Related Research Articles

Substance P (SP) is an undecapeptide and a type of neuropeptide, belongings to the tachykinin family of neuropeptides. It is acts as a neurotransmitter and a neuromodulator. Substance P and its closely related neurokinin A (NKA) are produced from a polyprotein precursor after alternative splicing of the preprotachykinin A gene. The deduced amino acid sequence of substance P is as follows:

Itch is a sensation that causes the desire or reflex to scratch. Itches have resisted many attempts to be classified as any one type of sensory experience. Itches have many similarities to pain, and while both are unpleasant sensory experiences, their behavioral response patterns are different. Pain creates a withdrawal reflex, whereas itches leads to a scratch reflex.

Rhinitis, also known as coryza, is irritation and inflammation of the mucous membrane inside the nose. Common symptoms are a stuffy nose, runny nose, sneezing, and post-nasal drip.
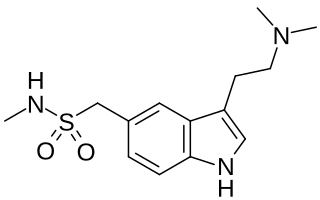
Sumatriptan, sold commonly under brand names Imitrex and Treximet among others, is a medication used to treat migraine headaches and cluster headaches. It is taken orally, intranasally, or by subcutaneous injection. Therapeutic effects generally occur within three hours.

Nasal sprays are used to deliver medications locally in the nasal cavities or systemically. They are used locally for conditions such as nasal congestion and allergic rhinitis. In some situations, the nasal delivery route is preferred for systemic therapy because it provides an agreeable alternative to injection or pills. Substances can be assimilated extremely quickly and directly through the nose. Many pharmaceutical drugs exist as nasal sprays for systemic administration. Other applications include hormone replacement therapy, treatment of Alzheimer's disease and Parkinson's disease. Nasal sprays are seen as a more efficient way of transporting drugs with potential use in crossing the blood–brain barrier.

Calcitonin gene-related peptide (CGRP) is a member of the calcitonin family of peptides consisting of calcitonin, amylin, adrenomedullin, adrenomedullin 2 (intermedin) and calcitonin‑receptor‑stimulating peptide. Calcitonin is mainly produced by thyroid C cells whilst CGRP is secreted and stored in the nervous system. This peptide, in humans, exists in two forms: CGRP alpha, and CGRP beta. α-CGRP is a 37-amino acid neuropeptide and is formed by alternative splicing of the calcitonin/CGRP gene located on chromosome 11. β-CGRP is less studied. In humans, β-CGRP differs from α-CGRP by three amino acids and is encoded in a separate, nearby gene. The CGRP family includes calcitonin (CT), adrenomedullin (AM), and amylin (AMY).

Antimigraine drugs are medications intended to reduce the effects or intensity of migraine headache. They include drugs for the treatment of acute migraine symptoms as well as drugs for the prevention of migraine attacks.

Calcitonin receptor-like (CALCRL), also known as the calcitonin receptor-like receptor (CRLR), is a human protein; it is a receptor for calcitonin gene-related peptide.

DNA-directed RNA polymerase III subunit RPC9 is an enzyme that in humans is encoded by the CRCP gene.

Preprotachykinin-1,, is a precursor protein that in humans is encoded by the TAC1 gene.
Zucapsaicin (Civanex) is a medication used to treat osteoarthritis of the knee and other neuropathic pain. It is applied three times daily for a maximum of three months. Zucapsaicin is a member of phenols and a member of methoxybenzenes It is a modulator of transient receptor potential cation channel subfamily V member 1 (TRPV-1), also known as the vanilloid or capsaicin receptor 1 that reduces pain, and improves articular functions. It is the cis-isomer of capsaicin. Civamide, manufactured by Winston Pharmaceuticals, is produced in formulations for oral, nasal, and topical use.
Calcitonin gene-related peptide (CGRP) receptor antagonists are a class of drugs that act as antagonists of the calcitonin gene-related peptide receptor (CGRPR).

