Related Research Articles

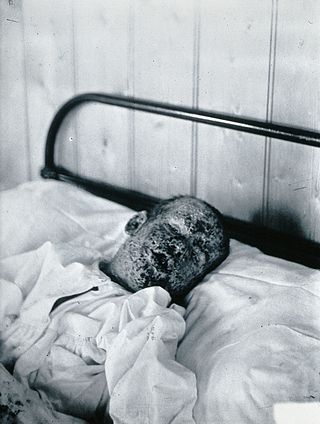
Malaria is a mosquito-borne infectious disease that affects vertebrates. Human malaria causes symptoms that typically include fever, fatigue, vomiting, and headaches. In severe cases, it can cause jaundice, seizures, coma, or death. Symptoms usually begin 10 to 15 days after being bitten by an infected Anopheles mosquito. If not properly treated, people may have recurrences of the disease months later. In those who have recently survived an infection, reinfection usually causes milder symptoms. This partial resistance disappears over months to years if the person has no continuing exposure to malaria.

Mefloquine, sold under the brand name Lariam among others, is a medication used to prevent or treat malaria. When used for prevention it is typically started before potential exposure and continued for several weeks after potential exposure. It can be used to treat mild or moderate malaria but is not recommended for severe malaria. It is taken by mouth.
Antimalarial medications or simply antimalarials are a type of antiparasitic chemical agent, often naturally derived, that can be used to treat or to prevent malaria, in the latter case, most often aiming at two susceptible target groups, young children and pregnant women. As of 2018, modern treatments, including for severe malaria, continued to depend on therapies deriving historically from quinine and artesunate, both parenteral (injectable) drugs, expanding from there into the many classes of available modern drugs. Incidence and distribution of the disease is expected to remain high, globally, for many years to come; moreover, known antimalarial drugs have repeatedly been observed to elicit resistance in the malaria parasite—including for combination therapies featuring artemisinin, a drug of last resort, where resistance has now been observed in Southeast Asia. As such, the needs for new antimalarial agents and new strategies of treatment remain important priorities in tropical medicine. As well, despite very positive outcomes from many modern treatments, serious side effects can impact some individuals taking standard doses.

The Pan American Health Organization (PAHO) is a specialized agency of the United Nations (UN) in charge of international health cooperation in the Americas. It fosters technical cooperation among member countries to fight communicable and noncommunicable diseases, strengthen health systems, and respond to emergencies and disasters.

Artesunate (AS) is a medication used to treat malaria. The intravenous form is preferred to quinine for severe malaria. Often it is used as part of combination therapy, such as artesunate plus mefloquine. It is not used for the prevention of malaria. Artesunate can be given by injection into a vein, injection into a muscle, by mouth, and by rectum.

The Drugs for Neglected Diseases initiative (DNDi) is a collaborative, patients' needs-driven, non-profit drug research and development (R&D) organization that is developing new treatments for neglected diseases, notably leishmaniasis, sleeping sickness, Chagas disease, malaria, filarial diseases, mycetoma, paediatric HIV, cryptococcal meningitis, hepatitis C, and dengue. DNDi's malaria activities were transferred to Medicines for Malaria Venture (MMV) in 2015.
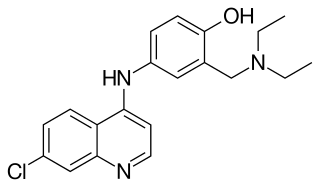
Amodiaquine (ADQ) is a medication used to treat malaria, including Plasmodium falciparum malaria when uncomplicated. It is recommended to be given with artesunate to reduce the risk of resistance. Due to the risk of rare but serious side effects, it is not generally recommended to prevent malaria. Though, the World Health Organization (WHO) in 2013 recommended use for seasonal preventive in children at high risk in combination with sulfadoxine and pyrimethamine.
The eradication of infectious diseases is the reduction of the prevalence of an infectious disease in the global host population to zero.

The United States established diplomatic relations with Malawi in 1964 after Malawi gained independence from the United Kingdom. Malawi's transition from a one-party state to a multi-party democracy significantly strengthened the already cordial U.S. relationship with Malawi. Significant numbers of Malawians study in the United States. The United States has an active Peace Corps program, Centers for Disease Control and Prevention, Department of Health and Human Services, and an Agency for International Development (USAID) mission in Malawi. Both countries have a common history and English language, as they were part of the British Empire.

