Related Research Articles

Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid agonist used for chronic pain and also for opioid use disorder. It is used to treat chronic pain, and it is also used to treat addiction to heroin or other opioids. Prescribed for daily use, the medicine relieves cravings and removes withdrawal symptoms. Withdrawal management using methadone can be accomplished in less than a month, or it may be done gradually over a longer period of time, or simply maintained for the rest of the patient's life. While a single dose has a rapid effect, maximum effect can take up to five days of use. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.

A poison is any chemical substance that is harmful or lethal to living organisms. The term is used in a wide range of scientific fields and industries, where it is often specifically defined. It may also be applied colloquially or figuratively, with a broad sense.

Methotrexate (MTX), formerly known as amethopterin, is a chemotherapy agent and immune-system suppressant. It is used to treat cancer, autoimmune diseases, and ectopic pregnancies. Types of cancers it is used for include breast cancer, leukemia, lung cancer, lymphoma, gestational trophoblastic disease, and osteosarcoma. Types of autoimmune diseases it is used for include psoriasis, rheumatoid arthritis, and Crohn's disease. It can be given by mouth or by injection.

Wernicke-Korsakoff syndrome (WKS) is the combined presence of Wernicke encephalopathy (WE) and Korsakoff syndrome. Due to the close relationship between these two disorders, people with either are usually diagnosed with WKS as a single syndrome. It mainly causes vision changes, ataxia and impaired memory.

Colchicine is a medication used to treat gout and Behçet's disease. In gout, it is less preferred than NSAIDs or steroids. Other uses for colchicine include the management of pericarditis and familial Mediterranean fever. Colchicine is taken by mouth.
Encephalopathy means any disorder or disease of the brain, especially chronic degenerative conditions. In modern usage, encephalopathy does not refer to a single disease, but rather to a syndrome of overall brain dysfunction; this syndrome has many possible organic and inorganic causes.

Hepatotoxicity implies chemical-driven liver damage. Drug-induced liver injury is a cause of acute and chronic liver disease caused specifically by medications and the most common reason for a drug to be withdrawn from the market after approval.
Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids. Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are important components of opioid use disorder.

Acute liver failure is the appearance of severe complications rapidly after the first signs of liver disease, and indicates that the liver has sustained severe damage. The complications are hepatic encephalopathy and impaired protein synthesis. The 1993 classification defines hyperacute as within 1 week, acute as 8–28 days, and subacute as 4–12 weeks; both the speed with which the disease develops and the underlying cause strongly affect outcomes.
Nephrotoxicity is toxicity in the kidneys. It is a poisonous effect of some substances, both toxic chemicals and medications, on kidney function. There are various forms, and some drugs may affect kidney function in more than one way. Nephrotoxins are substances displaying nephrotoxicity.

Abrin is an extremely toxic toxalbumin found in the seeds of the rosary pea, Abrus precatorius. It has a median lethal dose of 0.7 micrograms per kilogram of body mass when given to mice intravenously. The median toxic dose for humans ranges from 10 to 1000 micrograms per kilogram when ingested and is 3.3 micrograms per kilogram when inhaled.

Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris, aspiration, herbicides or fluorocarbons and some systemic diseases. If unresolved, continued inflammation can result in irreparable damage such as pulmonary fibrosis.
Toxic encephalopathy is a neurologic disorder caused by exposure to neurotoxic organic solvents such as toluene, following exposure to heavy metals such as manganese, as a side effect of melarsoprol treatment for African trypanosomiasis, adverse effects to prescription drugs, or exposure to extreme concentrations of any natural toxin such as cyanotoxins found in shellfish or freshwater cyanobacteria crusts. Toxic encephalopathy can occur following acute or chronic exposure to neurotoxicants, which includes all natural toxins. Exposure to toxic substances can lead to a variety of symptoms, characterized by an altered mental status, memory loss, and visual problems. Toxic encephalopathy can be caused by various chemicals, some of which are commonly used in everyday life, or cyanotoxins which are bio-accumulated from harmful algal blooms (HABs) which have settled on the benthic layer of a waterbody. Toxic encephalopathy can permanently damage the brain and currently treatment is mainly just for the symptoms.

"Chasing the dragon" (CTD), or "foily" in Australian English, refers to inhaling the vapor of a powdered psychoactive drug off a heated sheet of aluminum foil. The moving vapor is chased after with a tube through which the user inhales. The "chasing" occurs as the user gingerly keeps the liquid moving in order to keep it from overheating and burning up too quickly, on a heat conducting material such as aluminium foil.

