Related Research Articles

Cartilage is a resilient and smooth type of connective tissue. In tetrapods, it covers and protects the ends of long bones at the joints as articular cartilage, and is a structural component of many body parts including the rib cage, the neck and the bronchial tubes, and the intervertebral discs. In other taxa, such as chondrichthyans, but also in cyclostomes, it may constitute a much greater proportion of the skeleton. It is not as hard and rigid as bone, but it is much stiffer and much less flexible than muscle. The matrix of cartilage is made up of glycosaminoglycans, proteoglycans, collagen fibers and, sometimes, elastin.

Rhinoplasty, commonly called nose job, medically called nasal reconstruction is a plastic surgery procedure for altering and reconstructing the nose. There are two types of plastic surgery used – reconstructive surgery that restores the form and functions of the nose and cosmetic surgery that changes the appearance of the nose. Reconstructive surgery seeks to resolve nasal injuries caused by various traumas including blunt, and penetrating trauma and trauma caused by blast injury. Reconstructive surgery can also treat birth defects, breathing problems, and failed primary rhinoplasties. Rhinoplasty may remove a bump, narrow nostril width, change the angle between the nose and the mouth, or address injuries, birth defects, or other problems that affect breathing, such as a deviated nasal septum or a sinus condition. Surgery only on the septum is called a septoplasty.
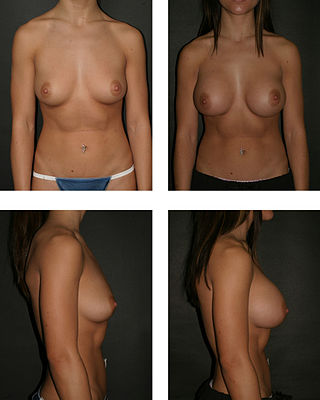
Breast augmentation and augmentation mammoplasty is a cosmetic surgery technique using breast-implants and fat-graft mammoplasty techniques to increase the size, change the shape, and alter the texture of the breasts. Augmentation mammoplasty is applied to correct congenital defects of the breasts and the chest wall. As an elective cosmetic surgery, primary augmentation changes the aesthetics – of size, shape, and texture – of healthy breasts.
Grafting refers to a surgical procedure to move tissue from one site to another on the body, or from another creature, without bringing its own blood supply with it. Instead, a new blood supply grows in after it is placed. A similar technique where tissue is transferred with the blood supply intact is called a flap. In some instances, a graft can be an artificially manufactured device. Examples of this are a tube to carry blood flow across a defect or from an artery to a vein for use in hemodialysis.

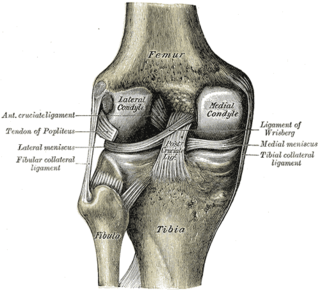
The long bones are those that are longer than they are wide. They are one of five types of bones: long, short, flat, irregular and sesamoid. Long bones, especially the femur and tibia, are subjected to most of the load during daily activities and they are crucial for skeletal mobility. They grow primarily by elongation of the diaphysis, with an epiphysis at each end of the growing bone. The ends of epiphyses are covered with hyaline cartilage. The longitudinal growth of long bones is a result of endochondral ossification at the epiphyseal plate. Bone growth in length is stimulated by the production of growth hormone (GH), a secretion of the anterior lobe of the pituitary gland.
Dysbaric osteonecrosis or DON is a form of avascular necrosis where there is death of a portion of the bone that is thought to be caused by nitrogen embolism in divers. Although the definitive pathologic process is poorly understood, there are several hypotheses:

Bone grafting is a surgical procedure that replaces missing bone in order to repair bone fractures that are extremely complex, pose a significant health risk to the patient, or fail to heal properly. Some small or acute fractures can be cured without bone grafting, but the risk is greater for large fractures like compound fractures.
Autotransplantation is the transplantation of organs, tissues, or even particular proteins from one part of the body to another in the same person.