Olcegepant is a calcitonin gene-related peptide receptor antagonist being studied as a potential treatment for migraines.
Neuropeptide K, is a protein encoded by the TAC1 gene. It is an elongated derivative of the N-terminus of neurokinin A as the final post-translational processing product of beta-preprotachykinin.
Fremanezumab, sold under the brand name Ajovy, is a medication used to prevent migraines in adults. It is given by injection under the skin.
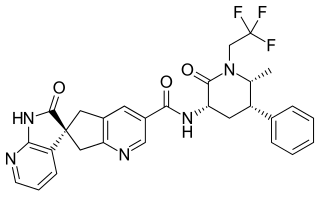
Ubrogepant, sold under the brand name Ubrelvy, is a medication used for the acute (immediate) treatment of migraine with or without aura in adults. It is not indicated for the preventive treatment of migraine. Ubrogepant is a small-molecule calcitonin gene-related peptide receptor antagonist. It is the first drug in this class approved for the acute treatment of migraine.

Wasabi receptor toxin (WaTx) is the active component of the venom of the Australian black rock scorpion Urodacus manicatus. WaTx targets TRPA1, also known as the wasabi receptor or irritant receptor. WaTx is a cell-penetrating toxin that stabilizes the TRPA1 channel open state while reducing its Ca2+-permeability, thereby eliciting pain and pain hypersensitivity without the neurogenic inflammation that typically occurs in other animal toxins.
Susan Diana Brain is a professor of pharmacology at the School of Cardiovascular Medicine and Sciences at King's College London where she has worked since 1989.

Iain Macintyre FRS was a British endocrinologist who made important contributions to the understanding of calcium regulation and bone metabolism. Shortly after the hormone calcitonin had been described by Harold Copp, Macintyre's team was the first to isolate and sequence the hormone and to demonstrate its origin in the parafollicular cells of the thyroid gland. He subsequently analysed its physiological actions. Along with H. R. Morris he isolated and sequenced calcitonin gene-related peptide. Later research centred on the role played by nitric oxide on bone metabolism.

