Related Research Articles

Antipsychotics, also known as neuroleptics, are a class of psychotropic medication primarily used to manage psychosis, principally in schizophrenia but also in a range of other psychotic disorders. They are also the mainstay together with mood stabilizers in the treatment of bipolar disorder.
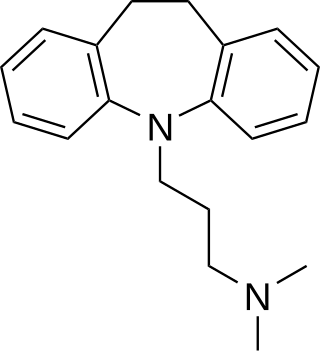
Tricyclic antidepressants (TCAs) are a class of medications that are used primarily as antidepressants, which is important for the management of depression. They are second-line drugs next to SSRIs. TCAs were discovered in the early 1950s and were marketed later in the decade. They are named after their chemical structure, which contains three rings of atoms. Tetracyclic antidepressants (TeCAs), which contain four rings of atoms, are a closely related group of antidepressant compounds.

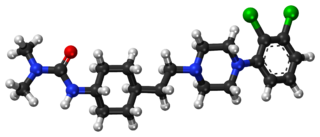
Chlorpromazine (CPZ), marketed under the brand names Thorazine and Largactil among others, is an antipsychotic medication. It is primarily used to treat psychotic disorders such as schizophrenia. Other uses include the treatment of bipolar disorder, severe behavioral problems in children including those with attention deficit hyperactivity disorder, nausea and vomiting, anxiety before surgery, and hiccups that do not improve following other measures. It can be given orally, by intramuscular injection, or intravenously.

Haloperidol, sold under the brand name Haldol among others, is a typical antipsychotic medication. Haloperidol is used in the treatment of schizophrenia, tics in Tourette syndrome, mania in bipolar disorder, delirium, agitation, acute psychosis, and hallucinations from alcohol withdrawal. It may be used by mouth or injection into a muscle or a vein. Haloperidol typically works within 30 to 60 minutes. A long-acting formulation may be used as an injection every four weeks by people with schizophrenia or related illnesses, who either forget or refuse to take the medication by mouth.

Typical antipsychotics are a class of antipsychotic drugs first developed in the 1950s and used to treat psychosis. Typical antipsychotics may also be used for the treatment of acute mania, agitation, and other conditions. The first typical antipsychotics to come into medical use were the phenothiazines, namely chlorpromazine which was discovered serendipitously. Another prominent grouping of antipsychotics are the butyrophenones, an example of which is haloperidol. The newer, second-generation antipsychotics, also known as atypical antipsychotics, have largely supplanted the use of typical antipsychotics as first-line agents due to the higher risk of movement disorders in the latter.

The atypical antipsychotics (AAP), also known as second generation antipsychotics (SGAs) and serotonin–dopamine antagonists (SDAs), are a group of antipsychotic drugs largely introduced after the 1970s and used to treat psychiatric conditions. Some atypical antipsychotics have received regulatory approval for schizophrenia, bipolar disorder, irritability in autism, and as an adjunct in major depressive disorder.

Ziprasidone, sold under the brand name Geodon among others, is an atypical antipsychotic used to treat schizophrenia and bipolar disorder. It may be used by mouth and by injection into a muscle (IM). The IM form may be used for acute agitation in people with schizophrenia.

