Related Research Articles

Parathyroid glands are small endocrine glands in the neck of humans and other tetrapods. Humans usually have four parathyroid glands, located on the back of the thyroid gland in variable locations. The parathyroid gland produces and secretes parathyroid hormone in response to a low blood calcium, which plays a key role in regulating the amount of calcium in the blood and within the bones.

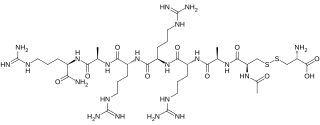
Parathyroid hormone (PTH), also called parathormone or parathyrin, is a peptide hormone secreted by the parathyroid glands that regulates the serum calcium concentration through its effects on bone, kidney, and intestine.

Calcium metabolism is the movement and regulation of calcium ions (Ca2+) in (via the gut) and out (via the gut and kidneys) of the body, and between body compartments: the blood plasma, the extracellular and intracellular fluids, and bone. Bone acts as a calcium storage center for deposits and withdrawals as needed by the blood via continual bone remodeling.

Calcitonin is a 32 amino acid peptide hormone secreted by parafollicular cells (also known as C cells) of the thyroid (or endostyle) in humans and other chordates in the ultimopharyngeal body. It acts to reduce blood calcium (Ca2+), opposing the effects of parathyroid hormone (PTH).
Hypercalcemia, also spelled hypercalcaemia, is a high calcium (Ca2+) level in the blood serum. The normal range is 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), with levels greater than 2.6 mmol/L defined as hypercalcemia. Those with a mild increase that has developed slowly typically have no symptoms. In those with greater levels or rapid onset, symptoms may include abdominal pain, bone pain, confusion, depression, weakness, kidney stones or an abnormal heart rhythm including cardiac arrest.
Disorders of calcium metabolism occur when the body has too little or too much calcium. The serum level of calcium is closely regulated within a fairly limited range in the human body. In a healthy physiology, extracellular calcium levels are maintained within a tight range through the actions of parathyroid hormone, vitamin D and the calcium sensing receptor. Disorders in calcium metabolism can lead to hypocalcemia, decreased plasma levels of calcium or hypercalcemia, elevated plasma calcium levels.

Parathyroid hormone-related protein (PTHrP) is a proteinaceous hormone and a member of the parathyroid hormone family secreted by mesenchymal stem cells. It is occasionally secreted by cancer cells. However, it also has normal functions in bone, teeth, vascular tissues and other tissues.

Parathyroid chief cells are one of the two cell types of the parathyroid glands, along with oxyphil cells. The chief cells are much more prevalent in the parathyroid gland than the oxyphil cells. It is perceived that oxyphil cells may be derived from chief cells at puberty, as they are not present at birth like chief cells.
Hypoparathyroidism is decreased function of the parathyroid glands with underproduction of parathyroid hormone (PTH). This can lead to low levels of calcium in the blood, often causing cramping and twitching of muscles or tetany, and several other symptoms. It is a very rare disease. The condition can be inherited, but it is also encountered after thyroid or parathyroid gland surgery, and it can be caused by immune system-related damage as well as a number of rarer causes. The diagnosis is made with blood tests, and other investigations such as genetic testing depending on the results. The primary treatment of hypoparathyroidism is calcium and vitamin D supplementation. Calcium replacement or vitamin D can ameliorate the symptoms but can increase the risk of kidney stones and chronic kidney disease. Additionally, medications such as recombinant human parathyroid hormone or teriparatide may be given by injection to replace the missing hormone.

Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands or as response to external stimuli. Symptoms of hyperparathyroidism are caused by inappropriately normal or elevated blood calcium excreted from the bones and flowing into the blood stream in response to increased production of parathyroid hormone. In healthy people, when blood calcium levels are high, parathyroid hormone levels should be low. With long-standing hyperparathyroidism, the most common symptom is kidney stones. Other symptoms may include bone pain, weakness, depression, confusion, and increased urination. Both primary and secondary may result in osteoporosis.
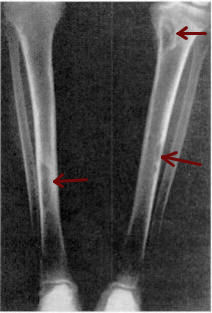
Osteitis fibrosa cystica is a skeletal disorder resulting in a loss of bone mass, a weakening of the bones as their calcified supporting structures are replaced with fibrous tissue, and the formation of cyst-like brown tumors in and around the bone. Osteitis fibrosis cystica (OFC), also known as osteitis fibrosa, osteodystrophia fibrosa, and von Recklinghausen's disease of bone, is caused by hyperparathyroidism, which is a surplus of parathyroid hormone from over-active parathyroid glands. This surplus stimulates the activity of osteoclasts, cells that break down bone, in a process known as osteoclastic bone resorption. The hyperparathyroidism can be triggered by a parathyroid adenoma, hereditary factors, parathyroid carcinoma, or renal osteodystrophy. Osteoclastic bone resorption releases minerals, including calcium, from the bone into the bloodstream, causing both elevated blood calcium levels, and the structural changes which weaken the bone. The symptoms of the disease are the consequences of both the general softening of the bones and the excess calcium in the blood, and include bone fractures, kidney stones, nausea, moth-eaten appearance in the bones, appetite loss, and weight loss.
There are two known parathyroid hormone receptors in mammals termed PTH1R and PTH2R. These receptors bind parathyroid hormone and are members of the GPCR family of transmembrane proteins.

