Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver.
An endoscope is an inspection instrument composed of image sensor, optical lens, light source and mechanical device, which is used to look deep into the body by way of openings such as the mouth or anus. A typical endoscope applies several modern technologies including optics, ergonomics, precision mechanics, electronics, and software engineering. With an endoscope, it is possible to observe lesions that cannot be detected by X-ray, making it useful in medical diagnosis. Endoscopes use tubes which are only a few millimeters thick to transfer illumination in one direction and high-resolution images in real time in the other direction, resulting in minimally invasive surgeries. It is used to examine the internal organs like the throat or esophagus. Specialized instruments are named after their target organ. Examples include the cystoscope (bladder), nephroscope (kidney), bronchoscope (bronchus), arthroscope (joints) and colonoscope (colon), and laparoscope. They can be used to examine visually and diagnose, or assist in surgery such as an arthroscopy.

Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. It is primarily performed by highly skilled and specialty trained gastroenterologists. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject a contrast medium into the ducts in the biliary tree and pancreas so they can be seen on radiographs.
A low-residue diet is a diet intended to reduce certain constituents of the bowel, often with consequence for functional behaviour of the bowel. It may be prescribed for patients with ailments or functional gastrointestinal disorders mitigated by fewer and smaller bowel movements each day.
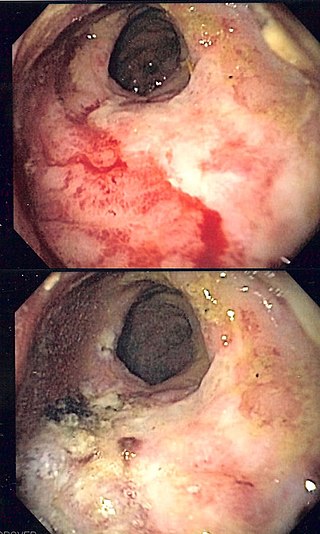
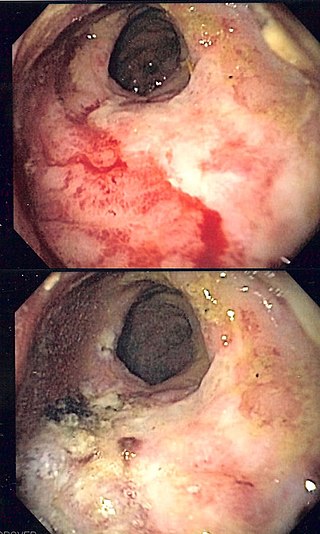
Radiation proctitis or radiation proctopathy is a condition characterized by damage to the rectum after exposure to x-rays or other ionizing radiation as a part of radiation therapy. Radiation proctopathy may occur as acute inflammation called "acute radiation proctitis" or with chronic changes characterized by radiation associated vascular ectasiae (RAVE) and chronic radiation proctopathy. Radiation proctitis most commonly occurs after pelvic radiation treatment for cancers such as cervical cancer, prostate cancer, bladder cancer, and rectal cancer. RAVE and chronic radiation proctopathy involves the lower intestine, primarily the sigmoid colon and the rectum, and was previously called chronic radiation proctitis, pelvic radiation disease and radiation enteropathy.

Bisacodyl (INN) is an organic compound that is used as a stimulant laxative drug. It works directly on the colon to produce a bowel movement. It is typically prescribed for relief of episodic and chronic constipation and for the management of neurogenic bowel dysfunction, as well as part of bowel preparation before medical examinations, such as for a colonoscopy.

Double-balloon enteroscopy, also known as push-and-pull enteroscopy, is an endoscopic technique for visualization of the small bowel. It was developed by Hironori Yamamoto in 2001. It is novel in the field of diagnostic gastroenterology as it is the first endoscopic technique that allows for the entire gastrointestinal tract to be visualized in real time.
Stretta is a minimally invasive endoscopic procedure for the treatment of gastroesophageal reflux disease (GERD) that delivers radiofrequency energy in the form of electromagnetic waves through electrodes at the end of a catheter to the lower esophageal sphincter (LES) and the gastric cardia – the region of the stomach just below the LES. The energy heats the tissue, ultimately causing it to swell and stiffen; the way this works was not understood as of 2015, but it was thought that perhaps the heat causes local inflammation, collagen deposition and muscular thickening of the LES and that it may disrupt the nerves there.