Osteochondritis dissecans is a joint disorder primarily of the subchondral bone in which cracks form in the articular cartilage and the underlying subchondral bone. OCD usually causes pain during and after sports. In later stages of the disorder there will be swelling of the affected joint which catches and locks during movement. Physical examination in the early stages does only show pain as symptom, in later stages there could be an effusion, tenderness, and a crackling sound with joint movement.
Articular cartilage, most notably that which is found in the knee joint, is generally characterized by very low friction, high wear resistance, and poor regenerative qualities. It is responsible for much of the compressive resistance and load bearing qualities of the knee joint and, without it, walking is painful to impossible. Osteoarthritis is a common condition of cartilage failure that can lead to limited range of motion, bone damage and invariably, pain. Due to a combination of acute stress and chronic fatigue, osteoarthritis directly manifests itself in a wearing away of the articular surface and, in extreme cases, bone can be exposed in the joint. Some additional examples of cartilage failure mechanisms include cellular matrix linkage rupture, chondrocyte protein synthesis inhibition, and chondrocyte apoptosis. There are several different repair options available for cartilage damage or failure.
Microfracture surgery is an articular cartilage repair surgical technique that works by creating tiny fractures in the underlying bone. This causes new cartilage to develop from a so-called super-clot.
Articular cartilage repair treatment is focused on the restoration of the surface of an articular joint's hyaline cartilage. Over the last few decades, surgeons and researchers have made progress in elaborating surgical cartilage repair interventions. Though these solutions do not perfectly restore the articular cartilage, some of the latest technologies start to bring very promising results in repairing cartilages from traumatic injuries or chondropathies. These treatments are especially targeted for patients who have articular cartilage damage. They provide pain relief, while at the same time slowing down the progression of damage or considerably delaying the joint replacement surgery. Articular cartilage repair treatments helps patients to return to their original lifestyle with reduced pain, regaining mobility, going back to work, and even practicing sports again.
Cartilage structures and functions can be damaged. Such damage can result from a variety of causes, such as a bad fall or traumatic sport-accident, previous knee injuries or wear and tear over time. Immobilization for long periods can also result in cartilage damage.
Autologous chondrocyte implantation is a biomedical treatment that repairs damages in articular cartilage. ACI provides pain relief while at the same time slowing down the progression or considerably delaying partial or total joint replacement surgery. The goal of ACI is to allow people suffering from articular cartilage damage to return to their old lifestyle; regaining mobility, going back to work and even practicing sports again.
Mesenchymal stem cells (MSCs) are multipotent cells found in multiple human adult tissues including bone marrow, synovial tissues, and adipose tissues. Since they are derived from the mesoderm, they have been shown to differentiate into bone, cartilage, muscle, and adipose tissue. MSCs from embryonic sources have shown promise scientifically while creating significant controversy. As a result, many researchers have focused on adult stem cells, or stem cells isolated from adult humans that can be transplanted into damaged tissue.
Kevin Robert Stone, M.D. is a physician, orthopedic surgeon, clinician, researcher, and company founder of The Stone Clinic and the Stone Research Foundation in San Francisco.
Autologous matrix-induced chondrogenesis (AMIC) is a treatment for articular cartilage damage. It combines microfracture surgery with the application of a bi-layer collagen I/III membrane. There is tentative short to medium term benefits as of 2017.
