Modafinil, sold under the brand name Provigil among others, is a wakefulness-promoting medication used primarily to treat narcolepsy. Modafinil is also approved for stimulating wakefulness in people with sleep apnea and shift work sleep disorder. It is taken by mouth. Modafinil is not approved by the US Food and Drug Administration (FDA) for use in people under age 17.

A sleep disorder, or somnipathy, is a medical disorder of an individual's sleep patterns. Some sleep disorders are severe enough to interfere with normal physical, mental, social and emotional functioning. Sleep disorders are frequent and can have serious consequences on patients' health and quality of life. Polysomnography and actigraphy are tests commonly ordered for diagnosing sleep disorders.
Dyssomnias are a broad classification of sleeping disorders involving difficulty getting to sleep, remaining asleep, or of excessive sleepiness.
Somnolence is a state of strong desire for sleep, or sleeping for unusually long periods. It has distinct meanings and causes. It can refer to the usual state preceding falling asleep, the condition of being in a drowsy state due to circadian rhythm disorders, or a symptom of other health problems. It can be accompanied by lethargy, weakness and lack of mental agility.
Hypersomnia is a neurological disorder of excessive time spent sleeping or excessive sleepiness. It can have many possible causes and can cause distress and problems with functioning. In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), hypersomnolence, of which there are several subtypes, appears under sleep-wake disorders.
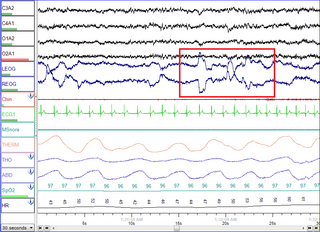
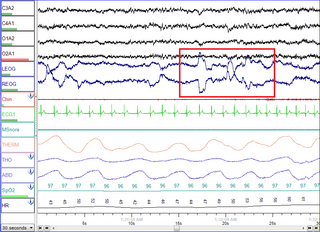
Polysomnography (PSG), a type of sleep study, is a multi-parameter study of sleep and a diagnostic tool in sleep medicine. The test result is called a polysomnogram, also abbreviated PSG. The name is derived from Greek and Latin roots: the Greek πολύς, the Latin somnus ("sleep"), and the Greek γράφειν.

Obstructive sleep apnea (OSA) is the most common sleep-related breathing disorder and is characterized by recurrent episodes of complete or partial obstruction of the upper airway leading to reduced or absent breathing during sleep. These episodes are termed "apneas" with complete or near-complete cessation of breathing, or "hypopneas" when the reduction in breathing is partial. In either case, a fall in blood oxygen saturation, a disruption in sleep, or both, may result. A high frequency of apneas or hypopneas during sleep may interfere with the quality of sleep, which – in combination with disturbances in blood oxygenation – is thought to contribute to negative consequences to health and quality of life. The terms obstructive sleep apnea syndrome (OSAS) or obstructive sleep apnea–hypopnea syndrome (OSAHS) may be used to refer to OSA when it is associated with symptoms during the daytime.

Somnology is the scientific study of sleep. It includes clinical study and treatment of sleep disorders and irregularities. Sleep medicine is a subset of somnology.
Cataplexy is a sudden and transient episode of muscle weakness accompanied by full conscious awareness, typically triggered by emotions such as laughing, crying, or terror. Cataplexy affects approximately 20% of people who have narcolepsy, and is caused by an autoimmune destruction of hypothalamic neurons that produce the neuropeptide hypocretin, which regulates arousal and has a role in stabilization of the transition between wake and sleep states. Cataplexy without narcolepsy is rare and the cause is unknown.

