Related Research Articles

Mold health issues refer to the harmful health effects of molds and their mycotoxins. However, recent research has shown these adverse health effects are caused not exclusively by molds, but also other microbial agents and biotoxins associated with dampness, mold, and water-damaged buildings, such as gram-negative bacteria that produce endotoxins, as well as actinomycetes and their associated exotoxins. Approximately 47% of houses in the United States have substantial levels of mold, with over 85% of commercial and office buildings found to have water damage predictive of mold. As many as 21% of asthma cases may result from exposure to mold. Substantial and statistically significant increases in the risks of both respiratory infections and bronchitis have been associated with dampness in homes and the resulting mold.

Berylliosis, or chronic beryllium disease (CBD), is a chronic allergic-type lung response and chronic lung disease caused by exposure to beryllium and its compounds, a form of beryllium poisoning. It is distinct from acute beryllium poisoning, which became rare following occupational exposure limits established around 1950. Berylliosis is an occupational lung disease.

A pesticide poisoning occurs when pesticides, chemicals intended to control a pest, affect non-target organisms such as humans, wildlife, plants, or bees. There are three types of pesticide poisoning. The first of the three is a single and short-term very high level of exposure which can be experienced by individuals who die by suicide, as well as pesticide formulators. The second type of poisoning is long-term high-level exposure, which can occur in pesticide formulators and manufacturers. The third type of poisoning is a long-term low-level exposure, which individuals are exposed to from sources such as pesticide residues in food as well as contact with pesticide residues in the air, water, soil, sediment, food materials, plants and animals.

Silicosis is a form of occupational lung disease caused by inhalation of crystalline silica dust. It is marked by inflammation and scarring in the form of nodular lesions in the upper lobes of the lungs. It is a type of pneumoconiosis. Silicosis, particularly the acute form, is characterized by shortness of breath, cough, fever, and cyanosis. It may often be misdiagnosed as pulmonary edema, pneumonia, or tuberculosis. Using workplace controls, silicosis is almost always a preventable disease.
Metal fume fever, also known as brass founders' ague, brass shakes, zinc shakes, galvie flu, galvo poisoning, metal dust fever, welding shivers, or Monday morning fever, is an illness primarily caused by exposure to chemicals such as zinc oxide (ZnO), aluminium oxide (Al2O3), or magnesium oxide (MgO) which are produced as byproducts in the fumes that result when certain metals are heated. Other common sources are fuming silver, gold, platinum, and chromium.

Hypersensitivity pneumonitis (HP) or extrinsic allergic alveolitis (EAA) is a syndrome caused by the repetitive inhalation of antigens from the environment in susceptible or sensitized people. Common antigens include molds, bacteria, bird droppings, bird feathers, agricultural dusts, bioaerosols and chemicals from paints or plastics. People affected by this type of lung inflammation (pneumonitis) are commonly exposed to the antigens by their occupations, hobbies, the environment and animals. The inhaled antigens produce a hypersensitivity immune reaction causing inflammation of the airspaces (alveoli) and small airways (bronchioles) within the lung. Hypersensitivity pneumonitis may eventually lead to interstitial lung disease.

Byssinosis is an occupational lung disease caused by inhalation of cotton or jute dust in inadequately ventilated working environments and can develop over time with repeated exposure. Byssinosis commonly occurs in textile workers who are employed in yarn and fabric manufacture industries. It is now thought that the cotton dust directly causes the disease and some believe that the causative agents are endotoxins that come from the cell walls of gram-negative bacteria that grow on the cotton. Although bacterial endotoxin is a likely cause, the absence of similar symptoms in workers in other industries exposed to endotoxins makes this uncertain. Current smokers are also at risk for developing byssinosis or having complications relating to byssinosis.

Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris, aspiration, herbicides or fluorocarbons and some systemic diseases. If unresolved, continued inflammation can result in irreparable damage such as pulmonary fibrosis.

