Related Research Articles

A medication is a drug used to diagnose, cure, treat, or prevent disease. Drug therapy (pharmacotherapy) is an important part of the medical field and relies on the science of pharmacology for continual advancement and on pharmacy for appropriate management.
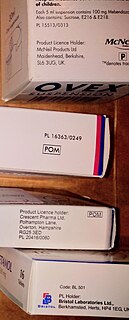
A prescription drug is a pharmaceutical drug that legally requires a medical prescription to be dispensed. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.

Rosiglitazone is an antidiabetic drug in the thiazolidinedione class. It works as an insulin sensitizer, by binding to the PPAR in fat cells and making the cells more responsive to insulin. It is marketed by the pharmaceutical company GlaxoSmithKline (GSK) as a stand-alone drug or for use in combination with metformin or with glimepiride. First released in 1999, annual sales peaked at approximately $2.5-billion in 2006; however, following a meta-analysis in 2007 that linked the drug's use to an increased risk of heart attack, sales plummeted to just $9.5-million in 2012. The drug's patent expired in 2012.
Many countries have measures in place to limit advertising by pharmaceutical companies.

Anti-obesity medication or weight loss medications are pharmacological agents that reduce or control weight. These medications alter one of the fundamental processes of the human body, weight regulation, by altering either appetite, or absorption of calories. The main treatment modalities for overweight and obese individuals remain dieting and physical exercise.
Polypharmacy (polypragmasia) is most commonly defined as the use of five or more medications daily by an individual. However, the definition of polypharmacy is still debated and can vary from two to 11 concurrent medications. Some studies also generally define polypharmacy as the use of multiple concurrent medications or simultaneous long term use of different drugs by the same individual.
Pharmacovigilance, also known as drug safety, is the pharmaceutical science relating to the collection, detection, assessment, monitoring, and prevention of adverse effects with pharmaceutical products. The etymological roots for the word "pharmacovigilance" are: pharmakon and vigilare. As such, pharmacovigilance heavily focuses on adverse drug reactions (ADR), which are defined as any response to a drug which is noxious and unintended, including lack of efficacy. Medication errors such as overdose, and misuse and abuse of a drug as well as drug exposure during pregnancy and breastfeeding, are also of interest, even without an adverse event, because they may result in an adverse drug reaction.
An adverse effect is an undesired harmful effect resulting from a medication or other intervention, such as surgery. An adverse effect may be termed a "side effect", when judged to be secondary to a main or therapeutic effect. If it results from an unsuitable or incorrect dosage or procedure, this is called a medical error and not a complication. Adverse effects are sometimes referred to as "iatrogenic" because they are generated by a physician/treatment. Some adverse effects occur only when starting, increasing or discontinuing a treatment. Adverse effects can also be caused by placebo treatments . Using a drug or other medical intervention which is contraindicated may increase the risk of adverse effects. Adverse effects may cause complications of a disease or procedure and negatively affect its prognosis. They may also lead to non-compliance with a treatment regimen. Adverse effects of medical treatment resulted in 142,000 deaths in 2013 up from 94,000 deaths in 1990 globally.