An endoclip is a metallic mechanical device used in endoscopy in order to close two mucosal surfaces without the need for surgery and suturing. Its function is similar to a suture in gross surgical applications, as it is used to join together two disjointed surfaces, but, can be applied through the channel of an endoscope under direct visualization. Endoclips have found use in treating gastrointestinal bleeding, in preventing bleeding after therapeutic procedures such as polypectomy, and in closing gastrointestinal perforations. Many forms of endoclips exist of different shapes and sizes, including two and three prong devices, which can be administered using single use and reloadable systems, and may or may not open and close to facilitate placement.

Capsule endoscopy is a medical procedure used to record internal images of the gastrointestinal tract for use in disease diagnosis. Newer developments are also able to take biopsies and release medication at specific locations of the entire gastrointestinal tract. Unlike the more widely used endoscope, capsule endoscopy provides the ability to see the middle portion of the small intestine. It can be applied to the detection of various gastrointestinal cancers, digestive diseases, ulcers, unexplained bleedings, and general abdominal pains. After a patient swallows the capsule, it passes along the gastrointestinal tract, taking a number of images per second which are transmitted wirelessly to an array of receivers connected to a portable recording device carried by the patient. General advantages of capsule endoscopy over standard endoscopy include the minimally invasive procedure setup, ability to visualize more of the gastrointestinal tract, and lower cost of the procedure.

An endoscopy unit refers to a dedicated area where medical procedures are performed with endoscopes, which are cameras used to visualize structures within the body, such as the digestive tract and genitourinary system. Endoscopy units may be located within a hospital, incorporated within other medical care centres, or may be stand-alone in nature.
Blair S. Lewis, M.D., F.A.C.P., F.A.C.G., is an American board-certified gastroenterologist and Clinical Professor of Medicine at the Mount Sinai School of Medicine. Lewis is a specialist in the field of gastrointestinal endoscopy and was the primary investigator for the first clinical trial of capsule endoscopy for the small intestine and also the first clinical trial of capsule endoscopy for the colon.
Peter B. Cotton is a British Gastroenterologist best known for his advancement in digestive disease, pioneering and naming the ERCP procedure and creating the Digestive Disease Center at the Medical University of South Carolina.

Michel Kahaleh is an American gastroenterologist and an expert in therapeutic endoscopy.
In medicine, endoscopic sleeve gastroplasty (ESG) is a minimally-invasive, non-surgical (incisionless), endoscopic weight loss procedure that is part of the field of endoscopic bariatric therapies. To perform ESG, a physician sutures a patient’s stomach into a narrower, smaller tube-like configuration. The result is a more restricted stomach that forces patients to feel fuller sooner, eating fewer calories, which facilitates weight loss.

Cheri L. Canon is an American abdominal radiologist at the University of Alabama at Birmingham School of Medicine Department of Radiology. She currently serves as a professor and as the Witten-Stanley Endowed Chair of Radiology in the department of radiology at UAB.

Sharmila Anandasabapathy is a Sri Lankan-American physician and researcher in the field of gastrointestinal cancer. She is a professor of medicine in gastroenterology and serves as director of Baylor Global Health and vice president at the Baylor College of Medicine.

Nib Soehendra is a German surgeon known for numerous contributions to the field of endoscopy and therapeutic endoscopy.
Prateek SharmaFACG, FACP, FASGE is an Indian American gastroenterologist that specializes in esophageal diseases and endoscopic treatments.

Kenneth Frank Binmoeller is a medical doctor and author of multiple scientific contributions and over 300 publications, as well as the inventor of the lumen-apposing metal stent (LAMS) and AXIOS System. These are medical devices used to relieve blockages while creating a direct connection between two bodily structures. He practices in the field of Gastroenterology with a specialty of Advanced Endoscopic Intervention. Binmoeller has been published for his innovations in medical devices and training in the field of Endoscopy.