Posterior reversible encephalopathy syndrome (PRES), also known as reversible posterior leukoencephalopathy syndrome (RPLS), is a rare condition in which parts of the brain are affected by swelling, usually as a result of an underlying cause. Someone with PRES may experience headaches, changes in vision, and seizures, with some developing other neurological symptoms such as confusion or weakness of one or more limbs. The name of the condition includes the word "posterior" because it predominantly though not exclusively affects the back of the brain. Common underlying causes are severely elevated blood pressure, kidney failure, severe infections, certain medications, some autoimmune diseases, and pre-eclampsia. The diagnosis is usually made by a brain scan (MRI) on which areas of swelling can be identified.
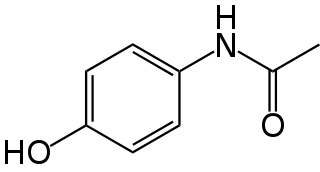
Paracetamol poisoning, also known as acetaminophen poisoning, is caused by excessive use of the medication paracetamol (acetaminophen). Most people have few or non-specific symptoms in the first 24 hours following overdose. These symptoms include feeling tired, abdominal pain, or nausea. This is typically followed by absence of symptoms for a couple of days, after which yellowish skin, blood clotting problems, and confusion occurs as a result of liver failure. Additional complications may include kidney failure, pancreatitis, low blood sugar, and lactic acidosis. If death does not occur, people tend to recover fully over a couple of weeks. Without treatment, death from toxicity occurs 4 to 18 days later.
An equianalgesic chart is a conversion chart that lists equivalent doses of analgesics. Equianalgesic charts are used for calculation of an equivalent dose between different analgesics. Tables of this general type are also available for NSAIDs, benzodiazepines, depressants, stimulants, anticholinergics and others.