The treatment of equine lameness is a complex subject. Lameness in horses has a variety of causes, and treatment must be tailored to the type and degree of injury, as well as the financial capabilities of the owner. Treatment may be applied locally, systemically, or intralesionally, and the strategy for treatment may change as healing progresses. The end goal is to reduce the pain and inflammation associated with injury, to encourage the injured tissue to heal with normal structure and function, and to ultimately return the horse to the highest level of performance possible following recovery.
Martinus Richter is a German orthopaedic surgeon, and Associate Professor at the Hannover Medical School and Head of the Department for Foot and Ankle Surgery Nuremberg and Rummelsberg at the Hospital Rummelsberg and Sana-Hospital Nuremberg.
Nasal chondrocytes (NC) are present in the hyaline cartilage of the nasal septum and in fact are the only cell type within the tissue. Similar to chondrocytes present in articular cartilage, NC express extracellular matrix proteins such as glycosaminoglycans and collagen.
References
- 1 2 3 Stone, KR; Walgenbach, AW; Freyer, A; Turek, TJ; Speer, DP (Mar 2006). "Articular cartilage paste grafting to full-thickness articular cartilage knee joint lesions: a 2- to 12-year follow-up". Arthroscopy. 22 (3): 291–9. doi:10.1016/j.arthro.2005.12.051. PMID 16517314.
- ↑ Kon, E; Vannini, F; Buda, R; Filardo, G; Cavallo, M; Ruffilli, A; Nanni, M; Di Martino, A; Marcacci, M; Giannini, S (Jan 4, 2012). "How to treat osteochondritis dissecans of the knee: surgical techniques and new trends: AAOS exhibit selection". The Journal of Bone and Joint Surgery. American Volume. 94 (1): e1(1–8). doi:10.2106/JBJS.K.00748. PMID 22218387. S2CID 34945123.
- ↑ Jaroszewski, J; Kruczyński, J; Piontek, T; Trzeciak, T; Lubiatowski, P (2003). "[The value of autologous osteochondral paste for in-vitro treatment of damage to articular cartilage. Part I. Macroscopic and microscopic assessment of the regenerated articular surface]". Chirurgia Narzadow Ruchu I Ortopedia Polska. 68 (4): 237–41. PMID 14702675.
- ↑ Jaroszewski, J; Kruczyński, J; Piontek, T; Trzeciak, T; Kaszuba, B; Lubiatowski, P (2003). "[Value of autologous transplantation of osteo-chondral paste in reconstruction of experimental cartilage defects. Part II. Microscopic analysis of integration with surrounding cartilage, structural integrity and subchondral bone reconstruction in repair tissue]". Chirurgia Narzadow Ruchu I Ortopedia Polska. 68 (5): 335–40. PMID 15104045.
- ↑ Jaroszewski, J; Kruczyński, J; Trzeciak, T; Lubiatowski, P; Kaszuba, B (2004). "[Value of osteo-chondral paste autologous transplantation in experimental cartilage defects reconstruction. Part III--Microscopic analysis of reconstructed cartilage thickness and surface regularity]". Chirurgia Narzadow Ruchu I Ortopedia Polska. 69 (1): 35–9. PMID 15305672.
- ↑ Jaroszewski, J; Kruczyński, J; Trzeciak, T; Piontek, T; Kaszuba, B (2004). "[Value of osteo-chondral paste autologous transplantation in experimental cartilage defects reconstruction. Part IV--Microscopic analysis of cellularity and of traits of necrosis in the defect-filling tissue]". Chirurgia Narzadow Ruchu I Ortopedia Polska. 69 (2): 115–9. PMID 15307383.
- ↑ Buckwalter, JA; Lohmander, S (Sep 1994). "Operative treatment of osteoarthrosis. Current practice and future development". The Journal of Bone and Joint Surgery. American Volume. 76 (9): 1405–18. doi:10.2106/00004623-199409000-00019. PMID 8077274.
- ↑ Buckwalter, J.A.; ManKin, J.J. (April 1997). "Instructional Course Lectures, The American Academy of Orthopaedic Surgeons - Articular Cartilage. Part II: Degeneration and Osteoarthrosis, Repair, Regeneration, and Transplantation". J Bone Joint Surg Am. 79 (4): 612–32. doi:10.2106/JBJS.J.01935. PMID 22810408.
- ↑ Stone, KR; Walgenbach, A (1997). "Surgical technique for articular cartilage transplantation to full-thickness cartilage defects in the knee joint". Operative Techniques in Orthopaedics. 7 (4): 305–11. doi:10.1016/s1048-6666(97)80034-1.
- ↑ Stone, KR; Walgenbach, A (1998). "Articular cartilage paste grafting: Surgical technique and initial results". European Journal of Sports Traumatology and Related Research. 20 (2): 71–79.