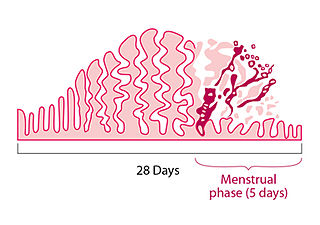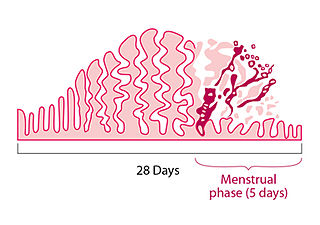
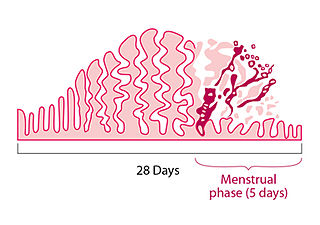
Menstruation is the regular discharge of blood and mucosal tissue from the inner lining of the uterus through the vagina. The menstrual cycle is characterized by the rise and fall of hormones. Menstruation is triggered by falling progesterone levels and is a sign that pregnancy has not occurred.
Menopause, also known as the climacteric, is the time when menstrual periods permanently stop, marking the end of reproduction. It typically occurs between the ages of 45 and 55, although the exact timing can vary. Menopause is usually a natural change. It can occur earlier in those who smoke tobacco. Other causes include surgery that removes both ovaries or some types of chemotherapy. At the physiological level, menopause happens because of a decrease in the ovaries' production of the hormones estrogen and progesterone. While typically not needed, a diagnosis of menopause can be confirmed by measuring hormone levels in the blood or urine. Menopause is the opposite of menarche, the time when a girl's periods start.

The menstrual cycle is a series of natural changes in hormone production and the structures of the uterus and ovaries of the female reproductive system that makes pregnancy possible. The ovarian cycle controls the production and release of eggs and the cyclic release of estrogen and progesterone. The uterine cycle governs the preparation and maintenance of the lining of the uterus (womb) to receive an embryo. These cycles are concurrent and coordinated, normally last between 21 and 35 days, with a median length of 28 days, and continue for about 30–45 years.
Premenstrual syndrome (PMS) is a disruptive set of emotional and physical symptoms that regularly occur in the one to two weeks before the start of each menstrual period. Symptoms resolve around the time menstrual bleeding begins. Different women experience different symptoms. Premenstrual syndrome commonly produces one or more physical, emotional, or behavioral symptoms, that resolve with menses. The range of symptoms is wide, and most commonly are breast tenderness, bloating, headache, mood swings, depression, anxiety, anger, and irritability. To be diagnosed as PMS, rather than a normal discomfort of the menstrual cycle, these symptoms must interfere with daily living, during two menstrual cycles of prospective recording. These symptoms are nonspecific and are seen in women without PMS. Often PMS-related symptoms are present for about six days. An individual's pattern of symptoms may change over time. PMS does not produce symptoms during pregnancy or following menopause.

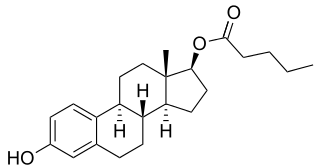
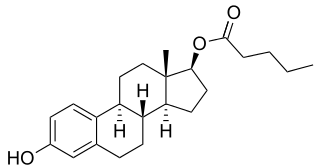
Estradiol (E2), also spelled oestradiol, is an estrogen steroid hormone and the major female sex hormone. It is involved in the regulation of female reproductive cycles such as estrous and menstrual cycles. Estradiol is responsible for the development of female secondary sexual characteristics such as the breasts, widening of the hips and a female pattern of fat distribution. It is also important in the development and maintenance of female reproductive tissues such as the mammary glands, uterus and vagina during puberty, adulthood and pregnancy. It also has important effects in many other tissues including bone, fat, skin, liver, and the brain.
Premenstrual dysphoric disorder (PMDD) is a mood disorder characterized by emotional, cognitive, and physical symptoms. PMDD causes significant distress or impairment in menstruating women during the luteal phase of the menstrual cycle. The symptoms occur in the luteal phase, improve within a few days after the onset of menses, and are minimal or absent in the week after menses. PMDD has a profound impact on a woman’s quality of life and dramatically increases the risk of suicidal ideation and even suicide attempts. Many women of reproductive age experience discomfort or mild mood changes prior to menstruation. However, 5–8% experience severe premenstrual syndrome causing significant distress or functional impairment. Within this population of reproductive age, some will meet the criteria for PMDD.

