A skin condition, also known as cutaneous condition, is any medical condition that affects the integumentary system—the organ system that encloses the body and includes skin, nails, and related muscle and glands. The major function of this system is as a barrier against the external environment.

Lichen planus (LP) is a chronic inflammatory and immune-mediated disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, and is only named that because it looks like one. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

Hyperpigmentation is the darkening of an area of skin or nails caused by increased melanin.

Mycosis fungoides, also known as Alibert-Bazin syndrome or granuloma fungoides, is the most common form of cutaneous T-cell lymphoma. It generally affects the skin, but may progress internally over time. Symptoms include rash, tumors, skin lesions, and itchy skin.

Cutaneous T cell lymphoma (CTCL) is a class of non-Hodgkin lymphoma, which is a type of cancer of the immune system. Unlike most non-Hodgkin lymphomas, CTCL is caused by a mutation of T cells. The cancerous T cells in the body initially migrate to the skin, causing various lesions to appear. These lesions change shape as the disease progresses, typically beginning as what appears to be a rash which can be very itchy and eventually forming plaques and tumors before spreading to other parts of the body.
PUVA is an ultraviolet light therapy treatment for skin diseases: eczema, psoriasis, graft-versus-host disease, vitiligo, mycosis fungoides, large plaque parapsoriasis, and cutaneous T-cell lymphoma, using the sensitizing effects of the drug psoralen. The psoralen is applied or taken orally to sensitize the skin, then the skin is exposed to UVA.

Chlormethine, also known as mechlorethamine, mustine, HN2, and embikhin (эмбихин), is a nitrogen mustard sold under the brand name Mustargen among others. It is the prototype of alkylating agents, a group of anticancer chemotherapeutic drugs. It works by binding to DNA, crosslinking two strands and preventing cell duplication. It binds to the N7 nitrogen on the DNA base guanine. As the chemical is a blister agent, its use is strongly restricted within the Chemical Weapons Convention where it is classified as a Schedule 1 substance.

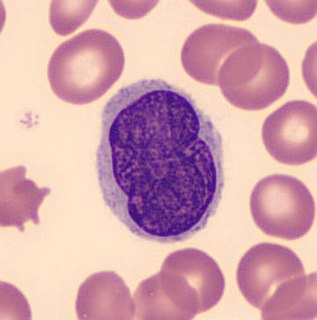
Sézary disease, or Sézary syndrome, is a type of cutaneous T-cell lymphoma that was first described by Albert Sézary. The affected T cells, known as Sézary's cells or Lutzner cells, have pathological quantities of mucopolysaccharides. Sézary disease is sometimes considered a late stage of mycosis fungoides with lymphadenopathy.

Rothmund–Thomson syndrome (RTS) is a rare autosomal recessive skin condition.
Large plaque parapsoriasis are skin lesions that may be included in the modern scheme of cutaneous conditions described as parapsoriasis. These lesions, called plaques, may be irregularly round-shaped to oval and are 10 cm (4 in) or larger in diameter. They can be very thin plaques that are asymptomatic or mildly pruritic. Large-plaque parapsoriasis is a common associate of retiform parapsoriasis, can be accompanied by poikiloderma vasculare atrophicans, and can in rare occasions be a precursor to cutaneous T-cell lymphoma.

Cutaneous lymphoid hyperplasia refers to a groups of benign cutaneous disorders characterized by collections of lymphocytes, macrophages, and dendritic cells in the skin. Conditions included in this groups are:
Pagetoid reticulosis is a cutaneous condition, an uncommon lymphoproliferative disorder, sometimes considered a form of mycosis fungoides.
Granulomatous slack skin (GSS) is a rare cutaneous condition, a variant of lymphoma that typically presents in middle-aged adults.
Non-mycosis fungoides CD30− cutaneous large T-cell lymphoma is a cutaneous condition that usually presents as solitary or generalized plaques, nodules, or tumors of short duration.
Pleomorphic T-cell lymphoma is a cutaneous condition characterized by a 5-year survival rate of 62%.
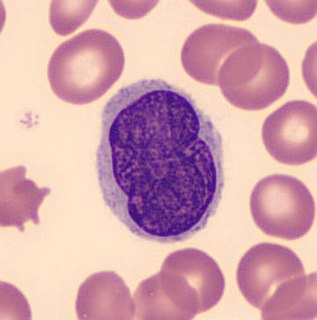
Lutzner cells were discovered by Marvin A. Lutzner, Lucien-Marie Pautrier, and Albert Sézary. These cells are described as the smaller forms of Sézary cells, or Sézary-Lutzner cells, and the two variants are recognised as being morphologically different. Aggregates of these cells in mycosis fungoides are known as a Pautrier's microabscesses. They are a form of T-lymphocytes that has been mutated This atypical form of T-lymphocytes contains T-cell receptors on the surface and is found in both the dermis and epidermis layers of the skin. Since Lutzner cells are a mutated form of T-lymphocytes, they develop in bone marrow and are transported to the thymus is order to mature. The production and maturation stages occur before the cell has developed a mutation. Lutzner cells can form cutaneous T-cell lymphoma, which is a form of skin cancer.
Retiform parapsoriasis is a cutaneous condition, considered to be a type of large-plaque parapsoriasis. It is characterized by widespread, ill-defined plaques on the skin, that have a net-like or zebra-striped pattern. Skin atrophy, a wasting away of the cutaneous tissue, usually occurs within the area of these plaques.

Poikiloderma is a skin condition that consists of areas of hypopigmentation, hyperpigmentation, telangiectasias and atrophy. Poikiloderma of Civatte is most frequently seen on the chest or the neck, characterized by red colored pigment on the skin that is commonly associated with sun damage.
Poikiloderma of Civatte is a cutaneous condition and refers to reticulated red to red-brown skin patches with telangiectasias. It is identifiable as a reddish-brown discoloration on the side of the neck, usually on both sides. It is more common in lighter-skinned individuals, in females rather than in males and more often affects middle-aged to elderly women. This disease is basically a change of the skin due to dilation of the blood vessels in the neck. "Civatte" was the French dermatologist who first identified it in the 1920s.