Hemiparesis, or unilateral paresis, is weakness of one entire side of the body. Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, Traumatic Brain Injury or stroke.

Ramsay Hunt syndrome type 2, commonly referred to simply as Ramsay Hunt syndrome (RHS) and also known as herpes zoster oticus, is inflammation of the geniculate ganglion of the facial nerve as a late consequence of varicella zoster virus (VZV). In regard to the frequency, less than 1% of varicella zoster infections involve the facial nerve and result in RHS. It is traditionally defined as a triad of ipsilateral facial paralysis, otalgia, and vesicles close to the ear and auditory canal. Due to its proximity to the vestibulocochlear nerve, the virus can spread and cause hearing loss, tinnitus, and vertigo. It is common for diagnoses to be overlooked or delayed, which can raise the likelihood of long-term consequences. It is more complicated than Bell's palsy. Therapy aims to shorten its overall length, while also providing pain relief and averting any consequences.
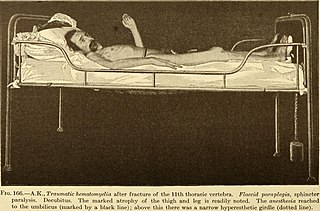
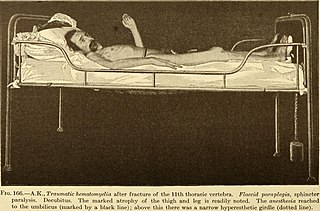
Paraplegia, or paraparesis, is an impairment in motor or sensory function of the lower extremities. The word comes from Ionic Greek (παραπληγίη) "half-stricken". It is usually caused by spinal cord injury or a congenital condition that affects the neural (brain) elements of the spinal canal. The area of the spinal canal that is affected in paraplegia is either the thoracic, lumbar, or sacral regions. If four limbs are affected by paralysis, tetraplegia or quadriplegia is the correct term. If only one limb is affected, the correct term is monoplegia. Spastic paraplegia is a form of paraplegia defined by spasticity of the affected muscles, rather than flaccid paralysis.

Myoclonus is a brief, involuntary, irregular twitching of a muscle, a joint, or a group of muscles, different from clonus, which is rhythmic or regular. Myoclonus describes a medical sign and, generally, is not a diagnosis of a disease. It belongs to the hyperkinetic movement disorders, among tremor and chorea for example. These myoclonic twitches, jerks, or seizures are usually caused by sudden muscle contractions or brief lapses of contraction. The most common circumstance under which they occur is while falling asleep. Myoclonic jerks occur in healthy people and are experienced occasionally by everyone. However, when they appear with more persistence and become more widespread they can be a sign of various neurological disorders. Hiccups are a kind of myoclonic jerk specifically affecting the diaphragm. When a spasm is caused by another person it is known as a provoked spasm. Shuddering attacks in babies fall in this category.
Dysarthria is a speech sound disorder resulting from neurological injury of the motor component of the motor–speech system and is characterized by poor articulation of phonemes. In other words, it is a condition in which problems effectively occur with the muscles that help produce speech, often making it very difficult to pronounce words. It is unrelated to problems with understanding language, although a person can have both. Any of the speech subsystems can be affected, leading to impairments in intelligibility, audibility, naturalness, and efficiency of vocal communication. Dysarthria that has progressed to a total loss of speech is referred to as anarthria. The term dysarthria was formed from the Greek components dys- "dysfunctional, impaired" and arthr- "joint, vocal articulation".
Astasis is a lack of motor coordination marked by an inability to stand, walk or even sit without assistance due to disruption of muscle coordination.

Mirror therapy (MT) or mirror visual feedback (MVF) is a therapy for pain or disability that affects one side of the patient more than the other side. It was invented by Vilayanur S. Ramachandran to treat post-amputation patients who had phantom limb pain (PLP). Ramachandran created a visual illusion of two intact limbs by putting the patient's affected limb into a "mirror box," with a mirror down the center.
Hemiballismus or hemiballism is a basal ganglia syndrome resulting from damage to the subthalamic nucleus in the basal ganglia. Hemiballismus is a rare hyperkinetic movement disorder, that is characterized by violent involuntary limb movements, on one side of the body, and can cause significant disability. Ballismus affects both sides of the body and is much rarer. Symptoms can decrease during sleep.

Brain herniation is a potentially deadly side effect of very high pressure within the skull that occurs when a part of the brain is squeezed across structures within the skull. The brain can shift across such structures as the falx cerebri, the tentorium cerebelli, and even through the foramen magnum. Herniation can be caused by a number of factors that cause a mass effect and increase intracranial pressure (ICP): these include traumatic brain injury, intracranial hemorrhage, or brain tumor.

