Tests
| | This section is empty. You can help by adding to it. (July 2024) |
Aldosterone-to-renin ratio (ARR) is the mass concentration of aldosterone divided by the plasma renin activity or by serum renin concentration in blood. The aldosterone/renin ratio is recommended as screening tool for primary hyperaldosteronism. [1]
| | This section is empty. You can help by adding to it. (July 2024) |
The cutoff normal individuals from those with primary hyperaldosteronism is significantly affected by the conditions of testing, such as posture and time of day. On average, an ARR cutoff of 23.6 ng/dL per ng/(mL·h), expressed in alternative units as 651 pmol/L per μg/(L·h), has been estimated to have a sensitivity of 97% and specificity of 94%. [2] An ARR value in an individual that is higher than the cutoff indicates primary hyperaldosteronism.
If the inverse ratio (i.e. renin-to-aldosterone) ratio is used, a value lower than the cutoff indicates primary hyperaldosteronism.
| Aldosterone-to-renin ratio | Renin-to-aldosterone ratio | |||
|---|---|---|---|---|
| Value | Unit | Value | Unit | |
| 13.1, [1] 23.6, [2] 35.0 [1] | ng/dL per ng/(mL·h) | 0.029, 0.042, 0.076 | ng/(mL·h) per ng/dL | |
| 362, 651, 966 | pmol/L per μg/(L·h) | 0.0010, 0.0015, 0.0028 | μg/(L·h) per pmol/L | |
Reference ranges for blood tests are sets of values used by a health professional to interpret a set of medical test results from blood samples. Reference ranges for blood tests are studied within the field of clinical chemistry, the area of pathology that is generally concerned with analysis of bodily fluids.

Renin, also known as an angiotensinogenase, is an aspartic protease protein and enzyme secreted by the kidneys that participates in the body's renin–angiotensin–aldosterone system (RAAS)—also known as the renin–angiotensin–aldosterone axis—that increases the volume of extracellular fluid and causes arterial vasoconstriction. Thus, it increases the body's mean arterial blood pressure.
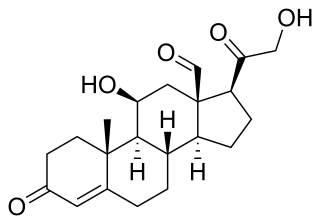
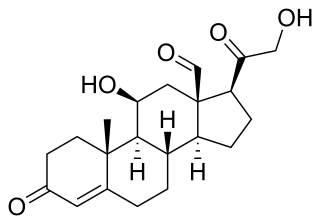
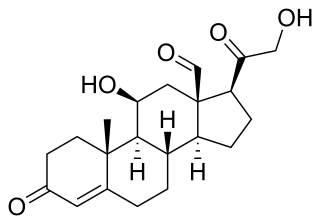
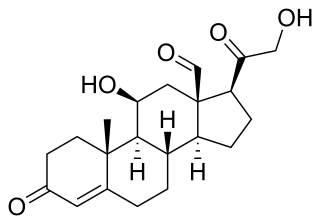
Aldosterone is the main mineralocorticoid steroid hormone produced by the zona glomerulosa of the adrenal cortex in the adrenal gland. It is essential for sodium conservation in the kidney, salivary glands, sweat glands, and colon. It plays a central role in the homeostatic regulation of blood pressure, plasma sodium (Na+), and potassium (K+) levels. It does so primarily by acting on the mineralocorticoid receptors in the distal tubules and collecting ducts of the nephron. It influences the reabsorption of sodium and excretion of potassium (from and into the tubular fluids, respectively) of the kidney, thereby indirectly influencing water retention or loss, blood pressure, and blood volume. When dysregulated, aldosterone is pathogenic and contributes to the development and progression of cardiovascular and kidney disease. Aldosterone has exactly the opposite function of the atrial natriuretic hormone secreted by the heart.
Primary aldosteronism (PA), also known as primary hyperaldosteronism, refers to the excess production of the hormone aldosterone from the adrenal glands, resulting in low renin levels and high blood pressure. This abnormality is caused by hyperplasia or tumors. About 35% of the cases are caused by a single aldosterone-secreting adenoma, a condition known as Conn's syndrome.
Hypoaldosteronism is an endocrinological disorder characterized by decreased levels of the hormone aldosterone. Similarly, isolated hypoaldosteronism is the condition of having lowered aldosterone without corresponding changes in cortisol.

The zona glomerulosa of the adrenal gland is the most superficial layer of the adrenal cortex, lying directly beneath the renal capsule. Its cells are ovoid and arranged in clusters or arches.

Metabolic alkalosis is a metabolic condition in which the pH of tissue is elevated beyond the normal range (7.35–7.45). This is the result of decreased hydrogen ion concentration, leading to increased bicarbonate, or alternatively a direct result of increased bicarbonate concentrations. The condition typically cannot last long if the kidneys are functioning properly.
Hyperaldosteronism is a medical condition wherein too much aldosterone is produced. High aldosterone levels can lead to lowered levels of potassium in the blood (hypokalemia) and increased hydrogen ion excretion (alkalosis). Aldosterone is normally produced in the adrenal glands.

Apparent mineralocorticoid excess is an autosomal recessive disorder causing hypertension, hypernatremia and hypokalemia. It results from mutations in the HSD11B2 gene, which encodes the kidney isozyme of 11β-hydroxysteroid dehydrogenase type 2. In an unaffected individual, this isozyme inactivates circulating cortisol to the less active metabolite cortisone. The inactivating mutation leads to elevated local concentrations of cortisol in the aldosterone sensitive tissues like the kidney. Cortisol at high concentrations can cross-react and activate the mineralocorticoid receptor due to the non-selectivity of the receptor, leading to aldosterone-like effects in the kidney. This is what causes the hypokalemia, hypertension, and hypernatremia associated with the syndrome. Patients often present with severe hypertension and end-organ changes associated with it like left ventricular hypertrophy, retinal, renal and neurological vascular changes along with growth retardation and failure to thrive. In serum both aldosterone and renin levels are low.

