Related Research Articles

Brain abscess is an abscess within the brain tissue caused by inflammation and collection of infected material coming from local or remote infectious sources. The infection may also be introduced through a skull fracture following a head trauma or surgical procedures. Brain abscess is usually associated with congenital heart disease in young children. It may occur at any age but is most frequent in the third decade of life.
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body. Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, or stroke.

A head injury is any injury that results in trauma to the skull or brain. The terms traumatic brain injury and head injury are often used interchangeably in the medical literature. Because head injuries cover such a broad scope of injuries, there are many causes—including accidents, falls, physical assault, or traffic accidents—that can cause head injuries.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

A subdural hematoma (SDH) is a type of bleeding in which a collection of blood—usually but not always associated with a traumatic brain injury—gathers between the inner layer of the dura mater and the arachnoid mater of the meninges surrounding the brain. It usually results from tears in bridging veins that cross the subdural space.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.

Epidural hematoma is when bleeding occurs between the tough outer membrane covering the brain and the skull. Often there is loss of consciousness following a head injury, a brief regaining of consciousness, and then loss of consciousness again. Other symptoms may include headache, confusion, vomiting, and an inability to move parts of the body. Complications may include seizures.
Monoplegia is paralysis of a single limb, usually an arm. Common symptoms associated with monoplegic patients are weakness, numbness, and pain in the affected limb. Monoplegia is a type of paralysis that falls under hemiplegia. While hemiplegia is paralysis of half of the body, monoplegia is localized to a single limb or to a specific region of the body. Monoplegia of the upper limb is sometimes referred to as brachial monoplegia, and that of the lower limb is called crural monoplegia. Monoplegia in the lower extremities is not as common of an occurrence as in the upper extremities. Monoparesis is a similar, but less severe, condition because one limb is very weak, not paralyzed. For more information, see paresis.

Intracerebral hemorrhage (ICH), also known as hemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is a type of bleeding within the skull and one kind of stroke. Symptoms can vary dramatically depending on the severity, acuity, and location (anatomically) but can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, neck stiffness, and fever.

Intraparenchymal hemorrhage (IPH) is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage (IVH).

Brain herniation is a potentially deadly side effect of very high pressure within the skull that occurs when a part of the brain is squeezed across structures within the skull. The brain can shift across such structures as the falx cerebri, the tentorium cerebelli, and even through the foramen magnum. Herniation can be caused by a number of factors that cause a mass effect and increase intracranial pressure (ICP): these include traumatic brain injury, intracranial hemorrhage, or brain tumor.
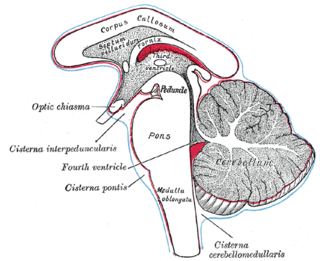
Duret haemorrhages are small linear areas of bleeding in the midbrain and upper pons of the brainstem. They are caused by a traumatic downward displacement of the brainstem.
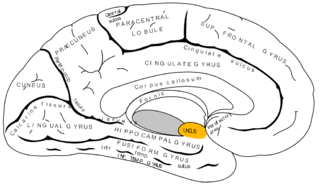
The uncus is an anterior extremity of the parahippocampal gyrus. It is separated from the apex of the temporal lobe by a slight fissure called the incisura temporalis.
In medicine, a mass effect is the effect of a growing mass that results in secondary pathological effects by pushing on or displacing surrounding tissue.
Central facial palsy is a symptom or finding characterized by paralysis or paresis of the lower half of one side of the face. It usually results from damage to upper motor neurons of the facial nerve.

Brown-Séquard syndrome is caused by damage to one half of the spinal cord, i.e. hemisection of the spinal cord resulting in paralysis and loss of proprioception on the same side as the injury or lesion, and loss of pain and temperature sensation on the opposite side as the lesion. It is named after physiologist Charles-Édouard Brown-Séquard, who first described the condition in 1850.
James Watson Kernohan, M.D. (1896–1981) was an Irish-American pathologist born October 1, 1896, in County Antrim, Ireland. He studied medicine at Queen's University Belfast, and in 1922 he emigrated to the United States and subsequently worked as a pathologist at the Mayo Clinic in Rochester, Minnesota. Kernohan retired from active medical practice in 1962 and died May 5, 1981.
Amorphosynthesis, also called a hemi-sensory deficit, is a neuropsychological condition in which a patient experiences unilateral inattention to sensory input. This phenomenon is frequently associated with damage to the right cerebral hemisphere resulting in severe sensory deficits that are observed on the contralesional (left) side of the body. A right-sided deficit is less commonly observed and the effects are reported to be temporary and minor. Evidence suggests that the right cerebral hemisphere has a dominant role in attention and awareness to somatic sensations through ipsilateral and contralateral stimulation. In contrast, the left cerebral hemisphere is activated only by contralateral stimuli. Thus, the left and right cerebral hemispheres exhibit redundant processing to the right-side of the body and a lesion to the left cerebral hemisphere can be compensated by the ipsiversive processes of the right cerebral hemisphere. For this reason, right-sided amorphosynthesis is less often observed and is generally associated with bilateral lesions.
A sports-related traumatic brain injury is a serious accident which may lead to significant morbidity or mortality. Traumatic brain injury (TBI) in sports are usually a result of physical contact with another person or stationary object, These sports may include boxing, gridiron football, field/ice hockey, lacrosse, martial arts, rugby, soccer, wrestling, auto racing, cycling, equestrian, rollerblading, skateboarding, skiing or snowboarding.