Vaginal bleeding is any expulsion of blood from the vagina. This bleeding may originate from the uterus, vaginal wall, or cervix. Generally, it is either part of a normal menstrual cycle or is caused by hormonal or other problems of the reproductive system, such as abnormal uterine bleeding.

Pregnancy is the time during which one or more offspring develops (gestates) inside a woman's uterus (womb). A multiple pregnancy involves more than one offspring, such as with twins.
Breast pain is the symptom of discomfort in either one or both breasts. Pain in both breasts is often described as breast tenderness, is usually associated with the menstrual period and is not serious. Pain that involves only one part of a breast is more concerning, particularly if a hard mass or nipple discharge is also present.

Complications of pregnancy are health problems that are related to, or arise during pregnancy. Complications that occur primarily during childbirth are termed obstetric labor complications, and problems that occur primarily after childbirth are termed puerperal disorders. While some complications improve or are fully resolved after pregnancy, some may lead to lasting effects, morbidity, or in the most severe cases, maternal or fetal mortality.
A menstrual disorder is characterized as any abnormal condition with regards to a woman's menstrual cycle. There are many different types of menstrual disorders that vary with signs and symptoms, including pain during menstruation, heavy bleeding, or absence of menstruation. Normal variations can occur in menstrual patterns but generally menstrual disorders can also include periods that come sooner than 21 days apart, more than 3 months apart, or last more than 10 days in duration. Variations of the menstrual cycle are mainly caused by the immaturity of the hypothalamic-pituitary-ovarian (HPO) axis, and early detection and management is required in order to minimize the possibility of complications regarding future reproductive ability.
Postpartum blues, also known as baby blues and maternity blues, is a very common but self-limited condition that begins shortly after childbirth and can present with a variety of symptoms such as mood swings, irritability, and tearfulness. Mothers may experience negative mood symptoms mixed with intense periods of joy. Up to 85% of new mothers are affected by postpartum blues, with symptoms starting within a few days after childbirth and lasting up to two weeks in duration. Treatment is supportive, including ensuring adequate sleep and emotional support. If symptoms are severe enough to affect daily functioning or last longer than two weeks, the individual should be evaluated for related postpartum psychiatric conditions, such as postpartum depression and postpartum anxiety. It is unclear whether the condition can be prevented, however education and reassurance are important to help alleviate patient distress.

Pruritic urticarial papules and plaques of pregnancy (PUPPP), known in United Kingdom as polymorphic eruption of pregnancy (PEP), is a chronic hives-like rash that strikes some women during pregnancy. Some skin changes are known to occur in people who are pregnant while other skin conditions, or dermatoses, that people have prior to getting pregnant will become altered or symptoms will increase. Pruritic urticarial papules and plaques of pregnancy (PUPPP) is one of many skin conditions that is specific to pregnancy and occurs in about 1 in every 160 (0.625%) of pregnancies.
Psychoneuroendocrinology is the clinical study of hormone fluctuations and their relationship to human behavior. It may be viewed from the perspective of psychiatry, where in certain mood disorders, there are associated neuroendocrine or hormonal changes affecting the brain. It may also be viewed from the perspective of endocrinology, where certain endocrine disorders can be associated with negative health outcomes and psychiatric illness. Brain dysfunctions associated with the hypothalamus-pituitary-adrenal axis HPA axis can affect the endocrine system, which in turn can result in physiological and psychological symptoms. This complex blend of psychiatry, psychology, neurology, biochemistry, and endocrinology is needed to comprehensively understand and treat symptoms related to the brain, endocrine system (hormones), and psychological health..