Liddle's syndrome, also called Liddle syndrome, is a genetic disorder inherited in an autosomal dominant manner that is characterized by early, and frequently severe, high blood pressure associated with low plasma renin activity, metabolic alkalosis, low blood potassium, and normal to low levels of aldosterone. Liddle syndrome involves abnormal kidney function, with excess reabsorption of sodium and loss of potassium from the renal tubule, and is treated with a combination of low sodium diet and potassium-sparing diuretics. It is extremely rare, with fewer than 30 pedigrees or isolated cases having been reported worldwide as of 2008.
Pseudohyperaldosteronism is a medical condition which mimics the effects of elevated aldosterone (hyperaldosteronism) by presenting with high blood pressure, low blood potassium levels (hypokalemia), metabolic alkalosis, and low levels of plasma renin activity (PRA). However, unlike hyperaldosteronism, this conditions exhibits low or normal levels of aldosterone in the blood. Causes include genetic disorders, acquired conditions, metabolic disorders, and dietary imbalances including excessive consumption of licorice. Confirmatory diagnosis depends on the specific cause and may involve blood tests, urine tests, or genetic testing; however, all forms of this condition exhibit abnormally low concentrations of both plasma renin activity (PRA) and plasma aldosterone concentration (PAC) which differentiates this group of conditions from other forms of secondary hypertension. Treatment is tailored to the specific cause and focuses on symptom control, blood pressure management, and avoidance of triggers.

Aldosterone synthase, also called steroid 18-hydroxylase, corticosterone 18-monooxygenase or P450C18, is a steroid hydroxylase cytochrome P450 enzyme involved in the biosynthesis of the mineralocorticoid aldosterone and other steroids. The enzyme catalyzes sequential hydroxylations of the steroid angular methyl group at C18 after initial 11β-hydroxylation. It is encoded by the CYP11B2 gene in humans.
The ACTH test is a medical test usually requested and interpreted by endocrinologists to assess the functioning of the adrenal glands' stress response by measuring the adrenal response to adrenocorticotropic hormone or another corticotropic agent such as tetracosactide or alsactide (Synchrodyn). ACTH is a hormone produced in the anterior pituitary gland that stimulates the adrenal glands to release cortisol, dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (DHEA-S), and aldosterone.

Renin inhibitors are pharmaceutical drugs inhibiting the activity of renin that is responsible for hydrolyzing angiotensinogen to angiotensin I, which in turn reduces the formation of angiotensin II that facilitates blood pressure.
Plasma renin activity (PRA), also known as the renin (active) assay or random plasma renin, is a measure of the activity of the plasma enzyme renin, which plays a major role in the body's regulation of blood pressure, thirst, and urine output. Measure of direct renin concentration (DRC) is technically more demanding, and hence PRA is used instead. DRC assays are still in evolution, and generally a conversion factor of PRA (ng/mL/h) to DRC (mU/L) is 8.2. A recently developed and already commonly used automated DRC assay uses the conversion factor of 12. PRA is sometimes measured, specially in case of certain diseases which present with hypertension or hypotension. PRA is also raised in certain tumors. A PRA measurement may be compared to a plasma aldosterone concentration as an aldosterone-to-renin ratio (ARR).
Glucocorticoid remediable aldosteronism also describable as aldosterone synthase hyperactivity, is an autosomal dominant disorder in which the increase in aldosterone secretion produced by ACTH is no longer transient.

Pathophysiology is a study which explains the function of the body as it relates to diseases and conditions. The pathophysiology of hypertension is an area which attempts to explain mechanistically the causes of hypertension, which is a chronic disease characterized by elevation of blood pressure. Hypertension can be classified by cause as either essential or secondary. About 90–95% of hypertension is essential hypertension. Some authorities define essential hypertension as that which has no known explanation, while others define its cause as being due to overconsumption of sodium and underconsumption of potassium. Secondary hypertension indicates that the hypertension is a result of a specific underlying condition with a well-known mechanism, such as chronic kidney disease, narrowing of the aorta or kidney arteries, or endocrine disorders such as excess aldosterone, cortisol, or catecholamines. Persistent hypertension is a major risk factor for hypertensive heart disease, coronary artery disease, stroke, aortic aneurysm, peripheral artery disease, and chronic kidney disease.
Feline hyperaldosteronism is a disease in cats. The symptoms are caused by abnormally high concentrations of the hormone aldosterone, which is secreted by the adrenal gland. The high concentrations of aldosterone may be due directly to a disorder of the adrenal gland, or due to something outside of the adrenal gland causing it to secrete excessive aldosterone.

11β-Hydroxyprogesterone (11β-OHP), also known as 21-deoxycorticosterone, as well as 11β-hydroxypregn-4-ene-3,20-dione, is a naturally occurring, endogenous steroid and derivative of progesterone. It is a potent mineralocorticoid. Syntheses of 11β-OHP from progesterone is catalyzed by the steroid 11β-hydroxylase (CYP11B1) enzyme, and, to a lesser extent, by the aldosterone synthase enzyme (CYP11B2).
SUSPUP (serum sodium to urinary sodium to serum potassium to urinary potassium) and SUSPPUP (serum sodium to urinary sodium to (serum potassium)2 to urinary potassium) are calculated structure parameters of the renin–angiotensin-aldosterone system (RAAS). They have been developed to support screening for primary or secondary aldosteronism.