Related Research Articles

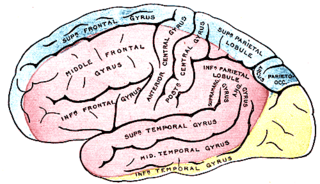
Expressive aphasia, also known as Broca's aphasia, is a type of aphasia characterized by partial loss of the ability to produce language, although comprehension generally remains intact. A person with expressive aphasia will exhibit effortful speech. Speech generally includes important content words but leaves out function words that have more grammatical significance than physical meaning, such as prepositions and articles. This is known as "telegraphic speech". The person's intended message may still be understood, but their sentence will not be grammatically correct. In very severe forms of expressive aphasia, a person may only speak using single word utterances. Typically, comprehension is mildly to moderately impaired in expressive aphasia due to difficulty understanding complex grammar.
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body. Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, or stroke.
Anosognosia is a condition in which a person with a disability is cognitively unaware of having it due to an underlying physical condition. Anosognosia results from physiological damage to brain structures, typically to the parietal lobe or a diffuse lesion on the fronto-temporal-parietal area in the right hemisphere, and is thus a neuropsychiatric disorder. A deficit of self-awareness, it was first named by the neurologist Joseph Babinski in 1914.
Lateral medullary syndrome is a neurological disorder causing a range of symptoms due to ischemia in the lateral part of the medulla oblongata in the brainstem. The ischemia is a result of a blockage most commonly in the vertebral artery or the posterior inferior cerebellar artery. Lateral medullary syndrome is also called Wallenberg's syndrome, posterior inferior cerebellar artery (PICA) syndrome and vertebral artery syndrome.

Hemispatial neglect is a neuropsychological condition in which, after damage to one hemisphere of the brain, a deficit in attention and awareness towards the side of space opposite brain damage is observed. It is defined by the inability of a person to process and perceive stimuli towards the contralesional side of the body or environment. Hemispatial neglect is very commonly contralateral to the damaged hemisphere, but instances of ipsilesional neglect have been reported.

Global aphasia is a severe form of nonfluent aphasia, caused by damage to the left side of the brain, that affects receptive and expressive language skills as well as auditory and visual comprehension. Acquired impairments of communicative abilities are present across all language modalities, impacting language production, comprehension, and repetition. Patients with global aphasia may be able to verbalize a few short utterances and use non-word neologisms, but their overall production ability is limited. Their ability to repeat words, utterances, or phrases is also affected. Due to the preservation of the right hemisphere, an individual with global aphasia may still be able to express themselves through facial expressions, gestures, and intonation. This type of aphasia often results from a large lesion of the left perisylvian cortex. The lesion is caused by an occlusion of the left middle cerebral artery and is associated with damage to Broca's area, Wernicke's area, and insular regions which are associated with aspects of language.
The primary goals of stroke management are to reduce brain injury and promote maximum patient recovery. Rapid detection and appropriate emergency medical care are essential for optimizing health outcomes. When available, patients are admitted to an acute stroke unit for treatment. These units specialize in providing medical and surgical care aimed at stabilizing the patient's medical status. Standardized assessments are also performed to aid in the development of an appropriate care plan. Current research suggests that stroke units may be effective in reducing in-hospital fatality rates and the length of hospital stays.

Intraparenchymal hemorrhage (IPH) is one form of intracerebral bleeding in which there is bleeding within brain parenchyma. The other form is intraventricular hemorrhage (IVH).

Brain herniation is a potentially deadly side effect of very high pressure within the skull that occurs when a part of the brain is squeezed across structures within the skull. The brain can shift across such structures as the falx cerebri, the tentorium cerebelli, and even through the foramen magnum. Herniation can be caused by a number of factors that cause a mass effect and increase intracranial pressure (ICP): these include traumatic brain injury, intracranial hemorrhage, or brain tumor.
The posterior cerebral artery (PCA) is one of a pair of cerebral arteries that supply oxygenated blood to the occipital lobe, part of the back of the human brain. The two arteries originate from the distal end of the basilar artery, where it bifurcates into the left and right posterior cerebral arteries. These anastomose with the middle cerebral arteries and internal carotid arteries via the posterior communicating arteries.