Postpartum psychosis (PPP), also known as puerperal psychosis or peripartum psychosis, involves the abrupt onset of psychotic symptoms shortly following childbirth, typically within two weeks of delivery but less than 4 weeks postpartum. PPP is a condition currently represented under "Brief Psychotic Disorder" in the Diagnostic and Statistical Manual of Mental Disorders, Volume V (DSM-V). Symptoms may include delusions, hallucinations, disorganized speech, and/or abnormal motor behavior. Other symptoms frequently associated with PPP include confusion, disorganized thought, severe difficulty sleeping, variations of mood disorders, as well as cognitive features such as consciousness that comes and goes or disorientation.

Catamenial epilepsy is a form of epilepsy in women where seizures are exacerbated during certain phases of the menstrual cycle. In rare cases, seizures occur only during certain parts of the cycle; in most cases, seizures occur more frequently during certain parts of the cycle. Catamenial epilepsy is underlain by hormonal fluctuations of the menstrual cycle where estrogens promote seizures and progesterone counteracts seizure activity.
Thyroid disease in pregnancy can affect the health of the mother as well as the child before and after delivery. Thyroid disorders are prevalent in women of child-bearing age and for this reason commonly present as a pre-existing disease in pregnancy, or after childbirth. Uncorrected thyroid dysfunction in pregnancy has adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Due to an increase in thyroxine binding globulin, an increase in placental type 3 deioidinase and the placental transfer of maternal thyroxine to the fetus, the demand for thyroid hormones is increased during pregnancy. The necessary increase in thyroid hormone production is facilitated by high human chorionic gonadotropin (hCG) concentrations, which bind the TSH receptor and stimulate the maternal thyroid to increase maternal thyroid hormone concentrations by roughly 50%. If the necessary increase in thyroid function cannot be met, this may cause a previously unnoticed (mild) thyroid disorder to worsen and become evident as gestational thyroid disease. Currently, there is not enough evidence to suggest that screening for thyroid dysfunction is beneficial, especially since treatment thyroid hormone supplementation may come with a risk of overtreatment. After women give birth, about 5% develop postpartum thyroiditis which can occur up to nine months afterwards. This is characterized by a short period of hyperthyroidism followed by a period of hypothyroidism; 20–40% remain permanently hypothyroid.
Women's reproductive health in the United States refers to the set of physical, mental, and social issues related to the health of women in the United States. It includes the rights of women in the United States to adequate sexual health, available contraception methods, and treatment for sexually transmitted diseases. The prevalence of women's health issues in American culture is inspired by second-wave feminism in the United States. As a result of this movement, women of the United States began to question the largely male-dominated health care system and demanded a right to information on issues regarding their physiology and anatomy. The U.S. government has made significant strides to propose solutions, like creating the Women's Health Initiative through the Office of Research on Women's Health in 1991. However, many issues still exist related to the accessibility of reproductive healthcare as well as the stigma and controversy attached to sexual health, contraception, and sexually transmitted diseases.
High-dose estrogen therapy (HDE) is a type of hormone therapy in which high doses of estrogens are given. When given in combination with a high dose of progestogen, it has been referred to as pseudopregnancy. It is called this because the estrogen and progestogen levels achieved are in the range of the very high levels of these hormones that occur during pregnancy. HDE and pseudopregnancy have been used in medicine for a number of hormone-dependent indications, such as breast cancer, prostate cancer, and endometriosis, among others. Both natural or bioidentical estrogens and synthetic estrogens have been used and both oral and parenteral routes may be used.
Menstruation can have a notable impact on mental health, with some individuals experiencing mood disturbances and psychopathological symptoms during their menstrual cycle. Menstruation involves hormonal fluctuations and physiological changes in the body, which can affect a person's mood and psychological state. Many individuals report experiencing mood swings, irritability, anxiety, and even depression in the days leading up to their menstrual period. This cluster of symptoms is often referred to as premenstrual syndrome (PMS). For some individuals, the psychopathological symptoms associated with menstruation can be severe and debilitating, leading to a condition known as premenstrual dysphoric disorder (PMDD). PMDD is characterized by intense mood disturbances, cognitive, and somatic symptoms, which occur in a cyclical pattern linked to the menstrual cycle. In addition to PMDD, menstruation can exacerbate existing mental health conditions. The complex relationship between menstruation and mental well-being has garnered increased attention in both scientific research and public discourse.