Parathyroid glands are small endocrine glands in the neck of humans and other tetrapods. Humans usually have four parathyroid glands, located on the back of the thyroid gland in variable locations. The parathyroid gland produces and secretes parathyroid hormone in response to a low blood calcium, which plays a key role in regulating the amount of calcium in the blood and within the bones.

Parathyroid hormone (PTH), also called parathormone or parathyrin, is a peptide hormone secreted by the parathyroid glands that regulates the serum calcium concentration through its effects on bone, kidney, and intestine.

Calcium metabolism is the movement and regulation of calcium ions (Ca2+) in (via the gut) and out (via the gut and kidneys) of the body, and between body compartments: the blood plasma, the extracellular and intracellular fluids, and bone. Bone acts as a calcium storage center for deposits and withdrawals as needed by the blood via continual bone remodeling.
Osteoblasts are cells with a single nucleus that synthesize bone. However, in the process of bone formation, osteoblasts function in groups of connected cells. Individual cells cannot make bone. A group of organized osteoblasts together with the bone made by a unit of cells is usually called the osteon.

Calcitonin is a 32 amino acid peptide hormone secreted by parafollicular cells (also known as C cells) of the thyroid (or endostyle) in humans and other chordates in the ultimopharyngeal body. It acts to reduce blood calcium (Ca2+), opposing the effects of parathyroid hormone (PTH).
Hypercalcemia, also spelled hypercalcaemia, is a high calcium (Ca2+) level in the blood serum. The normal range is 2.1–2.6 mmol/L (8.8–10.7 mg/dL, 4.3–5.2 mEq/L), with levels greater than 2.6 mmol/L defined as hypercalcemia. Those with a mild increase that has developed slowly typically have no symptoms. In those with greater levels or rapid onset, symptoms may include abdominal pain, bone pain, confusion, depression, weakness, kidney stones or an abnormal heart rhythm including cardiac arrest.

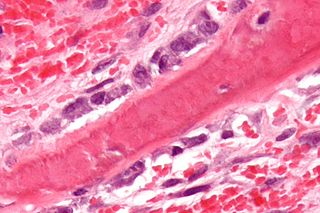
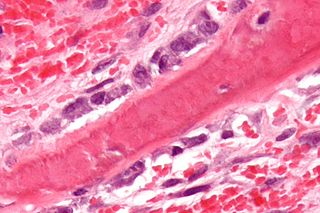
Parathyroid chief cells are one of the two cell types of the parathyroid glands, along with oxyphil cells. The chief cells are much more prevalent in the parathyroid gland than the oxyphil cells. It is perceived that oxyphil cells may be derived from chief cells at puberty, as they are not present at birth like chief cells.

Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands or as response to external stimuli. Symptoms of hyperparathyroidism are caused by inappropriately normal or elevated blood calcium leaving the bones and flowing into the blood stream in response to increased production of parathyroid hormone. In healthy people, when blood calcium levels are high, parathyroid hormone levels should be low. With long-standing hyperparathyroidism, the most common symptom is kidney stones. Other symptoms may include bone pain, weakness, depression, confusion, and increased urination. Both primary and secondary may result in osteoporosis.
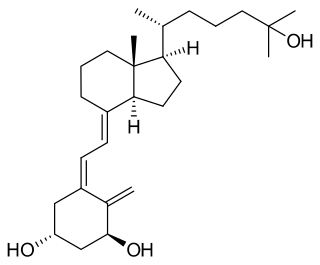
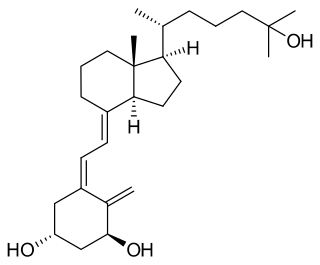
Calcitriol is the active form of vitamin D, normally made in the kidney. It is also known as 1,25-dihydroxycholecalciferol. It is a hormone which binds to and activates the vitamin D receptor in the nucleus of the cell, which then increases the expression of many genes. Calcitriol increases blood calcium (Ca2+) mainly by increasing the uptake of calcium from the intestines.

Primary hyperparathyroidism is a medical condition where the parathyroid gland produce excess amounts of parathyroid hormone (PTH). The symptoms of the condition relate to the resulting elevated serum calcium (hypercalcemia), which can cause digestive symptoms, kidney stones, psychiatric abnormalities, and bone disease.

Bone resorption is resorption of bone tissue, that is, the process by which osteoclasts break down the tissue in bones and release the minerals, resulting in a transfer of calcium from bone tissue to the blood.
There are two known parathyroid hormone receptors in mammals termed PTH1R and PTH2R. These receptors bind parathyroid hormone and are members of the GPCR family of transmembrane proteins.

Jansen's metaphyseal chondrodysplasia (JMC) is a disease that results from ligand-independent activation of the type 1 (PTH1R) of the parathyroid hormone receptor, due to one of three reported mutations.

The calcium-sensing receptor (CaSR) is a Class C G-protein coupled receptor which senses extracellular levels of calcium ions. It is primarily expressed in the parathyroid gland, the renal tubules of the kidney and the brain. In the parathyroid gland, it controls calcium homeostasis by regulating the release of parathyroid hormone (PTH). In the kidney it has an inhibitory effect on the reabsorption of calcium, potassium, sodium, and water depending on which segment of the tubule is being activated.

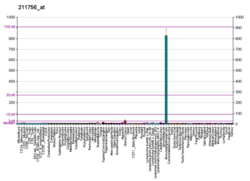
Parathyroid hormone/parathyroid hormone-related peptide receptor, also known as parathyroid hormone 1 receptor (PTH1R), is a protein that in humans is encoded by the PTH1R gene. PTH1R functions as a receptor for parathyroid hormone (PTH) and for parathyroid hormone-related protein (PTHrP), also called parathyroid hormone-like hormone (PTHLH).

Parathyroid hormone 2 receptor is a protein that in humans is encoded by the PTH2R gene.

Tuberoinfundibular peptide of 39 residues is a protein that in humans is encoded by the PTH2 gene.
The parathyroid hormone family is a family of structurally and functionally related proteins. Parathyroid hormone (PTH) is a polypeptidic hormone primarily involved in calcium metabolism. The parathyroid hormone-related protein (PTH-rP) is a related protein with predominantly paracrine function and possibly an endocrine role in lactation, as PTHrP has been found to be secreted by mammary glands into the circulation and increase bone turnover. PTH and PTH-rP bind to the same G-protein coupled receptor. The related protein PTH-L has been found in teleost fish, which also have two forms of PTH and PTHrP. Three subfamilies can be identified: PTH, PTHrP and PTH-L.
Abaloparatide, sold under the brand name Tymlos among others, is a parathyroid hormone-related protein (PTHrP) analog medication used to treat osteoporosis. It is an anabolic agent.
A bone growth factor is a growth factor that stimulates the growth of bone tissue.