Foix–Chavany–Marie Syndrome (FCMS), also known as bilateral opercular syndrome, is a neuropathological disorder characterized by paralysis of the facial, tongue, pharynx, and masticatory muscles of the mouth that aid in chewing. The disorder is primarily caused by thrombotic and embolic strokes, which cause a deficiency of oxygen in the brain. As a result, bilateral lesions may form in the junctions between the frontal lobe and temporal lobe, the parietal lobe and cortical lobe, or the subcortical region of the brain. FCMS may also arise from defects existing at birth that may be inherited or nonhereditary. Symptoms of FCMS can be present in a person of any age and it is diagnosed using automatic-voluntary dissociation assessment, psycholinguistic testing, neuropsychological testing, and brain scanning. Treatment for FCMS depends on the onset, as well as on the severity of symptoms, and it involves a multidisciplinary approach.

Hemianopsia, or hemianopia, is a visual field loss on the left or right side of the vertical midline. It can affect one eye but usually affects both eyes.
Central facial palsy is a symptom or finding characterized by paralysis or paresis of the lower half of one side of the face. It usually results from damage to upper motor neurons of the facial nerve.

Weber's syndrome, also known as midbrain stroke syndrome or superior alternating hemiplegia, is a form of stroke that affects the medial portion of the midbrain. It involves oculomotor fascicles in the interpeduncular cisterns and cerebral peduncle so it characterizes the presence of an ipsilateral lower motor neuron type oculomotor nerve palsy and contralateral hemiparesis or hemiplegia.