Farmer's lung is a hypersensitivity pneumonitis induced by the inhalation of biologic dusts coming from hay dust or mold spores or any other agricultural products. It results in a type III hypersensitivity inflammatory response and can progress to become a chronic condition which is considered potentially dangerous.
Occupational lung diseases comprise a broad group of diseases, including occupational asthma, industrial bronchitis, chronic obstructive pulmonary disease (COPD), bronchiolitis obliterans, inhalation injury, interstitial lung diseases, infections, lung cancer and mesothelioma. These can be caused directly or due to immunological response to an exposure to a variety of dusts, chemicals, proteins or organisms. Occupational cases of interstitial lung disease may be misdiagnosed as COPD, idiopathic pulmonary fibrosis, or a myriad of other diseases; leading to a delay in identification of the causative agent.
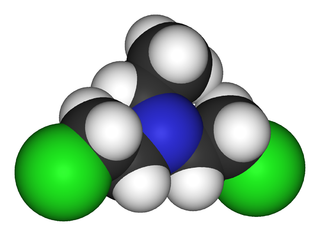
Bis(2-chloroethyl)ethylamine is the organic compound with the formula C2H5N(CH2CH2Cl)2. Often abbreviated HN1, it is a powerful vesicant and a nitrogen mustard gas used for chemical warfare. HN1 was developed in the 1920s and 1930s to remove warts and later as a military agent. Because of the latter use, it is a Schedule 1 chemical within the Chemical Weapons Convention and therefore use and production is strongly restricted. It has never been used in warfare.
The use of podiatry drills, in the absence of engineering controls and personal protective equipment, is an occupational hazard to the healthcare provider. Nail dust collected during foot care procedures performed in office settings has been found to contain keratin, keratin hydrolysates, microbial debris, and viable fungal elements, including dermatophytes and saprotrophs. Exposure to nail dust and the associated risk will vary with the policies and practices in place, the type of podiatry drill used, therapy technique, frequency of procedures, personal protective equipment utilized and the use of ventilation systems.
Occupational asthma is new onset asthma or the recurrence of previously quiescent asthma directly caused by exposure to an agent at workplace. It is an occupational lung disease and a type of work-related asthma. Agents that can induce occupational asthma can be grouped into sensitizers and irritants.
Aerotoxic syndrome relates to ill-health effects associated with breathing contaminated air in an airliner cabin. Researchers have associated aerotoxic syndrome with exposure to substances such as engine oil and hydraulic fluid. Although researchers have identified correlations between the aircraft occupational environment and symptoms of aerotoxic syndrome, this condition is not an established medical diagnosis because the incidence and aetiology of the condition are still under debate.
Chronic solvent-induced encephalopathy (CSE) is a condition induced by long-term exposure to organic solvents, often—but not always—in the workplace, that lead to a wide variety of persisting sensorimotor polyneuropathies and neurobehavioral deficits even after solvent exposure has been removed. This syndrome can also be referred to as psycho-organic syndrome, organic solvent syndrome, chronic painter's syndrome, occupational solvent encephalopathy, solvent intoxication, toxic solvent syndrome, painters disease, chronic toxic encephalopathy, or neurasthenic syndrome. The multiple names of solvent-induced syndromes combined with inconsistency in research methods makes referencing this disease difficult and its catalog of symptoms vague.
Acute inhalation injury may result from frequent and widespread use of household cleaning agents and industrial gases. The airways and lungs receive continuous first-pass exposure to non-toxic and irritant or toxic gases via inhalation. Irritant gases are those that, on inhalation, dissolve in the water of the respiratory tract mucosa and provoke an inflammatory response, usually from the release of acidic or alkaline radicals. Smoke, chlorine, phosgene, sulfur dioxide, hydrogen chloride, hydrogen sulfide, nitrogen dioxide, ozone, and ammonia are common irritants.
Chlorine gas poisoning is an illness resulting from the effects of exposure to chlorine beyond the threshold limit value.

Agricultural safety and health is an aspect of occupational safety and health in the agricultural workplace. It specifically addresses the health and safety of farmers, farm workers, and their families.
Occupational toxicology is the application of toxicology to chemical hazards in the workplace. It focuses on substances and conditions that people may be exposed to in workplaces, including inhalation and dermal exposures, which are most prevalent when discussing occupational toxicology. These environmental and individual exposures can impact health, and there is a focus on identifying early adverse affects that are more subtle than those presented in clinical medicine.

Occupational dust exposure occurs when small particles are generated at the workplace through the disturbance/agitation of rock/mineral, dry grain, timber, fiber, or other material. When these small particles become suspended in the air, they can pose a risk to the health of those who breath in the contaminated air.
References
- 1 2 3 4 5 6 7 Seifert SA, Von Essen S, Jacobitz K, Crouch R, Lintner CP (2003). "Organic dust toxic syndrome: a review". Journal of Toxicology: Clinical Toxicology. 41 (2): 185–93. doi:10.1081/clt-120019136. PMID 12733858. S2CID 35345201.
- 1 2 Linaker C, Smedley J (December 2002). "Respiratory illness in agricultural workers". Occupational Medicine. 52 (8): 451–59. doi: 10.1093/occmed/52.8.451 . PMID 12488515.
- ↑ National Institute for Occupational Safety and Health (April 1994). "Request for Assistance in Preventing Organic Dust Toxic Syndrome". DHHS (NIOSH) Publication Number (94–102).