Related Research Articles

A picture archiving and communication system (PACS) is a medical imaging technology which provides economical storage and convenient access to images from multiple modalities. Electronic images and reports are transmitted digitally via PACS; this eliminates the need to manually file, retrieve, or transport film jackets, the folders used to store and protect X-ray film. The universal format for PACS image storage and transfer is DICOM. Non-image data, such as scanned documents, may be incorporated using consumer industry standard formats like PDF, once encapsulated in DICOM. A PACS consists of four major components: The imaging modalities such as X-ray plain film (PF), computed tomography (CT) and magnetic resonance imaging (MRI), a secured network for the transmission of patient information, workstations for interpreting and reviewing images, and archives for the storage and retrieval of images and reports. Combined with available and emerging web technology, PACS has the ability to deliver timely and efficient access to images, interpretations, and related data. PACS reduces the physical and time barriers associated with traditional film-based image retrieval, distribution, and display.

Radiology is the medical discipline that uses medical imaging to diagnose diseases and guide their treatment, within the bodies of humans and other animals. It began with radiography, but today it includes all imaging modalities, including those that use no electromagnetic radiation, as well as others that do, such as computed tomography (CT), fluoroscopy, and nuclear medicine including positron emission tomography (PET). Interventional radiology is the performance of usually minimally invasive medical procedures with the guidance of imaging technologies such as those mentioned above.
Medical physics deals with the application of the concepts and methods of physics to the prevention, diagnosis and treatment of human diseases with a specific goal of improving human health and well-being. Since 2008, medical physics has been included as a health profession according to International Standard Classification of Occupation of the International Labour Organization.

Mammography is the process of using low-energy X-rays to examine the human breast for diagnosis and screening. The goal of mammography is the early detection of breast cancer, typically through detection of characteristic masses or microcalcifications.
A radiation oncologist is a specialist physician who uses ionizing radiation in the treatment of cancer. Radiation oncology is one of the three primary specialties, the other two being surgical and medical oncology, involved in the treatment of cancer. Radiation can be given as a curative modality, either alone or in combination with surgery and/or chemotherapy. It may also be used palliatively, to relieve symptoms in patients with incurable cancers. A radiation oncologist may also use radiation to treat some benign diseases, including benign tumors. In some countries, radiotherapy and chemotherapy are controlled by a single oncologist who is a "clinical oncologist". Radiation oncologists work closely with other physicians such as surgical oncologists, interventional radiologists, internal medicine subspecialists, and medical oncologists, as well as medical physicists and technicians as part of the multi-disciplinary cancer team. Radiation oncologists undergo four years of oncology-specific training whereas oncologists who deliver chemotherapy have two years of additional training in cancer care during fellowship after internal medicine residency in the United States.
Computed tomography laser mammography (CTLM) is the trademark of Imaging Diagnostic Systems, Inc. for its optical tomographic technique for female breast imaging.

Radiographers, also known as radiologic technologists, diagnostic radiographers and medical radiation technologists are healthcare professionals who specialise in the imaging of human anatomy for the diagnosis and treatment of pathology. Radiographers are infrequently, and almost always erroneously, known as x-ray technicians. In countries that use the title radiologic technologist they are often informally referred to as techs in the clinical environment; this phrase has emerged in popular culture such as television programmes. The term radiographer can also refer to a therapeutic radiographer, also known as a radiation therapist.
BI-RADS is an acronym for Breast Imaging-Reporting and Data System, a quality assurance tool originally designed for use with mammography. The system is a collaborative effort of many health groups but is published and trademarked by the American College of Radiology (ACR).

Molecular breast imaging (MBI), also known as scintimammography, is a type of breast imaging test that is used to detect cancer cells in breast tissue of individuals who have had abnormal mammograms, especially for those who have dense breast tissue, post-operative scar tissue or breast implants.
Physician self-referral is a term describing the practice of a physician ordering tests on a patient that are performed by either the referring physician himself or a fellow faculty member from whom he receives financial compensation in return for the referral. Examples of self-referral include an internist performing an EKG, a surgeon suggesting an operation that he himself would perform, and a physician ordering imaging tests that would be done at a facility he owns or leases.
Nuclear medicine physicians, also called nuclear radiologists or simply nucleologists, are medical specialists that use tracers, usually radiopharmaceuticals, for diagnosis and therapy. Nuclear medicine procedures are the major clinical applications of molecular imaging and molecular therapy. In the United States, nuclear medicine physicians are certified by the American Board of Nuclear Medicine and the American Osteopathic Board of Nuclear Medicine.