A landlocked sub-Saharan country, Burkina Faso is among the poorest countries in the world—44 percent of its population lives below the international poverty line of US$1.90 per day —and it ranks 185th out of 188 countries on UNDP's 2016 Human Development Index. Rapid population growth, gender inequality, and low levels of educational attainment contribute to food insecurity and poverty in Burkina Faso. The total population is just over 20 million with the estimated population growth rate is 3.1 percent per year and seven out of 10 Burkinabe are younger than 30. Total health care expenditures were an estimated 5% of GDP. Total expenditure on health per capita is 82 in 2014.
Intermittent preventive therapy or intermittent preventive treatment (IPT) is a public health intervention aimed at treating and preventing malaria episodes in infants (IPTi), children (IPTc), schoolchildren (IPTsc) and pregnant women (IPTp). The intervention builds on two tested malaria control strategies to clear existing parasites and to prevent new infections (prophylaxis).
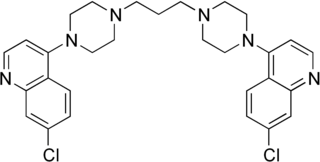
Piperaquine is an antiparasitic drug used in combination with dihydroartemisinin to treat malaria. Piperaquine was developed under the Chinese National Malaria Elimination Programme in the 1960s and was adopted throughout China as a replacement for the structurally similar antimalarial drug chloroquine. Due to widespread parasite resistance to piperaquine, the drug fell out of use as a monotherapy, and is instead used as a partner drug for artemisinin combination therapy. Piperaquine kills parasites by disrupting the detoxification of host heme.
Project 523 is a code name for a 1967 secret military project of the People's Republic of China to find antimalarial medications. Named after the date the project launched, 23 May, it addressed malaria, an important threat in the Vietnam War. At the behest of Ho Chi Minh, Prime Minister of North Vietnam, Zhou Enlai, the Premier of the People's Republic of China, convinced Mao Zedong, Chairman of the Chinese Communist Party, to start the mass project "to keep [the] allies' troops combat-ready", as the meeting minutes put it. More than 500 Chinese scientists were recruited. The project was divided into three streams. The one for investigating traditional Chinese medicine discovered and led to the development of a class of new antimalarial drugs called artemisinins. Launched during and lasting throughout the Cultural Revolution, Project 523 was officially terminated in 1981.
Naval Medical Research Unit SOUTH, formerly known as Naval Medical Research Unit Six, is a biomedical research laboratory of the U.S. Navy located in Lima, Peru. It is the only U.S. military command located in South America. Its mission is to identify infectious disease threats of military and public health importance and to develop and evaluate interventions and products to mitigate those threats.
The Affordable Medicines Facility-malaria (AMFm) is a financing mechanism intended to expand access to affordable and effective antimalarial medication. It works primarily through the commercial private sector, in addition to the public and non-governmental organization sectors which are the more traditional routes for development assistance in malaria control. Its goal is to drive down the price of the most effective malaria medicines so that millions of people can afford to buy them. The program has been called "one of the most important recent advances in fighting malaria" and "a triumph of international cooperation." The AMFm is hosted and managed by the Global Fund to Fight AIDS, Tuberculosis and Malaria in Geneva, Switzerland.
The Johns Hopkins Center for Communication Programs (CCP) was founded over 30 years ago by Phyllis Tilson Piotrow as a part the Johns Hopkins Bloomberg School of Public Health's department of Health, Behavior, and Society and is located in Baltimore, Maryland, United States.

