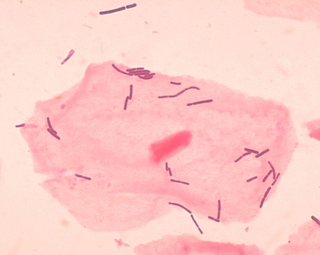
Bacterial vaginosis (BV) is an infection of the vagina caused by excessive growth of bacteria. Common symptoms include increased vaginal discharge that often smells like fish. The discharge is usually white or gray in color. Burning with urination may occur. Itching is uncommon. Occasionally, there may be no symptoms. Having BV approximately doubles the risk of infection by a number of sexually transmitted infections, including HIV/AIDS. It also increases the risk of early delivery among pregnant women.

Meconium is the earliest stool of a mammalian infant resulting from defecation. Unlike later feces, meconium is composed of materials ingested during the time the infant spends in the uterus: intestinal epithelial cells, lanugo, mucus, amniotic fluid, bile, and water. Meconium, unlike later feces, is viscous and sticky like tar – its color usually being a very dark olive green and it is almost odorless. When diluted in amniotic fluid, it may appear in various shades of green, brown, or yellow. It should be completely passed by the end of the first few days after birth, with the stools progressing toward yellow.
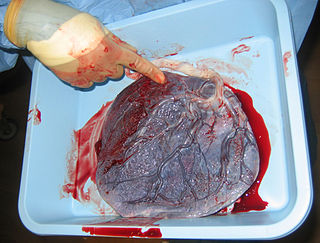
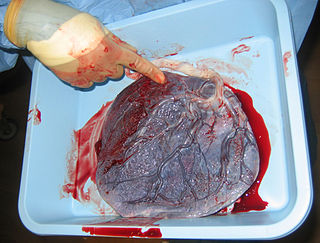
The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth. Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.
Fetal distress, also known as non-reassuring fetal status, is a condition during pregnancy or labor in which the fetus shows signs of inadequate oxygenation. Due to its imprecision, the term "fetal distress" has fallen out of use in American obstetrics. The term "non-reassuring fetal status" has largely replaced it. It is characterized by changes in fetal movement, growth, heart rate, and presence of meconium stained fluid.

Prelabor rupture of membranes (PROM), previously known as premature rupture of membranes, is breakage of the amniotic sac before the onset of labor. Women usually experience a painless gush or a steady leakage of fluid from the vagina. Complications in the baby may include premature birth, cord compression, and infection. Complications in the mother may include placental abruption and postpartum endometritis.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.
Postterm pregnancy is when a woman has not yet delivered her baby after 42 weeks of gestation, two weeks beyond the typical 40-week duration of pregnancy. Postmature births carry risks for both the mother and the baby, including fetal malnutrition, meconium aspiration syndrome, and stillbirths. After the 42nd week of gestation, the placenta, which supplies the baby with nutrients and oxygen from the mother, starts aging and will eventually fail. Postterm pregnancy is a reason to induce labor.
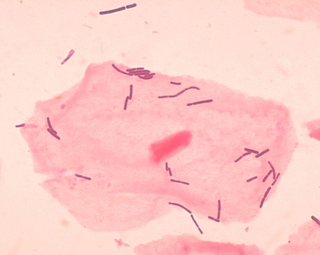
Vaginal flora, vaginal microbiota or vaginal microbiome are the microorganisms that colonize the vagina. They were discovered by the German gynecologist Albert Döderlein in 1892 and are part of the overall human flora. The amount and type of bacteria present have significant implications for an individual's overall health. The primary colonizing bacteria of a healthy individual are of the genus Lactobacillus, such as L. crispatus, and the lactic acid they produce is thought to protect against infection by pathogenic species.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.
A cervical mucus plug (operculum) is a plug that fills and seals the cervical canal during pregnancy. It is formed by a small amount of cervical mucus that condenses to form a cervical mucus plug during pregnancy.
Placental alpha microglobulin-1 (PAMG-1) is a human protein that was first isolated in 1975 from amniotic fluid. PAMG-1 is an important biomarker for the detection of premature rupture of fetal membrane (PROM) The high concentration of PAMG-1 in amniotic fluid means it can be used to detect if this fluid is present in the cervico-vaginal discharge of pregnant women; the presence of PAMG-1 in the discharge suggests that amniotic fluid is present, and therefore suggests that PROM has occurred. PAMG-1 was originally referred to as specific alpha-1 globulin of placenta.

