Related Research Articles

Kikuchi disease was described in 1972 in Japan. It is also known as histiocytic necrotizing lymphadenitis, Kikuchi necrotizing lymphadenitis, phagocytic necrotizing lymphadenitis, subacute necrotizing lymphadenitis, and necrotizing lymphadenitis. Kikuchi disease occurs sporadically in people with no family history of the condition.
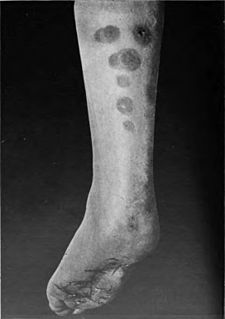
Panniculitis is a group of diseases whose hallmark is inflammation of subcutaneous adipose tissue. Symptoms include tender skin nodules, and systemic signs such as weight loss and fatigue.

Lichen planus (LP) is a chronic inflammatory and immune-mediated disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, and is only named that because it looks like one. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

Lymphadenopathy or adenopathy is a disease of the lymph nodes, in which they are abnormal in size or consistency. Lymphadenopathy of an inflammatory type is lymphadenitis, producing swollen or enlarged lymph nodes. In clinical practice, the distinction between lymphadenopathy and lymphadenitis is rarely made and the words are usually treated as synonymous. Inflammation of the lymphatic vessels is known as lymphangitis. Infectious lymphadenitis affecting lymph nodes in the neck is often called scrofula.

A malar rash, also called butterfly rash, is a medical sign consisting of a characteristic form of facial rash. It is often seen in lupus erythematosus. More rarely, it is also seen in other diseases, such as pellagra, dermatomyositis, and Bloom syndrome.

Mycosis fungoides, also known as Alibert-Bazin syndrome or granuloma fungoides, is the most common form of cutaneous T-cell lymphoma. It generally affects the skin, but may progress internally over time. Symptoms include rash, tumors, skin lesions, and itchy skin.

Livedo reticularis is a common skin finding consisting of a mottled reticulated vascular pattern that appears as a lace-like purplish discoloration of the skin. The discoloration is caused by reduction in blood flow through the arterioles that supply the cutaneous capillaries, resulting in deoxygenated blood showing as blue discoloration. This can be a secondary effect of a condition that increases a person's risk of forming blood clots, including a wide array of pathological and nonpathological conditions. Examples include hyperlipidemia, microvascular hematological or anemia states, nutritional deficiencies, hyper- and autoimmune diseases, and drugs/toxins.

Morphea is a form of scleroderma that involves isolated patches of hardened skin on the face, hands, and feet, or anywhere else on the body, with no internal organ involvement.

Granuloma annulare (GA) is a common, sometimes chronic skin condition which presents as reddish bumps on the skin arranged in a circle or ring. It can initially occur at any age, though two-thirds of patients are under 30 years old, and it is seen most often in children and young adults. Females are two times as likely to have it than males.

Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red painful, inflamed, coin-shaped patches of skin with a scaling and crusty appearance, most often on the scalp, cheeks, and ears. Hair loss may occur if the lesions are on the scalp. The lesions can then develop severe scarring, and the centre areas may appear lighter in color with a rim darker than the normal skin. These lesions can last for years without treatment.

Lupus erythematosus is a collection of autoimmune diseases in which the human immune system becomes hyperactive and attacks healthy tissues. Symptoms of these diseases can affect many different body systems, including joints, skin, kidneys, blood cells, heart, and lungs. The most common and most severe form is systemic lupus erythematosus.
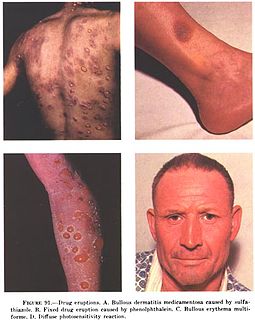
In medicine, a drug eruption is an adverse drug reaction of the skin. Most drug-induced cutaneous reactions are mild and disappear when the offending drug is withdrawn. These are called "simple" drug eruptions. However, more serious drug eruptions may be associated with organ injury such as liver or kidney damage and are categorized as "complex". Drugs can also cause hair and nail changes, affect the mucous membranes, or cause itching without outward skin changes.
Neonatal lupus erythematosus is the occurrence of systemic lupus erythematosus (SLE) symptoms in an infant born from a mother with SLE, most commonly presenting with a rash resembling subacute cutaneous lupus erythematosus, and sometimes with systemic abnormalities such as complete heart block or hepatosplenomegaly.

Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary between people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.

X-linked reticulate pigmentary disorder is a rare X-linked genetic condition in which males manifest multiple systemic symptoms and a reticulated mottled brown pigmentation of the skin, which, on biopsy, demonstrated dermal deposits of amyloid. Females usually only have linear streaks of hyperpigmentation.
Rowell's Syndrome was described by Professor Neville Rowell and colleagues in 1963. Patients with the syndrome have lupus erythematosus, annular lesions of the skin like erythema multiforme associated with a characteristic pattern of immunological abnormalities. It is uncommon but occurs worldwide.
Lupus and pregnancy can present some particular challenges for both mother and child.
Autoimmune optic neuropathy (AON), sometimes called autoimmune optic neuritis, may be a forme fruste of systemic lupus erythematosus (SLE) associated optic neuropathy. AON is more than the presence of any optic neuritis in a patient with an autoimmune process, as it describes a relatively specific clinical syndrome. AON is characterized by chronically progressive or recurrent vision loss associated with serological evidence of autoimmunity. Specifically, this term has been suggested for cases of optic neuritis with serological evidence of vasculitis by positive ANA, despite the lack of meeting criteria for SLE. The clinical manifestations include progressive vision loss that tends to be steroid-responsive and steroid dependent.
Cutaneous manifestations of COVID-19 are characteristic signs or symptoms of the Coronavirus disease 2019 that occur in the skin. The American Academy of Dermatology reports that skin lesions such as morbilliform, pernio, urticaria, macular erythema, vesicular purpura, papulosquamous purpura and retiform purpura are seen in people with COVID-19. Pernio-like lesions were more common in mild disease while retiform purpura was seen only in critically ill patients. The major dermatologic patterns identified in individuals with COVID-19 are urticarial rash, confluent erythematous/morbilliform rash, papulovesicular exanthem, chilbain-like acral pattern, livedo reticularis and purpuric “vasculitic” pattern. Chilblains and Multisystem inflammatory syndrome in children are also cutaneous manifestations of COVID-19.
References
- ↑ Rapini RP, Bolognia JL, Jorizzo JL (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- 1 2 Werth VP (June 2005). "Clinical manifestations of cutaneous lupus erythematosus". Autoimmunity Reviews. 4 (5): 296–302. doi:10.1016/j.autrev.2005.01.003. PMID 15990077.
- ↑ McCauliffe DP (March 2001). "Cutaneous lupus erythematosus". Seminars in Cutaneous Medicine and Surgery. 20 (1): 14–26. doi:10.1053/sder.2001.23091. PMID 11308132.
- 1 2 3 4 Okon LG, Werth VP (June 2013). "Cutaneous lupus erythematosus: diagnosis and treatment". Best Practice & Research. Clinical Rheumatology. Systemic Lupus Erythematosus. 27 (3): 391–404. doi:10.1016/j.berh.2013.07.008. PMC 3927537 . PMID 24238695.