Healthcare in Belize is provided through both public and private healthcare systems. The Ministry of Health (MoH) is the government agency responsible for overseeing the entire health sector and is also the largest provider of public health services in Belize. The MoH offers affordable care to a majority of Belizeans with a strong focus on providing quality healthcare through a range of public programs and institutions.
Malaria Day in the Americas is commemorated annually on November 6 to promote awareness, recognize past and current efforts to prevent and control malaria in the region of the Americas, build commitment, and to mobilize action to advance malaria goals and targets as the region works towards elimination. Awareness of this disease is very important in the region of the Americas, where an estimated 120 million people in 21 endemic countries are at risk of malaria. In 2012, there were 469,000 confirmed malaria cases in the region with 108 deaths. Nonetheless, declining incidence of disease and malaria-related mortality has led to low prioritization of malaria on national health agendas in the Americas.
Asia Pacific Leaders Malaria Alliance (APLMA) is an affiliation of Asian and Pacific heads of government formed to accelerate progress against malaria, aiming to eliminate the disease in the Asia Pacific Region by 2030 and reduce risk from other communicable diseases.
References
- 1 2 Najera, Jose; Zimmerman, Robert; Schmunis, Gabriel (April 23, 2012). External Evaluation of the AMI and RAVREDA.
- 1 2 3 Pribluda, Victor S; Barojas, Adrian; Añez, Arletta; López, Cecilia G; Figueroa, Ruth; Herrera, Roxana; Nakao, Gladys; Nogueira, Fernando HA; Pianetti, Gerson A; Povoa, Marinete M; Viana, Giselle MR; Gomes, Margarete S; Escobar, Jose P; Sierra, Olga L; Norena, Susana P; Veloz, Raúl; Bravo, Marcy; Aldás, Martha R; HindsSemple, Alison; Collins, Marilyn; Ceron, Nicolas; Krishnalall, Karanchand; Adhin, Malti; Bretas, Gustavo; Hernandez, Nelly; Mendoza, Marjorie; Smine, Abdelkrim; Chibwe, Kennedy; Lukulay, Patrick; Evans, Lawrence (2012). "Implementation of basic quality control tests for malaria medicines in Amazon Basin countries: results for the 2005–2010 period". Malaria Journal. 11 (1): 2–11. doi: 10.1186/1475-2875-11-202 . PMC 3433375 . PMID 22704680.
- ↑ "AMI Goal and Accomplishments" (PDF). usaidami. Archived from the original (PDF) on 2014-07-14. Retrieved 2014-06-09.
- 1 2 3 Cibulskis, Roll Back Malaria Partnership; [co-authored by Richard; Szilagyi], Zsofia (2012). Defeating malaria in Asia, the Pacific, Americas, Middle East and Europe. Geneva, Switzerland: World Health Organization on behalf of the Roll Back Maleria Secretariat. pp. 65–66. ISBN 9789241504430.
{{cite book}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 "AMI Brochure 2014" (PDF). linksmedia.net.
- ↑ Hiwat, Hélène; Hardjopawiro, Loretta S; Takken, Willem; Villegas, Leopoldo (2012). "Novel strategies lead to pre-elimination of malaria in previously high-risk areas in Suriname, South America". Malaria Journal. 11 (1): 1–4. doi: 10.1186/1475-2875-11-10 . PMC 3281795 . PMID 22230221.
- 1 2 3 "Activities in the Amazon Region". www.cdc.com. Retrieved 26 June 2014.
- 1 2 World Health Organisation (October 2011). "Plan to reduce Malaria and Prevent its Reintroduction" (Press Release). scoop. Retrieved 19 June 2014.
- ↑ Regional strategic plan for malaria in the Americas 2006-2010 (PDF). Washington, DC: Pan American Health Organization, Regional office of the World Health Organization. 2006. p. 23. ISBN 9275126410.
- 1 2 3 4 5 6 7 "Malaria in the Americas". paho.org. Retrieved 26 June 2014.
- ↑ "Combating Malaria" (PDF). NAPSA.
- ↑ Minsa (November 7, 2008). "Casos de Malaria mortal se redujeron". Andina. Archived from the original on August 31, 2014. Retrieved 19 June 2014.
- ↑ "Caribbean and the Americas at risk of disease carried by small insects". What'supCaribbean. Archived from the original on 2014-08-31. Retrieved 18 July 2014.
- ↑ Kumar, kaveri; Pigazzini, Anna; Stenson, Bo. "Financing for Malaria Elimination" (PDF). globalhealthscience.ucsf.edu. Archived from the original (PDF) on 2014-10-24. Retrieved 2014-06-19.
- 1 2 3 4 World Malaria Report (PDF). Geneva: WHO Library. 2011. p. 60. ISBN 978-92-4-156440-3 . Retrieved 7 July 2014.