Bipolar disorder, previously known as manic depression, is a mood disorder characterized by periods of depression and periods of abnormally-elevated happiness that last from days to weeks each. If the elevated mood is severe or associated with psychosis, it is called mania; if it is less severe, it is called hypomania. During mania, an individual behaves or feels abnormally energetic, happy or irritable, and they often make impulsive decisions with little regard for the consequences. There is usually also a reduced need for sleep during manic phases. During periods of depression, the individual may experience crying and have a negative outlook on life and poor eye contact with others. The risk of suicide is high; over a period of 20 years, 6% of those with bipolar disorder died by suicide, while 30–40% engaged in self-harm. Other mental health issues, such as anxiety disorders and substance use disorders, are commonly associated with bipolar disorder.

Bipolar I disorder is a type of bipolar spectrum disorder characterized by the occurrence of at least one manic episode, with or without mixed or psychotic features. Most people also, at other times, have one or more depressive episodes, and all experience a hypomanic stage before progressing to full mania.

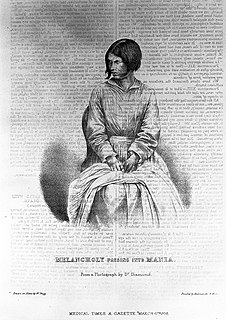
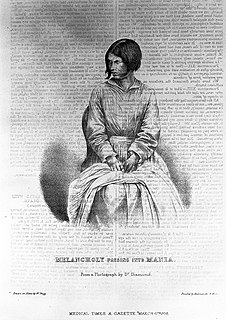
Mania, also known as manic syndrome, is a mental and behavioral disorder defined as a state of abnormally elevated arousal, affect, and energy level, or "a state of heightened overall activation with enhanced affective expression together with ability of affect." During a manic episode, an individual will experience rapidly changing emotions and moods, highly influenced by surrounding stimuli. Although mania is often conceived as a "mirror image" to depression, the heightened mood can be either euphoric or dysphoric. As the mania intensifies, irritability can be more pronounced and result in anxiety or anger.

A mood stabilizer is a psychiatric medication used to treat mood disorders characterized by intense and sustained mood shifts, such as bipolar disorder and the bipolar type of schizoaffective disorder.

Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.

A mood disorder, also known as an affective disorder, is any of a group of conditions of mental and behavioral disorder where a disturbance in the person's mood is the main underlying feature. The classification is in the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases (ICD).
Schizoaffective disorder is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis is made when the person has symptoms of both schizophrenia and a mood disorder: either bipolar disorder or depression. The main criterion for a diagnosis of schizoaffective disorder is the presence of psychotic symptoms for at least two weeks without any mood symptoms present. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, bipolar disorder with psychotic feature, schizophreniform disorder, or schizophrenia. It is imperative for providers to accurately diagnose patients, as treatment and prognosis differ greatly for each of these diagnoses.

Cognitive disorders (CDs), also known as neurocognitive disorders (NCDs), are a category of mental health disorders that primarily affect cognitive abilities including learning, memory, perception, and problem solving. Neurocognitive disorders include delirium, mild neurocognitive disorders, and major neurocognitive disorder. They are defined by deficits in cognitive ability that are acquired, typically represent decline, and may have an underlying brain pathology. The DSM-5 defines six key domains of cognitive function: executive function, learning and memory, perceptual-motor function, language, complex attention, and social cognition.
A mixed affective state, formerly known as a mixed-manic or mixed episode, has been defined as a state wherein features unique to both depression and mania—such as episodes of despair, doubt, anguish, rage or homicidal ideation, suicidal ideation, splitting, racing thoughts, sensory overload, pressure of activity, and heightened irritability—occur either simultaneously or in very short succession.
The emphasis of the treatment of bipolar disorder is on effective management of the long-term course of the illness, which can involve treatment of emergent symptoms. Treatment methods include pharmacological and psychological techniques.
Cyclical variations in moods and energy levels have been recorded at least as far back as several thousand years. The words "melancholia" and "mania" have their etymologies in Ancient Greek. The word melancholia is derived from melas/μελας, meaning "black", and chole/χολη, meaning "bile" or "gall", indicative of the term's origins in pre-Hippocratic humoral theories. A man known as Aretaeus of Cappadocia has the first records of analyzing the symptoms of depression and mania in the 1st century of Greece. There is documentation that explains how bath salts were used to calm those with manic symptoms and also help those who are dealing with depression. Even today, lithium is used as a treatment to bipolar disorder which is significant because lithium could have been an ingredient in the Greek bath salt. Centuries passed and very little was studied or discovered. It wasn't until the mid-19th century that a French psychiatrist by the name of Jean-Pierre Falret wrote an article describing "circular insanity" and this is believed to be the first recorded diagnosis of bipolar disorder. Years later, in the early 1900s, Emil Kraepelin, a German psychiatrist, analyzed the influence of biology on mental disorders, including bipolar disorder. His studies are still used as the basis of classification of mental disorders today.
Bipolar disorder in children, or pediatric bipolar disorder (PBD), is a controversial mental disorder in children and adolescents that is mainly diagnosed in the United States, and is hypothesized to be like bipolar disorder (BD) in adults, thus is proposed as an explanation for extreme changes in mood and behavior accompanying periods of depressed or irritable moods and periods of elevated moods so called manic or hypomanic episodes. These shifts are sometimes quick, but usually are gradual. The average age of onset of pediatric bipolar disorder is unclear, but the risk increases with the onset of puberty. Bipolar disorder is rare in childhood. Pediatric bipolar disorder is typically more severe and has a poorer prognosis than bipolar disorder with onset in late-adolescence or adulthood.