The calcium-sensing receptor (CaSR) is a Class C G-protein coupled receptor which senses extracellular levels of calcium ions. It is primarily expressed in the parathyroid gland, the renal tubules of the kidney and the brain. In the parathyroid gland, it controls calcium homeostasis by regulating the release of parathyroid hormone (PTH). In the kidney it has an inhibitory effect on the reabsorption of calcium, potassium, sodium, and water depending on which segment of the tubule is being activated.

Parathyroid hormone/parathyroid hormone-related peptide receptor, also known as parathyroid hormone 1 receptor (PTH1R), is a protein that in humans is encoded by the PTH1R gene. PTH1R functions as a receptor for parathyroid hormone (PTH) and for parathyroid hormone-related protein (PTHrP), also called parathyroid hormone-like hormone (PTHLH).

Parathyroid hormone 2 receptor is a protein that in humans is encoded by the PTH2R gene.

Indian hedgehog homolog (Drosophila), also known as IHH, is a protein which in humans is encoded by the IHH gene. This cell signaling protein is in the hedgehog signaling pathway. The several mammalian variants of the Drosophila hedgehog gene (which was the first named) have been named after the various species of hedgehog; the Indian hedgehog is honored by this one. The gene is not specific to Indian hedgehogs.

Tuberoinfundibular peptide of 39 residues is a protein that in humans is encoded by the PTH2 gene.
Abaloparatide, sold under the brand name Tymlos among others, is a parathyroid hormone-related protein (PTHrP) analog medication used to treat osteoporosis. It is an anabolic agent.
A bone growth factor is a growth factor that stimulates the growth of bone tissue.
Etelcalcetide is a calcimimetic drug for the treatment of secondary hyperparathyroidism in patients undergoing hemodialysis. It is administered intravenously at the end of each dialysis session. Etelcalcetide functions by binding to and activating the calcium-sensing receptor in the parathyroid gland. Parsabiv is currently owned by Amgen and Ono Pharmaceuticals in Japan.
References
- ↑ VanHouten JN, Dann P, Stewart AF, Watson CJ, Pollak M, Karaplis AC, Wysolmerski JJ (November 2003). "Mammary-specific deletion of parathyroid hormone-related protein preserves bone mass during lactation". J. Clin. Invest. 112 (9): 1429–36. doi:10.1172/JCI19504. PMC 228471 . PMID 14597768.
- ↑ McCauley LK, Martin TJ (June 2012). "Twenty-five years of PTHrP progress: from cancer hormone to multifunctional cytokine". J. Bone Miner. Res. 27 (6): 1231–9. doi:10.1002/jbmr.1617. PMC 4871126 . PMID 22549910.
- ↑ Martin TJ, Allan EH, Caple IW, Care AD, Danks JA, Diefenbach-Jagger H, Ebeling PR, Gillespie MT, Hammonds G, Heath JA (1989). "Parathyroid hormone-related protein: isolation, molecular cloning, and mechanism of action". Recent Prog. Horm. Res. 45: 467–502, discussion 502–6. doi:10.1016/b978-0-12-571145-6.50014-5. ISBN 9780125711456. PMID 2682846.
- ↑ Pinheiro PL, Cardoso JC, Gomes AS, Fuentes J, Power DM, Canário AV (2010). "Gene structure, transcripts and calciotropic effects of the PTH family of peptides in Xenopus and chicken". BMC Evol. Biol. 10: 373. doi: 10.1186/1471-2148-10-373 . PMC 3009671 . PMID 21122104.
- ↑ Guerreiro PM, Renfro JL, Power DM, Canario AV (February 2007). "The parathyroid hormone family of peptides: structure, tissue distribution, regulation, and potential functional roles in calcium and phosphate balance in fish". Am. J. Physiol. Regul. Integr. Comp. Physiol. 292 (2): R679–96. CiteSeerX 10.1.1.319.8873 . doi:10.1152/ajpregu.00480.2006. PMID 17023665.