The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

Pancreatitis is a condition characterized by inflammation of the pancreas. The pancreas is a large organ behind the stomach that produces digestive enzymes and a number of hormones. There are two main types: acute pancreatitis, and chronic pancreatitis.

Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. These cancerous cells have the ability to invade other parts of the body. A number of types of pancreatic cancer are known.

Acute pancreatitis (AP) is a sudden inflammation of the pancreas. Causes, in order of frequency, include: a gallstone impacted in the common bile duct beyond the point where the pancreatic duct joins it; heavy alcohol use; systemic disease; trauma; and, in children, mumps. Acute pancreatitis may be a single event; it may be recurrent; or it may progress to chronic pancreatitis and/or pancreatic failure.

Chronic pancreatitis is a long-standing inflammation of the pancreas that alters the organ's normal structure and functions. It can present as episodes of acute inflammation in a previously injured pancreas, or as chronic damage with persistent pain or malabsorption. It is a disease process characterized by irreversible damage to the pancreas as distinct from reversible changes in acute pancreatitis. Tobacco smoke and alcohol misuse are two of the most frequently implicated causes, and the two risk factors are thought to have a synergistic effect with regards to the development of chronic pancreatitis. Chronic pancreatitis is a risk factor for the development of pancreatic cancer.

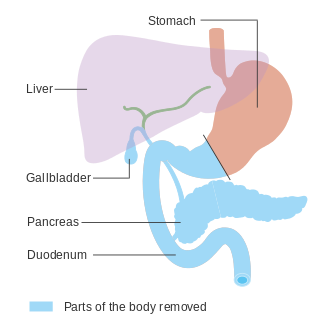
A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.
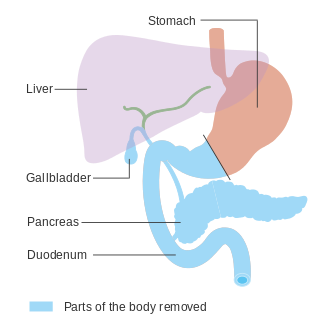
In medicine, a pancreatectomy is the surgical removal of all or part of the pancreas. Several types of pancreatectomy exist, including pancreaticoduodenectomy, distal pancreatectomy, segmental pancreatectomy, and total pancreatectomy. In recent years, the TP-IAT has also gained respectable traction within the medical community. These procedures are used in the management of several conditions involving the pancreas, such as benign pancreatic tumors, pancreatic cancer, and pancreatitis.

A pancreatic pseudocyst is a circumscribed collection of fluid rich in pancreatic enzymes, blood, and non-necrotic tissue, typically located in the lesser sac of the abdomen. Pancreatic pseudocysts are usually complications of pancreatitis, although in children they frequently occur following abdominal trauma. Pancreatic pseudocysts account for approximately 75% of all pancreatic masses.

Pancreas divisum is a congenital anomaly in the anatomy of the ducts of the pancreas in which a single pancreatic duct is not formed, but rather remains as two distinct dorsal and ventral ducts. Most individuals with pancreas divisum remain without symptoms or complications. A minority of people with pancreatic divisum may develop episodes of abdominal pain, nausea or vomiting due to acute or chronic pancreatitis. The presence of pancreas divisum is usually identified with cross sectional diagnostic imaging, such as endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP). In some cases, it may be detected intraoperatively. If no symptoms or complications are present, then treatment is not necessary. However, if there is recurrent pancreatitis, then a sphincterotomy of the minor papilla may be indicated.

Exocrine pancreatic insufficiency (EPI) is the inability to properly digest food due to a lack or reduction of digestive enzymes made by the pancreas. EPI can occur in humans and is prevalent in many conditions such as cystic fibrosis, Shwachman–Diamond syndrome, different types of pancreatitis, multiple types of diabetes mellitus, advanced renal disease, older adults, celiac disease, IBS-D, IBD, HIV, alcohol-related liver disease, Sjogren syndrome, tobacco use, and use of somatostatin analogues.

Hereditary pancreatitis (HP) is an inflammation of the pancreas due to genetic causes. It was first described in 1952 by Comfort and Steinberg but it was not until 1996 that Whitcomb et al isolated the first responsible mutation in the trypsinogen gene (PRSS1) on the long arm of chromosome seven (7q35).
Autoimmune Pancreatitis (AIP) is an increasingly recognized type of chronic pancreatitis that can be difficult to distinguish from pancreatic carcinoma but which responds to treatment with corticosteroids, particularly prednisone. Although autoimmune pancreatitis is quite rare, it constitutes an important clinical problem for both patients and their clinicians: the disease commonly presents itself as a tumorous mass which is diagnostically indistinguishable from pancreatic cancer, a disease that is much more common in addition to being very dangerous. Hence, some patients undergo pancreatic surgery, which is associated to substantial mortality and morbidity, out of the fear by patients and clinicians to undertreat a malignancy. However, surgery is not a good treatment for this condition as AIP responds well to immunosuppressive treatment. There are two categories of AIP: Type 1 and Type 2, each with distinct clinical profiles.
Markus Wolfgang Büchler is a German surgeon and university full professor. He specialises in gastrointestinal, hepatobiliary and transplant surgery, and is especially known for pioneering operations on the pancreas.

Pancreatic secretory trypsin inhibitor (PSTI) also known as serine protease inhibitor Kazal-type 1 (SPINK1) or tumor-associated trypsin inhibitor (TATI) is a protein that in humans is encoded by the SPINK1 gene.

Fat necrosis is a form of necrosis that is caused by the action of lipases on adipocytes.
Surgical Outcomes Analysis & Research, SOAR, is a research laboratory of the Department of Surgery at Boston University School of Medicine and Boston Medical Center with expertise in outcomes research. SOAR investigates surgical diseases and perioperative outcomes. The group focuses on pancreatic cancer, other gastrointestinal and hepatobiliary malignancies, vascular disease, and transplant surgery. SOAR's goal is to examine quality, delivery, and financing of care in order to have an immediate impact on patient care and system improvements. The group members utilize national health services and administrative databases, as well as institutional databases, to investigate and to address factors contributing to disease outcomes and healthcare disparities.

Intraductal papillary mucinous neoplasm (IPMN) is a type of tumor that can occur within the cells of the pancreatic duct. IPMN tumors produce mucus, and this mucus can form pancreatic cysts. Although intraductal papillary mucinous neoplasms are benign tumors, they can progress to pancreatic cancer. As such IPMN is viewed as a precancerous condition. Once an intraductal papillary mucinous neoplasm has been found, the management options include close monitoring and pre-emptive surgery.
The European Registry of Hereditary Pancreatitis and Pancreatic Cancer (EUROPAC) was started by John Neoptolemos and colleagues in 1997 and has become the world’s most extensive study on hereditary pancreatic diseases. It enabled discovery of several genetic characteristics causative for hereditary pancreatitis and familial pancreatic cancer.
Type 3c diabetes is diabetes that comes secondary to pancreatic diseases, involving the exocrine and digestive functions of the pancreas. It also occurs following surgical removal of the pancreas.
Lexipafant is a drug which acts as a potent and selective inhibitor of the phospholipid mediator platelet-activating factor (PAF). It was developed in the 1990s by British Biotech with several potential applications, including HIV-associated neurocognitive disorder and acute pancreatitis. Initial results were encouraging and it progressed as far as Phase III clinical trials, but final analysis of trial results showed that it failed to improve survival rates in pancreatitis despite some symptomatic improvement, and it was ultimately discontinued from development as a medicine, though it continues to be used as a model PAF inhibitor for pharmacology research.