Related Research Articles

Headache is the symptom of pain in the face, head, or neck. It can occur as a migraine, tension-type headache, or cluster headache. Frequent headaches can affect relationships and employment. There is also an increased risk of depression in those with severe headaches.
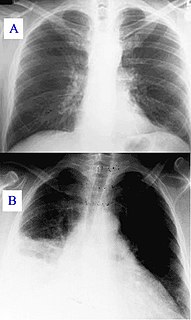
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, and sudden death.

Upper gastrointestinal bleeding is gastrointestinal bleeding in the upper gastrointestinal tract, commonly defined as bleeding arising from the esophagus, stomach, or duodenum. Blood may be observed in vomit or in altered form as black stool. Depending on the amount of the blood loss, symptoms may include shock.

Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consciousness, fever, and sometimes seizures. Neck stiffness or neck pain are also relatively common. In about a quarter of people a small bleed with resolving symptoms occurs within a month of a larger bleed.

A limp is a type of asymmetric abnormality of the gait. Limping may be caused by pain, weakness, neuromuscular imbalance, or a skeletal deformity. The most common underlying cause of a painful limp is physical trauma; however, in the absence of trauma, other serious causes, such as septic arthritis or slipped capital femoral epiphysis, may be present. The diagnostic approach involves ruling out potentially serious causes via the use of X-rays, blood tests, and sometimes joint aspiration. Initial treatment involves pain management. A limp is the presenting problem in about 4% of children who visit hospital emergency departments.
A thunderclap headache is a headache that is severe and has a sudden onset. It is defined as a severe headache that takes seconds to minutes to reach maximum intensity. Although approximately 75% are attributed to "primary" headaches—headache disorder, non-specific headache, idiopathic thunderclap headache, or uncertain headache disorder—the remainder are secondary to other causes, which can include some extremely dangerous acute conditions, as well as infections and other conditions. Usually, further investigations are performed to identify the underlying cause.
The pneumonia severity index (PSI) or PORT Score is a clinical prediction rule that medical practitioners can use to calculate the probability of morbidity and mortality among patients with community acquired pneumonia.

In medicine, the Ottawa ankle rules are a set of guidelines for clinicians to help decide if a patient with foot or ankle pain should be offered X-rays to diagnose a possible bone fracture. Before the introduction of the rules most patients with ankle injuries would have been imaged. However the vast majority of patients with unclear ankle injuries do not have bone fractures. As a result, many unnecessary X-rays were taken, which was costly, time consuming and a slight health risk due to radiation exposure.
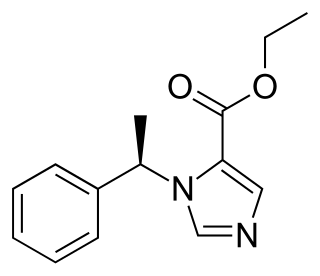
Etomidate is a short-acting intravenous anaesthetic agent used for the induction of general anaesthesia and sedation for short procedures such as reduction of dislocated joints, tracheal intubation, cardioversion and electroconvulsive therapy. It was developed at Janssen Pharmaceutica in 1964 and was introduced as an intravenous agent in 1972 in Europe and in 1983 in the United States.
CURB-65, also known as the CURB criteria, is a clinical prediction rule that has been validated for predicting mortality in community-acquired pneumonia and infection of any site. The CURB-65 is based on the earlier CURB score and is recommended by the British Thoracic Society for the assessment of severity of pneumonia. It was developed in 2002 at the University of Nottingham by Dr. W.S. Lim et al. In 2018 a new toolkit was presented on the basis of CURB-65.
Hospital-acquired pneumonia (HAP) or nosocomial pneumonia refers to any pneumonia contracted by a patient in a hospital at least 48–72 hours after being admitted. It is thus distinguished from community-acquired pneumonia. It is usually caused by a bacterial infection, rather than a virus.

Recursive partitioning is a statistical method for multivariable analysis. Recursive partitioning creates a decision tree that strives to correctly classify members of the population by splitting it into sub-populations based on several dichotomous independent variables. The process is termed recursive because each sub-population may in turn be split an indefinite number of times until the splitting process terminates after a particular stopping criterion is reached.
The Alvarado score is a clinical scoring system used in the diagnosis of appendicitis. The score has 6 clinical items and 2 laboratory measurements with a total 10 points. It was introduced in 1986 and although meant for pregnant females, it has been extensively validated in the non-pregnant population. The modified Alvarado score is at present in use. The Alvarado score has largely been superseded as a clinical prediction tool by the Appendicitis Inflammatory Response score.
Emergency ultrasound or point-of-care ultrasound (POCUS) is the application of ultrasound at the point of care to make immediate patient-care decisions. It is performed by the health care professional caring for the injured or ill persons. This point-of-care use of ultrasound is often to evaluate an emergency medical condition, in settings such as an emergency department, critical care unit, ambulance, or combat zone.