Raymond–Céstan syndrome is caused by blockage of the long circumferential branches of the basilar artery. It was described by Fulgence Raymond and Étienne Jacques Marie Raymond Céstan. Along with other related syndromes such as Millard–Gubler syndrome, Foville's syndrome, and Weber's syndrome, the description was instrumental in establishing important principles in brain-stem localization.
References
- Binder, D; Lyon R; Manley G (2004). "Transcranial motor evoked potential recording in a case of Kernohan's notch syndrome: Case report". Neurosurgery. 54 (4): 999–1002. doi:10.1227/01.NEU.0000115674.15497.09. PMID 15046669. S2CID 10308410.
- Boes, C; Kumar N; Swanson J (2007). "Comment on 'Kernohan's notch' by J. M. S. Pearce". European Neurology. 57 (4): 251. doi: 10.1159/000101294 . PMID 17389807.
- Collier, J (1904). "The false localizing signs of intracranial tumour". Brain. 27 (4): 490–508. doi:10.1093/brain/27.4.490.
- Fujimoto, A; Sato H; Katayama W; Nakai K; Tsunoda T (2004). "Kernohan's phenomenon associated with left ruptured occipital arteriovenous malformation". Journal of Clinical Neuroscience. 11 (4): 444–446. doi:10.1016/j.jocn.2002.09.003. PMID 15080971. S2CID 37615174.
- Gimenez-Pando, J; Cabezudo-Artero JM; Fernandez-Portales I; Rodriguez-Sanchez JA; Gomez-Perals L (2004). "Contralateral mesencephalic injury due to tentorial uncal herniation. Magnetic resonance imaging of the Kernohan's notch". Neurocirugia. 15 (4): 384–387. doi:10.1016/s1130-1473(04)70474-1. PMID 15368030.
- Jones, K; Seeger J; Yoshino M (1991). "Ipsilateral motor deficit resulting from a subdural hematoma and Kernohan notch". AJNR Am J Neuroradiol. 12 (6): 1238–1239. PMC 8331488 . PMID 1763762.
- Kernohan, J; Woltman H (1929). "Incisura of the crus due to contralateral brain tumour". Arch Neurol Psychiatry. 21 (2): 274–287. doi:10.1001/archneurpsyc.1929.02210200030004.
- Kole, M; Hysell S (2000). "MRI correlate of Kernohan's notch". Neurology. 55 (11): 1751. doi: 10.1212/wnl.55.11.1751 . PMID 11113240.
- Kunii, N; Morita A; Yoshikawa G; Kirino T (2005). "Subdural Hematoma Associated with Dural Metastasis - Case Report". Neurol Med Chir. 45 (10): 519–522. doi: 10.2176/nmc.45.519 . PMID 16247237.
- Lim, E; Yik J; Pek C; Seet R (2007). "Infratentorial meningioma causing ipsilateral hemiparesis: The other Kernohan's notch?". European Journal of Neurology. 14: 132–133. doi:10.1111/j.1468-1331.2007.01936.x.
- Meyer, A (1920). "Herniation of the brain". Arch Neurol Psychiatry. 4 (4): 387–400. doi:10.1001/archneurpsyc.1920.02180220036003.
- Milhorat, T; Marshall L; Marion D (2004). "Transcranial motor evoked potential recording in a case of Kernohan's notch syndrome: Case report". Neurosurgery. 54 (4): 1002–1003. doi:10.1227/01.neu.0000115674.15497.09. PMID 15046669. S2CID 10308410.
- Moon, K; Lee J; Joo S; Kim T; Jung S (2007). "Kernohan's notch phenomenon in chronic subdural hematoma: MRI findings". Journal of Clinical Neuroscience. 14 (10): 989–992. doi:10.1016/j.jocn.2006.05.016. PMID 17823049. S2CID 22983396.
- Pearce, J (2006). "Kernohan's notch". European Neurology. 55 (4): 230–232. doi: 10.1159/000093876 . S2CID 7258069.
- Pearce, J (2007). "Comment on 'Kernohan's notch' by J. M. S. Pearce - Reply". European Neurology. 57 (4): 252. doi: 10.1159/000101295 .
- Wolf, R; Weem C; Krikke A (1995). "Kernohan's notch and misdiagnosis". The Lancet. 345 (8944): 259–260. doi:10.1016/S0140-6736(95)90255-4. PMID 7823740. S2CID 44965102.