Behavioral neurology is a subspecialty of neurology that studies the impact of neurological damage and disease upon behavior, memory, and cognition, and the treatment thereof. Two fields associated with behavioral neurology are neuropsychiatry and neuropsychology. In the United States, 'Behavioral Neurology & Neuropsychiatry' has been recognized as a single subspecialty by the United Council for Neurologic Subspecialties (UCNS) since 2004.
Middle cerebral artery syndrome is a condition whereby the blood supply from the middle cerebral artery (MCA) is restricted, leading to a reduction of the function of the portions of the brain supplied by that vessel: the lateral aspects of frontal, temporal and parietal lobes, the corona radiata, globus pallidus, caudate and putamen. The MCA is the most common site for the occurrence of ischemic stroke.
Kernohan's notch is a cerebral peduncle indentation associated with some forms of transtentorial herniation. It is a secondary condition caused by a primary injury on the opposite hemisphere of the brain. Kernohan's notch is an ipsilateral condition, in that a left-sided primary lesion evokes motor impairment in the left side of the body and a right-sided primary injury evokes motor impairment in the right side of the body. The seriousness of Kernohan's notch varies depending on the primary problem causing it, which may range from benign brain tumors to advanced subdural hematoma.
Amorphosynthesis, also called a hemi-sensory deficit, is a neuropsychological condition in which a patient experiences unilateral inattention to sensory input. This phenomenon is frequently associated with damage to the right cerebral hemisphere resulting in severe sensory deficits that are observed on the contralesional (left) side of the body. A right-sided deficit is less commonly observed and the effects are reported to be temporary and minor. Evidence suggests that the right cerebral hemisphere has a dominant role in attention and awareness to somatic sensations through ipsilateral and contralateral stimulation. In contrast, the left cerebral hemisphere is activated only by contralateral stimuli. Thus, the left and right cerebral hemispheres exhibit redundant processing to the right-side of the body and a lesion to the left cerebral hemisphere can be compensated by the ipsiversive processes of the right cerebral hemisphere. For this reason, right-sided amorphosynthesis is less often observed and is generally associated with bilateral lesions.
Alternating hemiplegia is a form of hemiplegia that has an ipsilateral cranial nerve palsies and contralateral hemiplegia or hemiparesis of extremities of the body. The disorder is characterized by recurrent episodes of paralysis on one side of the body. There are multiple forms of alternating hemiplegia, Weber's syndrome, middle alternating hemiplegia, and inferior alternating hemiplegia. This type of syndrome can result from a unilateral lesion in the brainstem affecting both upper motor neurons and lower motor neurons. The muscles that would receive signals from these damaged upper motor neurons result in spastic paralysis. With a lesion in the brainstem, this affects the majority of limb and trunk muscles on the contralateral side due to the upper motor neurons decussation after the brainstem. The cranial nerves and cranial nerve nuclei are also located in the brainstem making them susceptible to damage from a brainstem lesion. Cranial nerves III (Oculomotor), VI (Abducens), and XII (Hypoglossal) are most often associated with this syndrome given their close proximity with the pyramidal tract, the location which upper motor neurons are in on their way to the spinal cord. Damages to these structures produce the ipsilateral presentation of paralysis or palsy due to the lack of cranial nerve decussation before innervating their target muscles. The paralysis may be brief or it may last for several days, many times the episodes will resolve after sleep. Some common symptoms of alternating hemiplegia are mental impairment, gait and balance difficulties, excessive sweating and changes in body temperature.
Dyschiria, also known as dyschiric syndrome, is a neurological disorder where one-half of an individual's body or space cannot be recognized or respond to sensations. The term dyschiria is rarely used in modern scientific research and literature. Dyschiria has been often referred to as unilateral neglect, visuo-spatial neglect, or hemispatial neglect from the 20th century onwards. Psychologists formerly characterized dyschiric patients to be unable to discriminate or report external stimuli. This left the patients incapable of orienting sensory responses in their extrapersonal and personal space. Patients with dyschiria are unable to distinguish one side of their body in general, or specific segments of the body. There are three stages to dyschiria: achiria, allochiria, and synchiria, in which manifestations of dyschiria evolve in varying degrees.
References
- 1 2 3 4 5 6 Karnath HO, Broetz D (December 2003). "Understanding and treating "pusher syndrome"". Phys Ther. 83 (12): 1119–25. doi: 10.1093/ptj/83.12.1119 . PMID 14640870. Archived from the original on 2013-04-15.
- ↑ Karnath HO, Ferber S, Dichgans J (November 2000). "The origin of contraversive pushing: evidence for a second graviceptive system in humans". Neurology. 55 (9): 1298–304. doi:10.1212/wnl.55.9.1298. PMID 11087771. S2CID 19399616.
- ↑ Karnath HO, Ferber S, Dichgans J (December 2000). "The neural representation of postural control in humans". Proc. Natl. Acad. Sci. U.S.A. 97 (25): 13931–6. Bibcode:2000PNAS...9713931K. doi: 10.1073/pnas.240279997 . PMC 17678 . PMID 11087818.
- 1 2 Pedersen PM, Wandel A, Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS (January 1996). "Ipsilateral pushing in stroke: incidence, relation to neuropsychological symptoms, and impact on rehabilitation. The Copenhagen Stroke Study". Arch Phys Med Rehabil. 77 (1): 25–8. doi:10.1016/s0003-9993(96)90215-4. PMID 8554469.
- ↑ Davies, P.M. (1985). Steps to follow: A guide to the treatment of adult hemiplegia : Based on the concept of K. and B. Bobath. New York: Springer-Verlag.
- ↑ O'Sullivan, S. (2007). "Ch. 12: Stroke". In O'Sullivan, S.; Schmitz, T. (eds.). Physical Rehabilitation (5th ed.). Philadelphia: F.A. Davis. pp. 705–769. ISBN 9780803612471.
- ↑ Davies, Patricia M.; Bobath, B. (1985). Steps to follow : a guide to the treatment of adult hemiplegia (1st ed., 8th print. ed.). Berlin: Springer. ISBN 978-3-540-13436-7.