Scoliosis is a condition in which a person's spine has an irregular curve. The curve is usually S- or C-shaped over three dimensions. In some, the degree of curve is stable, while in others, it increases over time. Mild scoliosis does not typically cause problems, but more severe cases can affect breathing and movement. Pain is usually present in adults, and can worsen with age. As the condition progresses, it may alter a person's life, and hence can also be considered a disability.

Kyphosis is an abnormally excessive convex curvature of the spine as it occurs in the thoracic and sacral regions. Abnormal inward concave lordotic curving of the cervical and lumbar regions of the spine is called lordosis. It can result from degenerative disc disease; developmental abnormalities, most commonly Scheuermann's disease; Copenhagen disease, osteoporosis with compression fractures of the vertebra; multiple myeloma; or trauma. A normal thoracic spine extends from the 1st thoracic to the 12th thoracic vertebra and should have a slight kyphotic angle, ranging from 20° to 45°. When the "roundness" of the upper spine increases past 45° it is called kyphosis or "hyperkyphosis". Scheuermann's kyphosis is the most classic form of hyperkyphosis and is the result of wedged vertebrae that develop during adolescence. The cause is not currently known and the condition appears to be multifactorial and is seen more frequently in males than females.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

Degenerative disc disease (DDD) is a medical condition typically brought on by the normal aging process in which there are anatomic changes and possibly a loss of function of one or more intervertebral discs of the spine. DDD can take place with or without symptoms, but is typically identified once symptoms arise. The root cause is thought to be loss of soluble proteins within the fluid contained in the disc with resultant reduction of the oncotic pressure, which in turn causes loss of fluid volume. Normal downward forces cause the affected disc to lose height, and the distance between vertebrae is reduced. The anulus fibrosus, the tough outer layers of a disc, also weakens. This loss of height causes laxity of the longitudinal ligaments, which may allow anterior, posterior, or lateral shifting of the vertebral bodies, causing facet joint malalignment and arthritis; scoliosis; cervical hyperlordosis; thoracic hyperkyphosis; lumbar hyperlordosis; narrowing of the space available for the spinal tract within the vertebra ; or narrowing of the space through which a spinal nerve exits with resultant inflammation and impingement of a spinal nerve, causing a radiculopathy.

The Harrington rod is a stainless steel surgical device. Historically, this rod was implanted along the spinal column to treat, among other conditions, a lateral or coronal-plane curvature of the spine, or scoliosis. Up to one million people had Harrington rods implanted for scoliosis between the early 1960s and the late 1990s.

Shriners Children's is a network of non-profit medical facilities across North America. Children with orthopaedic conditions, burns, spinal cord injuries, and cleft lip and palate are eligible for care and receive all services in a family-centered environment, regardless of the patients' ability to pay. Care for children is usually provided until age 18, although in some cases, it may be extended to age 21.

A back brace is a device designed to limit the motion of the spine in cases of bone fracture or in post-operative spinal fusiona, as well as a preventative measure against some progressive conditions or to correct patient posture.

Spinal fusion, also called spondylodesis or spondylosyndesis, is a surgery performed by orthopaedic surgeons or neurosurgeons that joins two or more vertebrae. This procedure can be performed at any level in the spine and prevents any movement between the fused vertebrae. There are many types of spinal fusion and each technique involves using bone grafting—either from the patient (autograft), donor (allograft), or artificial bone substitutes—to help the bones heal together. Additional hardware is often used to hold the bones in place while the graft fuses the two vertebrae together. The placement of hardware can be guided by fluoroscopy, navigation systems, or robotics.

Scheuermann's disease is a self-limiting skeletal disorder of childhood. Scheuermann's disease describes a condition where the vertebrae grow unevenly with respect to the sagittal plane; that is, the posterior angle is often greater than the anterior. This uneven growth results in the signature "wedging" shape of the vertebrae, causing kyphosis. It is named after Danish surgeon Holger Scheuermann.
Tethered cord syndrome (TCS) refers to a group of neurological disorders that relate to malformations of the spinal cord. Various forms include tight filum terminale, lipomeningomyelocele, split cord malformations (diastematomyelia), occult, dermal sinus tracts, and dermoids. All forms involve the pulling of the spinal cord at the base of the spinal canal, literally a tethered cord. The spinal cord normally hangs loose in the canal, free to move up and down with growth, and with bending and stretching. A tethered cord, however, is held taut at the end or at some point in the spinal canal. In children, a tethered cord can force the spinal cord to stretch as they grow. In adults the spinal cord stretches in the course of normal activity, usually leading to progressive spinal cord damage if untreated. TCS is often associated with the closure of a spina bifida. It can be congenital, such as in tight filum terminale, or the result of injury later in life.
The Boston brace, a type of thoraco-lumbo-sacral-orthosis (TLSO), is a back brace used primarily for the treatment of idiopathic scoliosis in children. It was developed in 1972 by M.E "Bill" Miller and John Hall at the Boston Children's Hospital in Boston, Massachusetts.

Spinal disease refers to a condition impairing the backbone. These include various diseases of the back or spine ("dorso-"), such as kyphosis. Dorsalgia refers to back pain. Some other spinal diseases include spinal muscular atrophy, ankylosing spondylitis, scoliosis, lumbar spinal stenosis, spina bifida, spinal tumors, osteoporosis and cauda equina syndrome.

