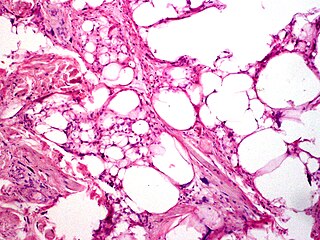
Liposarcomas are the most common subtype of soft tissue sarcomas, accounting for at least 20% of all sarcomas in adults. Soft tissue sarcomas are rare neoplasms with over 150 different histological subtypes or forms. Liposarcomas arise from the precursor lipoblasts of the adipocytes in adipose tissues. Adipose tissues are distributed throughout the body, including such sites as the deep and more superficial layers of subcutaneous tissues as well as in less surgically accessible sites like the retroperitoneum and visceral fat inside the abdominal cavity.

Hemangioendotheliomas are a family of vascular neoplasms of intermediate malignancy.

A schwannoma is a usually benign nerve sheath tumor composed of Schwann cells, which normally produce the insulating myelin sheath covering peripheral nerves.

Granular cell tumor is a tumor that can develop on any skin or mucosal surface, but occurs on the tongue 40% of the time.

Angiomyxoma is a myxoid tumor involving the blood vessels.
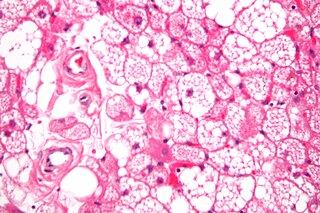
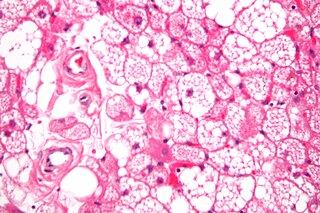
A hibernoma is a benign neoplasm of vestigial brown fat. They were first described under the name ‘pseudolipoma’ by the German physician H. Merkel in 1906 and the term hibernoma was proposed by the French anatomist Louis Gery in 1914 because of its resemblance to brown fat in hibernating animals.
Plexiform fibrohistiocytic tumor is a rare tumor that arises primarily on the upper extremities of children and young adults.

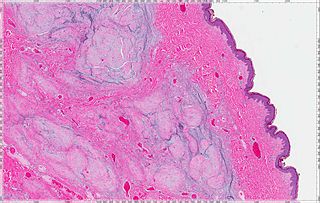
Atypical fibroxanthoma (AFX) of the skin is a low-grade malignancy related to malignant fibrous histiocytoma, which it resembles histologically. Atypical fibroxanthoma manifests as a hard, pink or red papule or nodule that grows over the course of several months and may bleed or ulcerate. They typically occur on the head and neck. Atypical fibroxanthoma is usually asymptomatic.

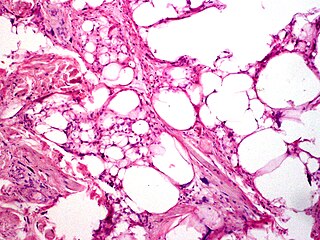
Spindle cell lipoma is an asymptomatic, slow-growing subcutaneous tumor that has a predilection for the posterior back, neck, and shoulders of older men.
Pleomorphic lipomas, like spindle-cell lipomas, occur for the most part on the backs and necks of elderly men, and are characterized by floret giant cells with overlapping nuclei.
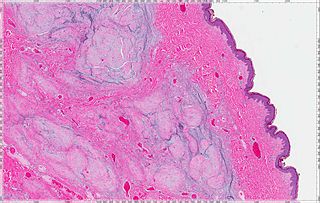
A cutaneous myxoma, or superficial angiomyxoma, consists of a multilobulated myxoid mass containing stellate or spindled fibroblasts with pools of mucin forming cleft-like spaces. There is often a proliferation of blood vessels and an inflammatory infiltrate. Staining is positive for vimentin, negative for cytokeratin and desmin, and variable for CD34, Factor VIIIa, SMA, MSA and S-100.
A superficial acral fibromyxoma is a type of myxoma and is a rare cutaneous condition characterized by a mesenchymal neoplasm that typically occurs on the digits of middle-aged adults.

Low-grade fibromyxoid sarcoma (LGFMS) is a rare type of low-grade sarcoma first described by H. L. Evans in 1987. LGFMS are soft tissue tumors of the mesenchyme-derived connective tissues; on microscopic examination, they are found to be composed of spindle-shaped cells that resemble fibroblasts. These fibroblastic, spindle-shaped cells are neoplastic cells that in most cases of LGFMS express fusion genes, i.e. genes composed of parts of two different genes that form as a result of mutations. The World Health Organization (2020) classified LGFMS as a specific type of tumor in the category of malignant fibroblastic and myofibroblastic tumors.
Rhabdomyoma is a benign mesenchymal tumor of skeletal muscle, separated into two major categories based on site: Cardiac and extracardiac. They are further separated by histology: fetal, juvenile (intermediate), and adult types. Genital types are recognized, but are often part of either the fetal or juvenile types. The fetal type is thought to recapitulate immature skeletal muscle at about week six to ten of gestational development.
An intraneural perineurioma is a rare benign tumor within the sheath of a single nerve that grows but typically does not recur or metastasize. These lesions are only composed of perineurial cells, cloned from a single cell. They are distinct from schwannoma and neurofibroma.

A myxoid tumor is a connective tissue tumor with a "myxoid" background, composed of clear, mucoid substance.
Ectomesenchymal chondromyxoid tumor (ECT) is a benign intraoral tumor with presumed origin from undifferentiated (ecto)mesenchymal cells. There are some who think it is a myoepithelial tumor type.
Acral myxoinflammatory fibroblastic sarcoma (AMSF), also termed myxoinflammatory fibroblastic sarcoma (MSF), is a rare, low-grade, soft tissue tumor that the World Health Organization (2020) classified as in the category of rarely metastasizing fibroblastic and myofibroblastic tumors. It is a locally aggressive neoplasm that often recurs at the site of its surgical removal. However, it usually grows slowly and in only 1–2% of cases spreads to distant tissues.
Lipofibromatosis-like neural tumor (LPF-NT) is an extremely rare soft tissue tumor first described by Agaram et al in 2016. As of mid-2021, at least 39 cases of LPF-NT have been reported in the literature. LPF-NT tumors have several features that resemble lipofibromatosis (LPF) tumors, malignant peripheral nerve sheath tumors, spindle cell sarcomas, low-grade neural tumors, peripheral nerve sheath tumors, and other less clearly defined tumors; Prior to the Agaram at al report, LPF-NTs were likely diagnosed as variants or atypical forms of these tumors. The analyses of Agaram at al and subsequent studies uncovered critical differences between LPF-NT and the other tumor forms which suggest that it is a distinct tumor entity differing not only from lipofibromatosis but also the other tumor forms.
Angiofibroma of soft tissue (AFST), also termed angiofibroma, not otherwise specified, is a recently recognized and rare disorder that was classified in the category of benign fibroblastic and myofibroblastic tumors by the World Health Organization in 2020. An AFST tumor is a neoplasm that was first described by A. Mariño-Enríquez and C.D. Fletcher in 2012.