Armodafinil (trade name Nuvigil) is the enantiopure compound of the eugeroic modafinil (Provigil). It consists of only the (R)-(−)-enantiomer of the racemic modafinil. Armodafinil is produced by the pharmaceutical company Cephalon Inc. and was approved by the U.S. Food and Drug Administration (FDA) in June 2007. In 2016, the FDA granted Mylan rights for the first generic version of Cephalon's Nuvigil to be marketed in the U.S.
The Multiple Sleep Latency Test (MSLT) is a sleep disorder diagnostic tool. It is used to measure the time elapsed from the start of a daytime nap period to the first signs of sleep, called sleep latency. The test is based on the idea that the sleepier people are, the faster they will fall asleep.
The Epworth Sleepiness Scale (ESS) is a scale intended to measure daytime sleepiness that is measured by use of a very short questionnaire. This can be helpful in diagnosing sleep disorders. It was introduced in 1991 by Dr Murray Johns of Epworth Hospital in Melbourne, Australia.
Excessive daytime sleepiness (EDS) is characterized by persistent sleepiness and often a general lack of energy, even during the day after apparently adequate or even prolonged nighttime sleep. EDS can be considered as a broad condition encompassing several sleep disorders where increased sleep is a symptom, or as a symptom of another underlying disorder like narcolepsy, circadian rhythm sleep disorder, sleep apnea or idiopathic hypersomnia.

Sleep medicine is a medical specialty or subspecialty devoted to the diagnosis and therapy of sleep disturbances and disorders. From the middle of the 20th century, research has provided increasing knowledge of, and answered many questions about, sleep–wake functioning. The rapidly evolving field has become a recognized medical subspecialty in some countries. Dental sleep medicine also qualifies for board certification in some countries. Properly organized, minimum 12-month, postgraduate training programs are still being defined in the United States. In some countries, the sleep researchers and the physicians who treat patients may be the same people.

Sleep deprivation, also known as sleep insufficiency or sleeplessness, is the condition of not having adequate duration and/or quality of sleep to support decent alertness, performance, and health. It can be either chronic or acute and may vary widely in severity. All known animals sleep or exhibit some form of sleep behavior, and the importance of sleep is self-evident for humans, as nearly a third of a person's life is spent sleeping.

Narcolepsy is a chronic neurological disorder that involves a decreased ability to regulate sleep–wake cycles. Symptoms often include periods of excessive daytime sleepiness and brief involuntary sleep episodes. Narcolepsy paired with cataplexy is evidenced to be an autoimmune disorder. These experiences of cataplexy can be brought on by strong emotions. Less commonly, there may be vivid hallucinations or an inability to move while falling asleep or waking up. People with narcolepsy tend to sleep about the same number of hours per day as people without it, but the quality of sleep tends to be lessened.
Pitolisant, sold under the brand name Wakix among others, is a medication used for the treatment of excessive daytime sleepiness in adults with narcolepsy. It is a histamine 3 (H3) receptor antagonist/inverse agonist (an antihistamine drug specific to that kind of receptors). It represents the first commercially available medication in its class, so that the US Food and Drug Administration (FDA) declares it a first-in-class medication. Pitolisant enhances the activity of histaminergic neurons in the brain that function to improve a person's wakefulness.

Eugeroics, also known as wakefulness-promoting agents and wakefulness-promoting drugs, are a class of drugs that promote wakefulness and alertness. They are medically indicated for the treatment of certain sleep disorders including excessive daytime sleepiness (EDS) in narcolepsy or obstructive sleep apnea (OSA). Eugeroics are also often prescribed off-label for the treatment of EDS in idiopathic hypersomnia. In contrast to classical psychostimulants, such as methylphenidate and amphetamine, which are also used in the treatment of these disorders, eugeroics typically do not produce marked euphoria, and, consequently, have a lower addictive potential.
Idiopathic hypersomnia(IH) is a neurological disorder which is characterized primarily by excessive sleep and excessive daytime sleepiness (EDS). Idiopathic hypersomnia was first described in 1976, and it can be divided into two forms: polysymptomatic and monosymptomatic. The condition typically becomes evident in early adulthood and most patients diagnosed with IH will have had the disorder for many years prior to their diagnosis. As of August 2021, an FDA-approved medication exists for IH called Xywav, which is oral solution of calcium, magnesium, potassium, and sodium oxybates; in addition to several off-label treatments (primarily FDA-approved narcolepsy medications).

Solriamfetol, sold under the brand name Sunosi, is a wakefulness-promoting medication used in the treatment of excessive sleepiness related to narcolepsy and sleep apnea. It is taken by mouth.