneum that passes through the transversalis fascia. Each testicle develops in the lower thoracic and upper lumbar region and migrates into the scrotum. During its descent it carries along with it the vas deferens, its vessels, nerves etc. There is one on each side.

The cremaster muscle is a paired structure made of thin layers of striated and smooth muscle that covers the testicles and the spermatic cords in human males. It consists of the lateral and medial parts. Cremaster is an involuntary muscle, responsible for the cremasteric reflex; a protective and physiologic superficial reflex of the testicles. The reflex raises and lowers the testicles in order to keep them protected. Along with the dartos muscle of the scrotum, it regulates testicular temperature, thus aiding the process of spermatogenesis.

The inguinal canal is a passage in the anterior abdominal wall on each side of the body, which in males, convey the spermatic cords and in females, the round ligament of the uterus. The inguinal canals are larger and more prominent in males.

A hydrocele testis is an accumulation of clear fluid within the cavum vaginale, the potential space between the layers of the tunica vaginalis of the testicle. It is the most common form of hydrocele and is often referred to simply as a "hydrocele". A primary hydrocele testis causes a painless enlargement in the scrotum on the affected side and is thought to be due to the defective absorption of fluid secreted between the two layers of the tunica vaginalis. A secondary hydrocele is secondary to either inflammation or a neoplasm in the testis.

The genitofemoral nerve is a mixed branch of the lumbar plexus derived from anterior rami of L1-L2. It splits a genital branch and a femoral branch. It provides sensory innervation to the upper anterior thigh, as well as the skin of the anterior scrotum in males and mons pubis in females. It also provides motor innervation to the cremaster muscle.

A hydrocele is an accumulation of serous fluid in a body cavity. A hydrocele testis, the most common form of hydrocele, is the accumulation of fluids around a testicle. It is often caused by fluid collecting within a layer wrapped around the testicle, called the tunica vaginalis, which is derived from peritoneum. Provided there is no hernia present, it goes away without treatment in the first year. Although hydroceles usually develop in males, rare instances have been described in females in the canal of Nuck.
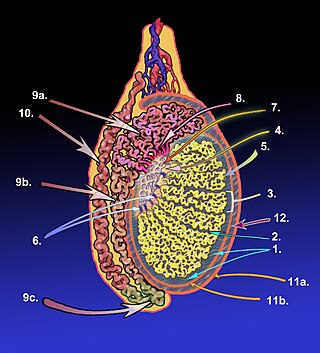
The tunica albuginea is a dense, blue-white layer of fibrous tissue surrounding the testis. It is the middle of three envelopes forming the capsule of the testis; it is deep to the visceral layer of tunica vaginalis, and superficial to the tunica vasculosa testis.

The lateral umbilical fold is an elevation of the peritoneum lining the inner/posterior surface of the lower anterior abdominal wall formed by the underlying inferior epigastric artery and inferior epigastric vein which the peritoneum covers. Superiorly, the lateral umbilical fold ends where the vessels reach and enter the rectus sheath at the arcuate line of rectus sheath; in spite of the name, the lateral umbilical folds do not extend as far superiorly as the umbilicus. Inferiorly, it extends to just medial to the deep inguinal ring.

The testicular artery is a branch of the abdominal aorta that supplies blood to the testicle. It is a paired artery, with one for each of the testicles.
The tunica vasculosa testis is the inner-most of the three layers that form the capsule of the testis. It consists of a vascular plexus and loose connective tissue. It extends into the testis itself to line the surfaces of individual septa of testis.

The cremasteric artery is a branch of the inferior epigastric artery which accompanies the spermatic cord to supply the cremaster muscle as well as other coverings of the spermatic cord in the male.

The artery to the ductus deferens is an artery in males that provides blood to the ductus deferens.
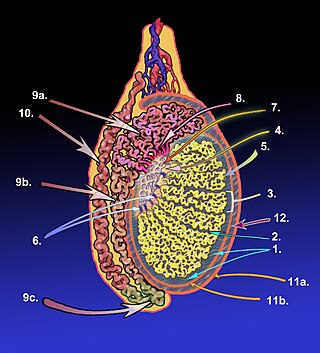
The mediastinum testis is a thick yet incomplete septum at the posterior part of the testis formed by the tunica albuginea of testis projecting into the testis at its posterior aspect where the testis is not lined by the serous membrane to allow for the attachment of the epididymis. It extends posteriorly between the testis' superior pole and inferior pole. It is wider superiorly than inferiorly. It supports the rete testis and blood and lymphatic vessels of the testis in their passage into and out of the substance of the gland.

The vaginal process is an embryonic developmental outpouching of the parietal peritoneum. It is present from around the 12th week of gestation, and commences as a peritoneal outpouching.
The development of the gonads is part of the prenatal development of the reproductive system and ultimately forms the testicles in males and the ovaries in females. The immature ova originate from cells from the dorsal endoderm of the yolk sac. Once they have reached the gonadal ridge they are called oogonia. Development proceeds and the oogonia become fully surrounded by a layer of connective tissue cells. In this way, the rudiments of the ovarian follicles are formed.

In most terrestrial mammals, the scrotum or scrotal sac is a part of the external male genitalia located at the base of the penis. It consists of a sac of skin containing the external spermatic fascia, testicles, epididymides, and vasa deferentia. The scrotum will usually tighten when exposed to cold temperatures.

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.