Sixth nerve palsy, or abducens nerve palsy, is a disorder associated with dysfunction of cranial nerve VI, which is responsible for causing contraction of the lateral rectus muscle to abduct the eye. The inability of an eye to turn outward, results in a convergent strabismus or esotropia of which the primary symptom is diplopia in which the two images appear side-by-side. Thus, the diplopia is horizontal and worse in the distance. Diplopia is also increased on looking to the affected side and is partly caused by overaction of the medial rectus on the unaffected side as it tries to provide the extra innervation to the affected lateral rectus. These two muscles are synergists or "yoke muscles" as both attempt to move the eye over to the left or right. The condition is commonly unilateral but can also occur bilaterally.
Akinetic mutism is a medical condition where patients tend neither to move (akinesia) nor speak (mutism). Akinetic mutism was first described in 1941 as a mental state where patients lack the ability to move or speak. However, their eyes may follow their observer or be diverted by sound. Patients lack most motor functions such as speech, facial expressions, and gestures, but demonstrate apparent alertness. They exhibit reduced activity and slowness, and can speak in whispered monosyllables. Patients often show visual fixation on their examiner, move their eyes in response to an auditory stimulus, or move after often repeated commands. Patients with akinetic mutism are not paralyzed, but lack the will to move. Many patients describe that as soon as they "will" or attempt a movement, a "counter-will" or "resistance" rises up to meet them.

Foix–Chavany–Marie syndrome (FCMS), also known as bilateral opercular syndrome, is a neuropathological disorder characterized by paralysis of the facial, tongue, pharynx, and masticatory muscles of the mouth that aid in chewing. The disorder is primarily caused by thrombotic and embolic strokes, which cause a deficiency of oxygen in the brain. As a result, bilateral lesions may form in the junctions between the frontal lobe and temporal lobe, the parietal lobe and cortical lobe, or the subcortical region of the brain. FCMS may also arise from defects existing at birth that may be inherited or nonhereditary. Symptoms of FCMS can be present in a person of any age and it is diagnosed using automatic-voluntary dissociation assessment, psycholinguistic testing, neuropsychological testing, and brain scanning. Treatment for FCMS depends on the onset, as well as on the severity of symptoms, and it involves a multidisciplinary approach.
Vocal cord paresis, also known as recurrent laryngeal nerve paralysis or vocal fold paralysis, is an injury to one or both recurrent laryngeal nerves (RLNs), which control all intrinsic muscles of the larynx except for the cricothyroid muscle. The RLN is important for speaking, breathing and swallowing.

Cortical deafness is a rare form of sensorineural hearing loss caused by damage to the primary auditory cortex. Cortical deafness is an auditory disorder where the patient is unable to hear sounds but has no apparent damage to the structures of the ear. It has been argued to be as the combination of auditory verbal agnosia and auditory agnosia. Patients with cortical deafness cannot hear any sounds, that is, they are not aware of sounds including non-speech, voices, and speech sounds. Although patients appear and feel completely deaf, they can still exhibit some reflex responses such as turning their head towards a loud sound.

Central nervous system diseases or central nervous system disorders are a group of neurological disorders that affect the structure or function of the brain or spinal cord, which collectively form the central nervous system (CNS). These disorders may be caused by such things as infection, injury, blood clots, age related degeneration, cancer, autoimmune disfunction, and birth defects. The symptoms vary widely, as do the treatments.

A neurological disorder is any disorder of the nervous system. Structural, biochemical or electrical abnormalities in the brain, spinal cord or other nerves can result in a range of symptoms. Examples of symptoms include paralysis, muscle weakness, poor coordination, loss of sensation, seizures, confusion, pain, tauopathies, and altered levels of consciousness. There are many recognized neurological disorders, some are relatively common, but many are rare.

Orthotics is a medical specialty that focuses on the design and application of orthoses, sometimes known as braces or calipers. An orthosis is "an externally applied device used to influence the structural and functional characteristics of the neuromuscular and skeletal systems." Orthotists are professionals who specialize in designing these braces.
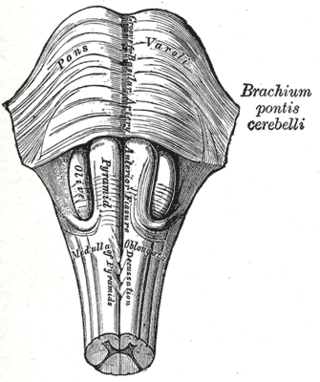
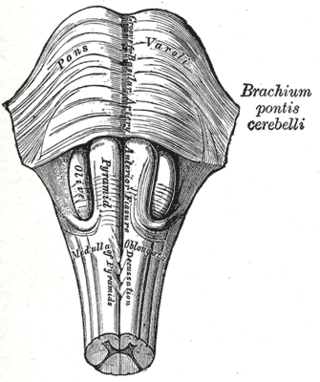
Babinski–Nageotte syndrome is an alternating brainstem syndrome. It occurs when there is damage to the dorsolateral or posterior lateral medulla oblongata, likely syphilitic in origin. Hence it is also called the alternating medulla oblongata syndrome.
Disorders of consciousness are medical conditions that inhibit consciousness. Some define disorders of consciousness as any change from complete self-awareness to inhibited or absent self-awareness and arousal. This category generally includes minimally conscious state and persistent vegetative state, but sometimes also includes the less severe locked-in syndrome and more severe but rare chronic coma. Differential diagnosis of these disorders is an active area of biomedical research. Finally, brain death results in an irreversible disruption of consciousness. While other conditions may cause a moderate deterioration or transient interruption of consciousness, they are not included in this category.
25. Injuries to the pons are the most common cause of locked-in syndrome,Harrison’s principles of internal medicine 21st edition vol 2 page 3332.