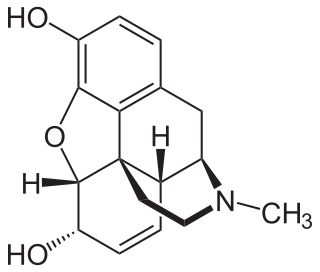
An opiate is an alkaloid substance derived from opium It has a different meaning from the similar term opioid, used to designate all substances, both natural and synthetic, that bind to opioid receptors in the brain. Opiates are alkaloid compounds naturally found in the opium poppy plant Papaver somniferum. The psychoactive compounds found in the opium plant include morphine, codeine, and thebaine. Opiates have long been used for a variety of medical conditions, with evidence of opiate trade and use for pain relief as early as the eighth century AD. Most opiates are considered drugs with moderate to high abuse potential and are listed on various "Substance-Control Schedules" under the Uniform Controlled Substances Act of the United States of America.
Grinker's myelinopathy, also known as anoxic leukoencephalopathy, is a rare disease of the central nervous system. The disease is characterized by a delayed leukoencephalopathy after a hypoxic episode. It is typically, though not necessarily, related to carbon monoxide poisoning or heroin overdose. It occurs in roughly 2.8% of those who experience an acute hypoxic/anoxic episode. Because of the wide range of symptoms and the delay in onset, it is often misdiagnosed as other neuropathologies. Grinker's myelinopathy was originally characterized by Roy R. Grinker in 1925 or 1926, depending on the source.
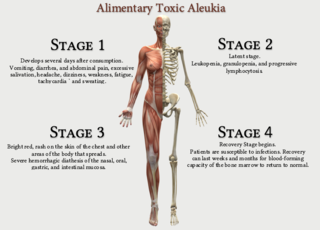
Alimentary toxic aleukia is a mycotoxin-induced condition characterized by nausea, vomiting, diarrhea, leukopenia (aleukia), hemorrhaging, skin inflammation, and sometimes death. Alimentary toxic aleukia almost always refers to the human condition associated with presence of T-2 Toxin.
References
- 1 2 3 4 5 Hagel J, Andrews G, Vertinsky T, Heran MK, Keogh C (October 2005). ""Chasing the dragon" - Imaging of heroin inhalation leukoencephalopathy". Canadian Association of Radiologists Journal. 56 (4): 199–203. PMID 16419370.
- 1 2 Filley CM, Kleinschmidt-DeMasters BK (August 2001). "Toxic leukoencephalopathy". N. Engl. J. Med. 345 (6): 425–32. doi:10.1056/NEJM200108093450606. PMID 11496854.
- 1 2 3 Buxton JA, Sebastian R, Clearsky L, Angus N, Shah L, Lem M, Spacey SD (2011). "Chasing the dragon - characterizing cases of leukoencephalopathy associated with heroin inhalation in British Columbia". Harm Reduction Journal. 8 (1): 3. doi: 10.1186/1477-7517-8-3 . PMC 3035193 . PMID 21255414.
- 1 2 3 4 5 Iyer, Ramesh; Apeksha Chaturvedi; Sumit Pruthi; Paritosh C. Khanna; Gisele E. Ishak (November 2011). "Medication neurotoxicity in children". Pediatric Radiology. 41 (11): 1455–1464. doi:10.1007/s00247-011-2191-3. PMID 21785849. S2CID 20277034.
- 1 2 3 4 Reddick WE, Glass JO, Helton KJ, Langston JW, Xiong X, Wu S, Pui CH (May 2005). "Prevalence of leukoencephalopathy in children treated for acute lymphoblastic leukemia with high-dose methotrexate". American Journal of Neuroradiology. 26 (5): 1263–1269. PMC 2396789 . PMID 15891195.
- 1 2 3 Offiah, C; E Hall (2008). "Heroin-induced leukoencephalopathy: characterization using MRI, diffusion-weighted imaging, and MR spectroscopy". Clinical Radiology. 63 (2): 146–152. doi:10.1016/j.crad.2007.07.021. PMID 18194689.
- ↑ Salkade, Pareg; Teh Aun Lim (Apr–Jun 2012). "Methotrexate-induced acute toxic leukoencephalopathy". Journal of Cancer Research and Therapeutics. 8 (2): 292–296. doi: 10.4103/0973-1482.98993 . PMID 22842379.
- 1 2 3 4 5 6 7 Sharma P, Eesa M, Scott JN (September 2009). "Toxic and acquired metabolic encephalopathies: MRI appearance". AJR Am J Roentgenol. 193 (3): 879–86. doi:10.2214/AJR.08.2257. PMID 19696305.
- 1 2 Cerase A, Leonini S, Bellini M, Chianese G, Venturi C (July 2011). "Methadone-Induced Toxic Leukoencephalopathy: Diagnosis and Follow-up by Magnetic Resonance Imaging Including Diffusion-Weighted Imaging and Apparent Diffusion Coefficient Maps". Journal of Neuroimaging. 21 (3): 283–286. doi:10.1111/j.1552-6569.2010.00530.x. PMID 20977538. S2CID 1012350.
- 1 2 McKinney, Alexander; Stephen A. Kieffer; Rogerich T. Paylor; Karen S. SantaCruz; Ayse Kendi; Leandro Lucato (July 2009). "Acute Toxic Leukoencephalopathy: Potential for Reversibility Clinically and on MRI With Diffusion-Weighted and FLAIR Imaging". American Journal of Roentgenology. 193 (1): 192–206. doi:10.2214/Ajr.08.1176. PMID 19542414.
- 1 2 González-Suárez I, Aguilar-Amat MJ, Trigueros M, Borobia AM, Cruz A, Arpa J (September 2013). "Leukoencephalopathy due to Oral Methotrexate". Cerebellum. 13 (1): 178–83. doi:10.1007/s12311-013-0528-1. PMID 24068485. S2CID 6854034.
- 1 2 Bathla, G; A.N. Hegde (May 2012). "MRI and CT appearances in metabolic encephalopathies due to systemic diseases in adults". Clinical Radiology. 22. 68 (6): 545–554. doi:10.1016/j.crad.2012.05.021. PMID 23142023.
- ↑ "Heroin-induced toxic leukoencephalopathy". appliedradiology.com. Retrieved 2018-03-07.
- 1 2 Salgado, Rodrigo (November 5, 2009). "Methadone-Induced Toxic Leukoencephalopathy: MR Imaging and MR Proton Spectroscopy Findings". American Journal of Neuroradiology. 31 (3): 565–566. doi: 10.3174/ajnr.A1889 . PMC 7963967 . PMID 19892815.
- ↑ Sacks J, Ray MJ, Williams S, Opatowsky MJ (October 2012). "Fatal toxic leukoencephalopathy secondary to overdose of a new psychoactive designer drug 2C-E ("Europa")". Proc (Bayl Univ Med Cent). 25 (4): 374–6. doi:10.1080/08998280.2012.11928883. PMC 3448584 . PMID 23077393.
- 1 2 Odia, Yazmin Morales; Madhavi Jinka; Wendy C. Ziai (May 2010). "Severe Leukoencephalopathy Following Acute Oxycodone Intoxication". Neurocritical Care Society. 13 (4): 93–97. doi: 10.1007/s12028-010-9373-y . PMID 20440598. S2CID 5995875.
- ↑ Beitinjaneh, Amer; Alexander M. McKinney; Qing Cao; Daniel Weisdorf (March 2011). "Toxic Leukoencephalopathy following Fludarabine-Associated Hematopoietic Cell Transplantation". Biology of Blood and Marrow Transplantation. 17 (3): 300–308. doi: 10.1016/j.bbmt.2010.04.003 . PMID 20399878.
- ↑ Avila, Edward; Paul Schraeder; Ajit Belliappa; Scott Faro (January 2006). "Pica with paradichlorobenzene mothball ingestion associated with toxic leukoencephalopathy". Journal of Neuroimaging. 78-81. 16 (1): 78–81. doi:10.1177/1051228405280171. PMID 16483281. S2CID 10630614.