Akathisia is a movement disorder characterized by a subjective feeling of inner restlessness accompanied by mental distress and an inability to sit still. Usually, the legs are most prominently affected. Those affected may fidget, rock back and forth, or pace, while some may just have an uneasy feeling in their body. The most severe cases may result in aggression, violence, and/or suicidal thoughts. Akathisia is also associated with threatening behaviour and physical aggression that is greatest in patients with mild akathisia, and diminishing with increasing severity of akathisia.
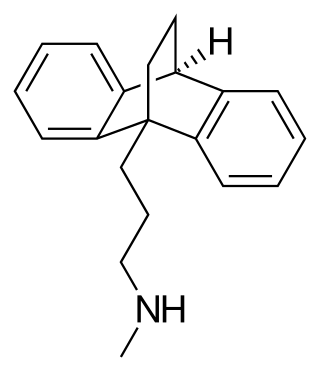
Maprotiline, sold under the brand name Ludiomil among others, is a tetracyclic antidepressant (TeCA) that is used in the treatment of depression. It may alternatively be classified as a tricyclic antidepressant (TCA), specifically a secondary amine. In terms of its chemistry and pharmacology, maprotiline is closely related to other secondary amine TCAs like nortriptyline and protriptyline, and has similar effects to them.

Azapirones are a class of drugs used as anxiolytics, antidepressants, and antipsychotics. They are commonly used as add-ons to other antidepressants, such as selective serotonin reuptake inhibitors (SSRIs).
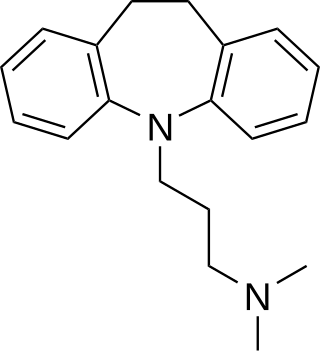
Imipramine, sold under the brand name Tofranil, among others, is a tricyclic antidepressant (TCA) mainly used in the treatment of depression. It is also effective in treating anxiety and panic disorder. Imipramine may also be used off-label for nocturnal enuresis and chronic pain. Imipramine is taken by mouth.
Biological psychiatry or biopsychiatry is an approach to psychiatry that aims to understand mental disorder in terms of the biological function of the nervous system. It is interdisciplinary in its approach and draws on sciences such as neuroscience, psychopharmacology, biochemistry, genetics, epigenetics and physiology to investigate the biological bases of behavior and psychopathology. Biopsychiatry is the branch of medicine which deals with the study of the biological function of the nervous system in mental disorders.

Trimipramine, sold under the brand name Surmontil among others, is a tricyclic antidepressant (TCA) which is used to treat depression. It has also been used for its sedative, anxiolytic, and weak antipsychotic effects in the treatment of insomnia, anxiety disorders, and psychosis, respectively. The drug is described as an atypical or "second-generation" TCA because, unlike other TCAs, it seems to be a fairly weak monoamine reuptake inhibitor. Similarly to other TCAs however, trimipramine does have antihistamine, antiserotonergic, antiadrenergic, antidopaminergic, and anticholinergic activities.

Chlorprothixene, sold under the brand name Truxal among others, is a typical antipsychotic of the thioxanthene group.

Amisulpride is an antiemetic and antipsychotic medication used at lower doses intravenously to prevent and treat postoperative nausea and vomiting; and at higher doses by mouth to treat schizophrenia and acute psychotic episodes. It is sold under the brand names Barhemsys and Solian, Socian, Deniban and others. At very low doses it is also used to treat dysthymia.

Dibenzepin, sold under the brand name Noveril among others, is a tricyclic antidepressant (TCA) used widely throughout Europe for the treatment of depression. It has similar efficacy and effects relative to other TCAs like imipramine but with fewer side effects.