Off-label use is the use of pharmaceutical drugs for an unapproved indication or in an unapproved age group, dosage, or route of administration. Both prescription drugs and over-the-counter drugs (OTCs) can be used in off-label ways, although most studies of off-label use focus on prescription drugs.
A polypill is a medication that is a drug product in pill form that combines multiple active pharmaceutical ingredients. The prefix "poly" means "multiple", referring to the multiplicity of distinct drugs in a given "pill". An occasional synonym is combopill. It is commonly manufactured as a fixed-dose combination (FDC) drug product targeting treatment or prevention of chronic disease.
Computerized physician order entry (CPOE), sometimes referred to as computerized provider order entry or computerized provider order management (CPOM), is a process of electronic entry of medical practitioner instructions for the treatment of patients under his or her care.
In medicine, an indication is a valid reason to use a certain test, medication, procedure, or surgery. There can be multiple indications to use a procedure or medication. An indication can commonly be confused with the term diagnosis. A diagnosis is the assessment that a particular [medical] condition is present while an indication is a reason for use. The opposite of an indication is a contraindication, a reason to withhold a certain medical treatment because the risks of treatment clearly outweigh the benefits.
Pharmaceutical policy is a branch of health policy that deals with the development, provision and use of medications within a health care system. It embraces drugs, biologics, vaccines and natural health products.
Medication costs, also known as drug costs are a common health care cost for many people and health care systems. Prescription costs are the costs to the end consumer. Medication costs are influenced by multiple factors such as patents, stakeholder influence, and marketing expenses. A number of countries including Canada, parts of Europe, and Brasil use external reference pricing as a means to compare drug prices and to determine a base price for a particular medication. Other countries use pharmacoeconomics, which looks at the cost/benefit of a product in terms of quality of life, alternative treatments, and cost reduction or avoidance in other parts of the health care system. Structures like the UK's National Institute for Health and Clinical Excellence and to a lesser extent Canada's Common Drug Review evaluate products in this way.
Health information technology (HIT) is health technology, particularly information technology, applied to health and health care. It supports health information management across computerized systems and the secure exchange of health information between consumers, providers, payers, and quality monitors. Based on an often-cited 2008 report on a small series of studies conducted at four sites that provide ambulatory care – three U.S. medical centers and one in the Netherlands – the use of electronic health records (EHRs) was viewed as the most promising tool for improving the overall quality, safety and efficiency of the health delivery system.
The FDA Adverse Event Reporting System is a computerized information database designed to support the U.S. Food and Drug Administration's (FDA) postmarketing safety surveillance program for all approved drug and therapeutic biologic products. The FDA uses FAERS to monitor for new adverse events and medication errors that might occur with these products. It is a system that measures occasional harms from medications to ascertain whether the risk–benefit ratio is high enough to justify continued use of any particular drug and to identify correctable and preventable problems in health care delivery. The system interacts with several related systems including MedWatch and the Vaccine Adverse Event Reporting System. FAERS replaced legacy AERS system in Sep 2012.

The opioid epidemic is the extensive ongoing overuse of opioid medications, both from medical prescriptions and from illegal sources. The epidemic began in the United States in the late 1990s, according to the Centers for Disease Control and Prevention (CDC), when opioids were increasingly prescribed for pain management and resulted in a rise in overall opioid use throughout subsequent years. The great majority of Americans who use prescription opioids do not believe that they are misusing them.

The opioid epidemic, also referred to as the opioid crisis, is the phrase used to describe the overuse, misuse/abuse, and overdose deaths attributed either in part or in whole to the class of drugs opiates/opioids, and the significant medical, social, psychological, and economic consequences of the medical, non-medical, and recreational use of these medications.

Drug utilization review refers to a review of prescribing, dispensing, administering and ingesting of medication. This authorized, structured and ongoing review is related to pharmacy benefit managers. Drug use/ utilization evaluation and medication utilization evaluations are the same as drug utilization review.
When authorized medical personnel prescribe two or more medications together for the same condition or disease to the same patient, it is known as co-prescribing. When clinicians prescribe the opioid overdose drug naloxone to patients in conjunction with the patient's opioid prescriptions, or to patients at risk for opioid overdose, it is called a naloxone co-prescription. Due, in part, to the opioid epidemic in the United States, there are currently both a state-level and nation-wide movement in the medical and public policy fields to encourage, and sometimes require, naloxone co-prescribing. The U.S. government has issued guidelines recommending co-prescribing naloxone along with opioids. Some co-prescribing, e.g., the practice of co-prescribing benzodiazepines and certain opioid medications to patients, has been cause for concern due to the high risk of opioid overdose.
References
- 1 2 Brody, Howard; Light, Donald W (2011). "The Inverse Benefit Law: How Drug Marketing Undermines Patient Safety and Public Health". American Journal of Public Health. 101 (3): 399–404. doi:10.2105/AJPH.2010.199844. PMC 3036704 . PMID 21233426.
- ↑ "Worst Pill, Best Pill. Public Citizen's Health Research Group". Worstpills.org. Retrieved 2014-02-17.
- ↑ Wood, Alastair J. J (1999). "The Safety of New Medicines". JAMA. 281 (18): 1753–4. doi:10.1001/jama.281.18.1753. PMID 10328077.
- ↑ "Astellas' lawsuit against Prescrire: French court rules that Prescrire did not "denigrate" Protopic° (tacrolimus). Prescrire. 2 March 2011". English.prescrire.org. 2011-03-02. Retrieved 2014-02-17.
- ↑ Gérvas J. Garum. Acta Sanitaria. 07/03/2011.