Syncope, also known as fainting, is a loss of consciousness and muscle strength characterized by a fast onset, short duration, and spontaneous recovery. It is caused by a decrease in blood flow to the brain, typically from low blood pressure. There are sometimes symptoms before the loss of consciousness such as lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, or feeling warm. Syncope may also be associated with a short episode of muscle twitching. When consciousness and muscle strength are not completely lost, it is called presyncope. It is recommended that presyncope be treated the same as syncope.

Electrocardiography in suspected myocardial infarction has the main purpose of detecting ischemia or acute coronary injury in emergency department populations coming for symptoms of myocardial infarction (MI). Also, it can distinguish clinically different types of myocardial infarction.
The Ottawa knee rules are a set of rules used to help physicians determine whether an x-ray of the knee is needed.
Permissive hypotension or hypotensive resuscitation is the use of restrictive fluid therapy, specifically in the trauma patient, that increases systemic blood pressure without reaching normotension. The goal blood pressure for these patients is a mean arterial pressure of 40-50mmHg or a systolic blood pressure less than or equal to 80. This goes along with certain clinical criteria. Following traumatic injury some patients experience hypotension that is usually due to blood loss (hemorrhage) but can be due to other causes as well. In the past, physicians were very aggressive with fluid resuscitation to try to bring the blood pressure to normal values. Recent studies have found that there is some benefit to allowing specific patients to experience some degree of hypotension in certain settings. This concept does not exclude therapy by means of i.v. fluid, inotropes or vasopressors, the only restriction is to avoid completely normalizing blood pressure in a context where blood loss may be enhanced. When a person starts to bleed the body starts a natural coagulation process that eventually stops the bleed. Issues with fluid resuscitation without control of bleeding is thought to be secondary to dislodgement of the thrombus that is helping to control further bleeding. Thrombus dislodgement was found to occur at a systolic pressure greater than 80mm Hg. In addition, fluid resuscitation will dilute coagulation factors that help form and stabilize a clot, hence making it harder for the body to use its natural mechanisms to stop the bleeding. These factors are aggravated by hypothermia.
Renal angina is a clinical methodology to risk stratify patients for the development of persistent and severe acute kidney injury (AKI). The composite of risk factors and early signs of injury for AKI, renal angina is used as a clinical adjunct to help optimize the use of novel AKI biomarker testing. The term angina from Latin and from the Greek ẚnkhone (“strangling”) are utilized in the context of AKI to denote the development of injury and the choking off of kidney function. Unlike angina pectoris, commonly caused due to ischemia of the heart muscle secondary to coronary artery occlusion or vasospasm, renal angina carries no obvious physical symptomatology. Renal angina was derived as a conceptual framework to identify evolving AKI. Like acute coronary syndrome which precedes or is a sign of a heart attack, renal angina is used as a herald sign for a kidney attack. Detection of renal angina is performed by calculating the renal angina index.
A sobering center is a facility or setting providing short-term recovery, detoxification, and recuperation from the effects of acute alcohol or drug intoxication. Sobering centers, instead, are fully staffed facilities providing oversight and ongoing monitoring throughout the sobering process. Sobering centers include alternatives to jail and emergency departments, as well as drop-in centers”. There are small numbers of sobering centers around the world. There are over 40 sobering centers in the United States, with dozens more in development.
References
- ↑ Quinn J; McDermott D; Stiell I; Kohn M; Wells G (May 2006). "Prospective validation of the San Francisco Syncope Rule to predict patients with serious outcomes". Ann Emerg Med. 47 (5): 448–54. doi:10.1016/j.annemergmed.2005.11.019. PMID 16631985.
- ↑ Birnbaum A; Esses D; Bijur P; Wollowitz A; Gallagher EJ (February 2008). "Failure to Validate the San Francisco Syncope Rule in an Independent Emergency Department Population". Ann Emerg Med. 52 (2): 151–9. doi:10.1016/j.annemergmed.2007.12.007. PMID 18282636.