Lexington Medical Center is a medical complex in Lexington, SC. Lexington Medical Center is owned by Lexington County Health Service District, Inc, a private company. The network includes six community medical centers, an occupational health facility, the largest nursing home in the Carolinas, an Alzheimer's disease care center and seventy physician practices in a variety of services.
Radiation Exposure Monitoring (REM) is a framework developed by Integrating the Healthcare Enterprise (IHE), for utilizing existing technical standards, such as DICOM, to provide information about the dose delivered to patients in radiology procedures, in an interoperable format.
Dynamic angiothermography (DATG) is a technique for the diagnosis of breast cancer. This technique, though springing from the thermography of old conception, is based on a completely different principle. DATG records the temperature variations linked to the vascular changes in the breast due to angiogenesis. The presence, change, and growth of tumors and lesions in breast tissue change the vascular network in the breast. Consequently, measuring the vascular structure over time, DATG effectively monitors the change in breast tissue due to tumors and lesions. It is currently used in combination with other techniques for diagnosis of breast cancer. This diagnostic method is a low cost one compared with other techniques.

Ronald J. Ross is a Cleveland, Ohio radiologist known for research on brain injury in professional and amateur boxers and for the first clinical use of nuclear magnetic resonance imaging on human patients. Ross is also credited with the first use of head and whole body computed tomography imaging (CT) in a private clinical setting in the United States.
Global radiology, a subspecialty of diagnostic radiology, comprises the study and practice of improving access to radiology resources in poor and developing countries, and addressing global health inequities through the application of radiology. Similar to the fields of public health and global health, global radiology draws on and encourages collaboration with nonmedical specialties relevant to disease patterns and the provision of medical services, including economic development, biomedical technology, engineering and social sciences.
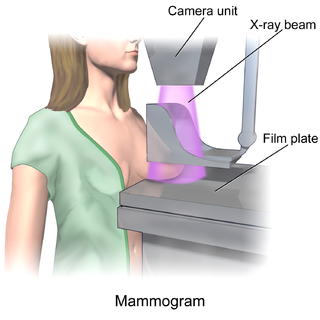
In medicine, breast imaging is a sub-speciality of diagnostic radiology that involves imaging of the breasts for screening or diagnostic purposes. There are various methods of breast imaging using a variety of technologies as described in detail below. Traditional screening and diagnostic mammography uses x-ray technology and has been the mainstay of breast imaging for many decades. Breast tomosynthesis is a relatively new digital x-ray mammography technique that produces multiple image slices of the breast similar to, but distinct from, computed tomography (CT). Xeromammography and galactography are somewhat outdated technologies that also use x-ray technology and are now used infrequently in the detection of breast cancer. Breast ultrasound is another technology employed in diagnosis and screening that can help differentiate between fluid filled and solid lesions, an important factor to determine if a lesion may be cancerous. Breast MRI is a technology typically reserved for high-risk patients and patients recently diagnosed with breast cancer. Lastly, scintimammography is used in a subgroup of patients who have abnormal mammograms or whose screening is not reliable on the basis of using traditional mammography or ultrasound.
Jill Wruble is a radiologist and fellow at Johns Hopkins Medicine who is best known as a speaker on overdiagnosis due to incidental imaging finding in United States medicine.
HB 2102, also known as "Henda's Law", is a breast density (BD) notification law approved in 2011 by the FDA that mammography patients be provided educational materials on dense breast tissue can hide abnormalities, including breast cancer, from traditional screening. Henda's Law aims to promote patient doctor discussion as well as reduce the rate of false negatives, as mammography may not detect abnormalities in dense breasts.
Dense breast tissue, also known as dense breasts, is a condition of the breasts where a higher proportion of the breasts are made up of glandular tissue and fibrous tissue than fatty tissue. Around 40–50% of women have dense breast tissue and one of the main medical components of the condition is that mammograms are unable to differentiate tumorous tissue from the surrounding dense tissue. This increases the risk of late diagnosis of breast cancer in women with dense breast tissue. Additionally, women with such tissue have a higher likelihood of developing breast cancer in general, though the reasons for this are poorly understood.
References
- ↑ "ACR Chapters". www.acr.org. Retrieved 2018-06-14.
- ↑ "Accredited Facility Search". www.acraccreditation.org.
- ↑ "ACR Education Center in Reston – the World's Best Practice Simulator | American College of Radiology". www.acr.org. Retrieved 2019-07-01.
- ↑ "Home". www.airp.org.
- ↑ "Radiology Leadership Institute". www.acr.org. Retrieved 2019-07-01.
- ↑ "Journal of the American College of Radiology Home Page". www.jacr.org. Retrieved 2019-07-01.
- ↑ "RadiologyInfo.org". www.radiologyinfo.org. Retrieved 2018-06-14.
- ↑ "Resources". www.acr.org.