Bipolar II disorder (BP-II) is a mood disorder on the bipolar spectrum, characterized by at least one episode of hypomania and at least one episode of major depression. Diagnosis for BP-II requires that the individual must never have experienced a full manic episode. Otherwise, one manic episode meets the criteria for bipolar I disorder (BP-I).

Grandiose delusions (GD), also known as delusions of grandeur or expansive delusions, are a subtype of delusion that occur in patients with a wide range of psychiatric diseases, including two-thirds of patients in manic state of bipolar disorder, half of those with schizophrenia, patients with the grandiose subtype of delusional disorder, frequently in narcissistic personality disorder, and a substantial portion of those with substance abuse disorders. GDs are characterized by fantastical beliefs that one is famous, omnipotent, wealthy, or otherwise very powerful. The delusions are generally fantastic and typically have a religious, science fictional, or supernatural theme. There is a relative lack of research into GD, in contrast to persecutory delusions and auditory hallucinations. Around 10% of healthy people experience grandiose thoughts at some point in their lives but do not meet full criteria for a diagnosis of GD.
Brief psychotic disorder — according to the classifications of mental disorders DSM-IV-TR and DSM-5 — is a psychotic condition involving the sudden onset of at least one psychotic symptom lasting 1 day to 1 month, often accompanied by emotional turmoil. Remission of all symptoms is complete with patients returning to the previous level of functioning. It may follow a period of extreme stress including the loss of a loved one. Most patients with this condition under DSM-5 would be classified as having acute and transient psychotic disorders under ICD-10. Prior to DSM-IV, this condition was called "brief reactive psychosis." This condition may or may not be recurrent, and it should not be caused by another condition.

Early in the history of medicine, it was recognized that severe mental illness sometimes started abruptly in the days after childbirth, later known as postpartum psychosis or puerperal psychosis. Gradually, it became clear that this was not a single and unique phenomenon, but a group of at least twenty distinct disorders.
Cyclothymia, also known as cyclothymic disorder, psychothemia/psychothymia, bipolar III, affective personality disorder and cyclothymic personality disorder, is a mental and behavioural disorder that involves numerous periods of symptoms of depression and periods of symptoms of elevated mood. These symptoms, however, are not sufficient to indicate a major depressive episode or a manic episode. Symptoms must last for more than one year in children and two years in adults.
The associated features of bipolar disorder are clinical phenomena that often accompany bipolar disorder (BD) but are not part of the diagnostic criteria for the disorder. There are several childhood precursors in children who later receive a diagnosis of bipolar disorder. They may show subtle early traits such as mood abnormalities, full major depressive episodes, and attention-deficit hyperactivity disorder. BD is also accompanied by changes in cognition processes and abilities. This includes reduced attentional and executive capabilities and impaired memory. How the individual processes the world also depends on the phase of the disorder, with differential characteristics between the manic, hypomanic and depressive states. Some studies have found a significant association between bipolar disorder and creativity.
Hypomania is a mental and behavioural disorder, characterised essentially by an apparently non-contextual elevation of mood (euphoria) that contributes to persistently disinhibited behaviour.
Unipolar mania is an unrecognized mental illness characterized by episodes of mania and normal mood, with the absence of depressive symptoms. The concept has its origins as far back as the year 1889, when the German psychiatrist Emil Kraepelin first used the term of "periodic mania" to refer to people with recurrent manic episodes and no depression. One year later, Carl Wernicke proposed that mania and depression should be viewed as separate disorders. As the time went on, unipolar mania became an invalid diagnosis due to its variations across different patients. Currently patients with symptoms of mania, even in the absence of any depressive symptoms, would get the bipolar 1 diagnosis.