The fetal membranes are the four extraembryonic membranes, associated with the developing embryo, and fetus in humans and other mammals. They are the amnion, chorion, allantois, and yolk sac. The amnion and the chorion are the chorioamniotic membranes that make up the amniotic sac which surrounds and protects the embryo. The fetal membranes are four of six accessory organs developed by the conceptus that are not part of the embryo itself, the other two are the placenta, and the umbilical cord.
Amnioinfusion is a method in which isotonic fluid is instilled into the uterine cavity.
The initial acquisition of microbiota is the formation of an organism's microbiota immediately before and after birth. The microbiota are all the microorganisms including bacteria, archaea and fungi that colonize the organism. The microbiome is another term for microbiota or can refer to the collected genomes.
The vaginal flora in pregnancy, or vaginal microbiota in pregnancy, is different from the vaginal flora before sexual maturity, during reproductive years, and after menopause. A description of the vaginal flora of pregnant women who are immunocompromised is not covered in this article. The composition of the vaginal flora significantly differs in pregnancy. Bacteria or viruses that are infectious most often have no symptoms.

Neonatal infections are infections of the neonate (newborn) acquired during prenatal development or within the first four weeks of life. Neonatal infections may be contracted by mother to child transmission, in the birth canal during childbirth, or after birth. Neonatal infections may present soon after delivery, or take several weeks to show symptoms. Some neonatal infections such as HIV, hepatitis B, and malaria do not become apparent until much later. Signs and symptoms of infection may include respiratory distress, temperature instability, irritability, poor feeding, failure to thrive, persistent crying and skin rashes.
The Human Microbiome Project (HMP), completed in 2012, laid the foundation for further investigation into the role the microbiome plays in overall health and disease. One area of particular interest is the role which delivery mode plays in the development of the infant/neonate microbiome and what potential implications this may have long term. It has been found that infants born via vaginal delivery have microbiomes closely mirroring that of the mother's vaginal microbiome, whereas those born via cesarean section tend to resemble that of the mother's skin. One notable study from 2010 illustrated an abundance of Lactobacillus and other typical vaginal genera in stool samples of infants born via vaginal delivery and an abundance of Staphylococcus and Corynebacterium, commonly found on the skin surfaces, in stool samples of infants born via cesarean section. From these discoveries came the concept of vaginal seeding, also known as microbirthing, which is a procedure whereby vaginal fluids are applied to a new-born child delivered by caesarean section. The idea of vaginal seeding was explored in 2015 after Maria Gloria Dominguez-Bello discovered that birth by caesarean section significantly altered the newborn child's microbiome compared to that of natural birth. The purpose of the technique is to recreate the natural transfer of bacteria that the baby gets during a vaginal birth. It involves placing swabs in the mother's vagina, and then wiping them onto the baby's face, mouth, eyes and skin. Due to the long-drawn nature of studying the impact of vaginal seeding, there are a limited number of studies available that support or refute its use. The evidence suggests that applying microbes from the mother's vaginal canal to the baby after cesarean section may aid in the partial restoration of the infant's natural gut microbiome with an increased likelihood of pathogenic infection to the child via vertical transmission.

The uterine microbiome is the commensal, nonpathogenic, bacteria, viruses, yeasts/fungi present in a healthy uterus, amniotic fluid and endometrium and the specific environment which they inhabit. It has been only recently confirmed that the uterus and its tissues are not sterile. Due to improved 16S rRNA gene sequencing techniques, detection of bacteria that are present in low numbers is possible. Using this procedure that allows the detection of bacteria that cannot be cultured outside the body, studies of microbiota present in the uterus are expected to increase.