A-967079 is a drug which acts as a potent and selective antagonist for the TRPA1 receptor. It has analgesic and antiinflammatory effects and is used in scientific research, but has not been developed for medical use.
References
- 1 2 Peroutka SJ (October 2005). "Neurogenic inflammation and migraine: implications for the therapeutics". Mol. Interv. 5 (5): 304–11. doi:10.1124/mi.5.5.10. PMID 16249526.
- 1 2 Chen Y, Lyga J (2014). "Brain-skin connection: stress, inflammation and skin aging". Inflamm Allergy Drug Targets. 13 (3): 177–90. doi:10.2174/1871528113666140522104422. PMC 4082169 . PMID 24853682.
- ↑ Geppetti P, Nassini R, Materazzi S, Benemei S (March 2008). "The concept of neurogenic inflammation". BJU Int. 101 (Suppl 3): 2–6. doi: 10.1111/j.1464-410X.2008.07493.x . PMID 18307678. S2CID 1096295.
- ↑ Caterina, M. J.; Leffler, A.; Malmberg, A. B.; Martin, W. J.; Trafton, J.; Petersen-Zeitz, K. R.; Koltzenburg, M.; Basbaum, A. I.; Julius, D. (2000-04-14). "Impaired nociception and pain sensation in mice lacking the capsaicin receptor". Science. 288 (5464): 306–313. Bibcode:2000Sci...288..306C. doi:10.1126/science.288.5464.306. ISSN 0036-8075. PMID 10764638.
- ↑ Lin King, John V.; Emrick, Joshua J.; Kelly, Mark J. S.; Herzig, Volker; King, Glenn F.; Medzihradszky, Katalin F.; Julius, David (2019-09-05). "A Cell-Penetrating Scorpion Toxin Enables Mode-Specific Modulation of TRPA1 and Pain". Cell. 178 (6): 1362–1374.e16. doi:10.1016/j.cell.2019.07.014. ISSN 1097-4172. PMC 6731142 . PMID 31447178.
- ↑ Zhao, Jianhua; King, John V. Lin; Cheng, Yifan; Julius, David (2019-12-27). "Mechanisms governing irritant-evoked activation and calcium modulation of TRPA1". bioRxiv: 2019.12.26.888982. doi: 10.1101/2019.12.26.888982 .
- ↑ Zhao, Jianhua; Lin King, John V.; Paulsen, Candice E.; Cheng, Yifan; Julius, David (2020-07-08). "Irritant-evoked activation and calcium modulation of the TRPA1 receptor". Nature. 585 (7823): 141–145. Bibcode:2020Natur.585..141Z. doi:10.1038/s41586-020-2480-9. ISSN 0028-0836. PMC 7483980 . PMID 32641835.
- ↑ Meseguer V, Alpizar YA, Luis E, Tajada S, Denlinger B, Fajardo O, et al. (2014). "TRPA1 channels mediate acute neurogenic inflammation and pain produced by bacterial endotoxins". Nat Commun. 5: 3125. Bibcode:2014NatCo...5.3125M. doi:10.1038/ncomms4125. PMC 3905718 . PMID 24445575.
- ↑ Rosa AC, Fantozzi R (September 2013). "The role of histamine in neurogenic inflammation". Br. J. Pharmacol. 170 (1): 38–45. doi:10.1111/bph.12266. PMC 3764847 . PMID 23734637.
- ↑ Malhotra R (2016). "Understanding migraine: Potential role of neurogenic inflammation". Ann Indian Acad Neurol. 19 (2): 175–82. doi: 10.4103/0972-2327.182302 . PMC 4888678 . PMID 27293326.
- ↑ Frediani F, Villani V, Casucci G (May 2008). "Peripheral mechanism of action of antimigraine prophylactic drugs". Neurol. Sci. 29 (Suppl 1): S127–30. doi:10.1007/s10072-008-0903-8. PMID 18545913. S2CID 24156261.
- ↑ Geppetti P, Capone JG, Trevisani M, Nicoletti P, Zagli G, Tola MR (April 2005). "CGRP and migraine: neurogenic inflammation revisited". J Headache Pain. 6 (2): 61–70. doi:10.1007/s10194-005-0153-6. PMC 3452316 . PMID 16362644.
- ↑ Schön and Boehncke, Psoriasis: Neurogenic inflammation and other mechanisms NEJM 352:1899-1912, Number 18, 2005
- 1 2 Saraceno R, Kleyn CE, Terenghi G, Griffiths CE (November 2006). "The role of neuropeptides in psoriasis". Br. J. Dermatol. 155 (5): 876–82. doi:10.1111/j.1365-2133.2006.07518.x. PMID 17034513. S2CID 9257957.
- ↑ Verones B, Oortgiesen M (December 2001). "Neurogenic inflammation and particulate matter (PM) air pollutants". Neurotoxicology. 22 (6): 795–810. doi:10.1016/S0161-813X(01)00062-6. PMID 11829413.
- ↑ Knipping S, Holzhausen HJ, Riederer A, Schrom T (August 2008). "[Ultrastructural changes in allergic rhinitis vs. idiopathic rhinitis]". HNO (in German). 56 (8): 799–807. doi:10.1007/s00106-008-1764-4. PMID 18651116. S2CID 24135943.
- ↑ Meggs, William J. The Role of Neurogenic Inflammation in Chemical Sensitivity (2017) EcopsychologyVol. 9, No. 2 Published Online:1 Jun 2017 https://doi.org/10.1089/eco.2016.0045