Sulpiride, sold under the brand name Dogmatil among others, is an atypical antipsychotic medication of the benzamide class which is used mainly in the treatment of psychosis associated with schizophrenia and major depressive disorder, and sometimes used in low dosage to treat anxiety and mild depression. Sulpiride is commonly used in Asia, Central America, Europe, South Africa and South America. Levosulpiride is its purified levo-isomer and is sold in India for similar purpose. It is not approved in the United States, Canada, or Australia. The drug is chemically and clinically similar to amisulpride.
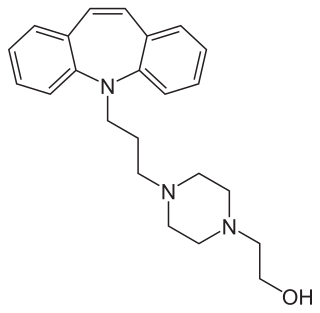
Opipramol, sold under the brand name Insidon among others, is an anxiolytic and tricyclic antidepressant that is used throughout Europe. Despite chemically being a tricyclic dibenzazepine (iminostilbene) derivative similar to imipramine, opipramol is not a monoamine reuptake inhibitor like most other tricyclic antidepressants, and instead, uniquely among antidepressants, acts primarily as a SIGMAR1 agonist. It was developed by Schindler and Blattner in 1961.

Medifoxamine, previously sold under the brand names Clédial and Gerdaxyl, is an atypical antidepressant with additional anxiolytic properties acting via dopaminergic and serotonergic mechanisms which was formerly marketed in France and Spain, as well as Morocco. The drug was first introduced in France sometime around 1990. It was withdrawn from the market in 1999 (Morocco) and 2000 (France) following incidences of hepatotoxicity.
Cariprazine, sold under the brand names Vraylar and Reagila among others, is an atypical antipsychotic originated by Gedeon Richter, which is used in the treatment of schizophrenia, bipolar mania, bipolar depression, and major depressive disorder. It acts primarily as a D3 and D2 receptor partial agonist, with a preference for the D3 receptor. Cariprazine is also a partial agonist at the serotonin 5-HT1A receptor and acts as an antagonist at 5-HT2B and 5-HT2A receptors, with high selectivity for the D3 receptor. It is taken by mouth.
References
- ↑ Rosenbloom, M (2002). "Chlorpromazine and the psychopharmacologic revolution". JAMA: The Journal of the American Medical Association. 287 (14): 1860–1. doi:10.1001/jama.287.14.1860. PMID 11939878.
- ↑ Ban, TA (2007). "Fifty years chlorpromazine: a historical perspective". Neuropsychiatric Disease and Treatment. 3 (4): 495–500. PMC 2655089 . PMID 19300578.
- 1 2 3 López-Muñoz, F.; Alamo, C. (2009). "Monoaminergic neurotransmission: the history of the discovery of antidepressants from 1950s until today". Current Pharmaceutical Design. 15 (14): 1563–1586. doi:10.2174/138161209788168001. PMID 19442174.
- ↑ Baumeister, A. A.; Francis, J. L. (2002). "Historical development of the dopamine hypothesis of schizophrenia". Journal of the History of the Neurosciences. 11 (3): 265–277. doi:10.1076/jhin.11.3.265.10391. PMID 12481477. S2CID 25572061.
- ↑ Baumeister, Alan; Hawkins, Mike (2005). "Continuity and Discontinuity in the Historical Development of Modern Psychopharmacology". Journal of the History of the Neurosciences. 14 (3): 199–209. doi:10.1080/096470490512562. PMID 16188699. S2CID 22697604.
- ↑ Ban, T. A. (2001). "Pharmacotherapy of depression: a historical analysis". Journal of Neural Transmission. 108 (6): 707–716. doi:10.1007/s007020170047. PMID 11478422. S2CID 19966517.
- ↑ Tenore, P. L. (2008). "Psychotherapeutic Benefits of Opioid Agonist Therapy". Journal of Addictive Diseases. 27 (3): 49–65. doi:10.1080/10550880802122646. PMID 18956529. S2CID 25882791.
- ↑ López-Muñoz, F; Ucha-Udabe, R; Alamo, C (2005). "The history of barbiturates a century after their clinical introduction". Neuropsychiatric Disease and Treatment. 1 (4): 329–43. PMC 2424120 . PMID 18568113.
- ↑ Ban, TA (2001). "Pharmacotherapy of mental illness--a historical analysis". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 25 (4): 709–27. doi:10.1016/s0278-5846(01)00160-9. PMID 11383974. S2CID 20630716.