The Scoliosis Research Society (SRS) is a non-profit, professional, international organization made up of physicians and allied health personnel, whose purpose is to "care for those with spinal deformity throughout life by patient care, education, research and patient advocacy." It was founded in 1966 with 37 members, and now has grown to include over 1300 spinal deformity surgeons and allied health personnel in 41 countries, with a primary focus on providing continuing medical education for health care professionals, and funding/support for research in spinal deformities. Among the founding members were Dr. Paul Randall Harrington, inventor of the Harrington rod treatment for scoliosis, and Dr. David B. Levine, spine surgeon at Hospital for Special Surgery. Harrington later served as President of the SRS from 1972 to 1973, and Levine was President of the Society from 1978 to 1979. Current membership primarily includes spinal deformity surgeons, as well as some researchers, physician assistants, and orthotists who are involved in research and treatment of spinal deformities. Strict membership criteria ensure that the individual SRS Fellows are dedicated to the highest standards of care for adult and pediatric spinal deformities, utilizing both non-operative and operative techniques.
Sean E. McCance is an American orthopedic surgeon and Co-Director of Spine Surgery in the Leni and Peter W. May Department of Orthopaedics at the Mount Sinai Medical Center in New York City. Additionally, he is an Associate Clinical Professor of Orthopaedics at the Mount Sinai School of Medicine and Attending Spine Physician at Lenox Hill Hospital.

The neuromechanics of idiopathic scoliosis is about the changes in the bones, muscles and joints in cases of spinal deformity consisting of a lateral curvature scoliosis and a rotation of the vertebrae within the curve, that is not explained by either congenital vertebral abnormalities, or neuromuscular disorders such as muscular dystrophy. The idiopathic scoliosis accounts for 80–90% of scoliosis cases. Its pathogenesis is unknown. However, changes in the vestibular system, a lateral shift of the hand representation and abnormal variability of erector spinae motor map location in the motor cortex may be involved in this disease. A short spinal cord and associated nerve tensions has been proposed as a cause and model for idiopathic scoliosis. Besides idiopathic scoliosis being more frequent in certain families, it is suspected to be transmitted via autosomal dominant inheritance. Estrogens could also play a crucial part in the progression of idiopathic scoliosis through their roles in bone formation, growth, maturation and turnover. Finally, collagen, intervertebral disc and muscle abnormalities have been suggested as the cause in idiopathic scoliosis, although these are perhaps results rather than causes.

The vertebral column, also known as the spinal column, spine or backbone, is the core part of the axial skeleton in vertebrate animals. The vertebral column is the defining and eponymous characteristic of the vertebrate endoskeleton, where the notochord found in all chordates has been replaced by a segmented series of mineralized irregular bones called vertebrae, separated by fibrocartilaginous intervertebral discs. The dorsal portion of the vertebral column houses the spinal canal, an elongated cavity formed by alignment of the vertebral neural arches that encloses and protects the spinal cord, with spinal nerves exiting via the intervertebral foramina to innervate each body segments.
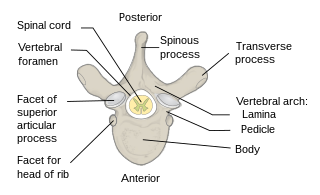
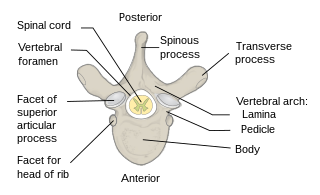
Each vertebra is an irregular bone with a complex structure composed of bone and some hyaline cartilage, that make up the vertebral column or spine, of vertebrates. The proportions of the vertebrae differ according to their spinal segment and the particular species.
The management of scoliosis is complex and is determined primarily by the type of scoliosis encountered: syndromic, congenital, neuromuscular, or idiopathic. Treatment options for idiopathic scoliosis are determined in part by the severity of the curvature and skeletal maturity, which together help predict the likelihood of progression. Non-surgical treatment should be pro-active with intervention performed early as "Best results were obtained in 10-25 degrees scoliosis which is a good indication to start therapy before more structural changes within the spine establish." Treatment options have historically been categorized under the following types:
- Observation
- Bracing
- Specialized physical therapy
- Surgery
The Providence brace is a nighttime spinal orthosis for the treatment of adolescent idiopathic scoliosis (AIS). The brace is used to curb the natural progression of the disease and prevent further curvature of the AIS patient's spine. The Providence brace was developed by Charles d'Amato and Barry McCoy, and is manufactured by Spinal Technology, Inc.

Halo-gravity traction (HGT) is a type of traction device utilized to treat spinal deformities such as scoliosis, congenital spine deformities, cervical instability, basilar invagination, and kyphosis. It is used prior to surgical treatment to reduce the difficulty of the following surgery and the need for a more dangerous surgery. The device works by applying weight to the spine in order to stretch and straighten it. Patients are capable of remaining somewhat active using a wheelchair or a walker whilst undergoing treatment. Most of the research suggests that HGT is a safe treatment, and it can even improve patients' nutrition or respiratory functioning. However, some patients may experience side effects such as headaches or neurological complications. The halo device itself was invented in the 1960s by doctors working at the Riancho Los Amigos hospital. Their work was published in a paper entitled "The Halo: A Spinal Skeletal Traction Fixation Device." The clinician Pierre Stagnara utilized the device to develop Halo-Gravity traction.