- ↑ Orriols R, Costa R, Cuberas G, Jacas C, Castell J, Sunyer J (December 2009). "Brain dysfunction in multiple chemical sensitivity". J. Neurol. Sci. 287 (1–2): 72–8. doi:10.1016/j.jns.2009.09.003. PMID 19801154. S2CID 28255407.
- ↑ Bascom R, Meggs WJ, Frampton M, Hudnell K, Killburn K, Kobal G, Medinsky M, Rea W (March 1997). "Neurogenic inflammation: with additional discussion of central and perceptual integration of nonneurogenic inflammation". Environ. Health Perspect. 105 (Suppl 2): 531–7. doi:10.1289/ehp.97105s2531. PMC 1469802 . PMID 9167992.
- ↑ Kalra AA, Elliott D (June 2007). "Acute migraine: Current treatment and emerging therapies". Ther Clin Risk Manag. 3 (3): 449–59. PMC 2386351 . PMID 18488069.
- ↑ Link AS, Kuris A, Edvinsson L (February 2008). "Treatment of migraine attacks based on the interaction with the trigemino-cerebrovascular system". J Headache Pain. 9 (1): 5–12. doi:10.1007/s10194-008-0011-4. PMC 2245994 . PMID 18217201.
- ↑ Grossmann, MD, Werner; Schmidramsl, MD, Hanns (2001). "An Extract of Petasites hybridus Is Effective in the Prophylaxis of Migraine" (PDF). Alternative Medicine Review. 6 (3): 303–10. PMID 11410074 . Retrieved 14 June 2015.
- ↑ Weglicki WB, Phillips TM (September 1992). "Pathobiology of magnesium deficiency: a cytokine/neurogenic inflammation hypothesis". Am. J. Physiol. 263 (3 Pt 2): R734–7. doi:10.1152/ajpregu.1992.263.3.R734. PMID 1384353.
- ↑ Rude RK, Singer FR, Gruber HE (April 2009). "Skeletal and hormonal effects of magnesium deficiency". J Am Coll Nutr. 28 (2): 131–41. doi:10.1080/07315724.2009.10719764. PMID 19828898. S2CID 43556609.
- ↑ "UpToDate".
- ↑ The Race to Offer CGRP for Migraine Migraine.com Editorial Team July 21, 2017
- ↑ Jancsó N, Jancsó-Gábor A, Szolcsányi J (September 1967). "Direct evidence for neurogenic inflammation and its prevention by denervation and by pretreatment with capsaicin". Br J Pharmacol Chemother. 31 (1): 138–51. doi:10.1111/j.1476-5381.1967.tb01984.x. PMC 1557289 . PMID 6055248.
- ↑ Durham PL, Vause CV (July 2010). "Calcitonin gene-related peptide (CGRP) receptor antagonists in the treatment of migraine". CNS Drugs. 24 (7): 539–48. doi:10.2165/11534920-000000000-00000. PMC 3138175 . PMID 20433208.
- ↑ Farinelli I, Missori S, Martelletti P (September 2008). "Proinflammatory mediators and migraine pathogenesis: moving towards CGRP as a target for a novel therapeutic class". Expert Rev Neurother. 8 (9): 1347–54. doi:10.1586/14737175.8.9.1347. PMID 18759547. S2CID 207195138.
- ↑ Farinelli I, De Filippis S, Coloprisco G, Missori S, Martelletti P (October 2009). "Future drugs for migraine". Intern Emerg Med. 4 (5): 367–73. doi:10.1007/s11739-009-0273-0. PMID 19551474. S2CID 26070466.
- ↑ Clinical trial number NCT00816517 for "Use of Botulinum Toxin to Treat Psoriasis" at ClinicalTrials.gov
- ↑ Product Information: Astelin, azelastine. Wallace Laboratories, Cranbury, NJ. (PI Revised 08/2000) PI Reviewed 01/2001
- ↑ Gehanno P, Deschamps E, Garay E, Baehre M, Garay RP (2001). "Vasomotor rhinitis: clinical efficacy of azelastine nasal spray in comparison with placebo". ORL J. Otorhinolaryngol. Relat. Spec. 63 (2): 76–81. doi:10.1159/000055714. PMID 11244365. S2CID 23292869.
- ↑ Bucelli RC, Gonsiorek EA, Kim WY, Bruun D, Rabin RA, Higgins D, Lein PJ (March 2008). "Statins decrease expression of the proinflammatory neuropeptides calcitonin gene-related peptide and substance P in sensory neurons". J. Pharmacol. Exp. Ther. 324 (3): 1172–80. doi:10.1124/jpet.107.132795. PMID 18079356. S2CID 1001915.
- ↑ Chiu IM, von Hehn CA, Woolf CJ (July 2012). "Neurogenic inflammation and the peripheral nervous system in host defense and immunopathology". Nat. Neurosci. 15 (8): 1063–7. doi:10.1038/nn.3144. PMC 3520068 . PMID 22837035.
- ↑ Chiu IM, von Hehn CA, Woolf CJ (2012). "Neurogenic inflammation and the peripheral nervous system in host defense and immunopathology". Nat Neurosci. 15 (8). Figure 3. doi:10.1038/nn.3144. PMC 3520068 . PMID 22837035.