Lumbar spinal stenosis (LSS) is a medical condition in which the spinal canal narrows and compresses the nerves and blood vessels at the level of the lumbar vertebrae. Spinal stenosis may also affect the cervical or thoracic region, in which case it is known as cervical spinal stenosis or thoracic spinal stenosis. Lumbar spinal stenosis can cause pain in the low back or buttocks, abnormal sensations, and the absence of sensation (numbness) in the legs, thighs, feet, or buttocks, or loss of bladder and bowel control.

A laminectomy is a surgical procedure that removes a portion of a vertebra called the lamina, which is the roof of the spinal canal. It is a major spine operation with residual scar tissue and may result in postlaminectomy syndrome. Depending on the problem, more conservative treatments may be viable.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related wear and tear of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

Degenerative disc disease (DDD) is a medical condition typically brought on by the normal aging process in which there are anatomic changes and possibly a loss of function of one or more intervertebral discs of the spine. DDD can take place with or without symptoms, but is typically identified once symptoms arise. The root cause is thought to be loss of soluble proteins within the fluid contained in the disc with resultant reduction of the oncotic pressure, which in turn causes loss of fluid volume. Normal downward forces cause the affected disc to lose height, and the distance between vertebrae is reduced. The anulus fibrosus, the tough outer layers of a disc, also weakens. This loss of height causes laxity of the longitudinal ligaments, which may allow anterior, posterior, or lateral shifting of the vertebral bodies, causing facet joint malalignment and arthritis; scoliosis; cervical hyperlordosis; thoracic hyperkyphosis; lumbar hyperlordosis; narrowing of the space available for the spinal tract within the vertebra ; or narrowing of the space through which a spinal nerve exits with resultant inflammation and impingement of a spinal nerve, causing a radiculopathy.

Spondylolisthesis is the displacement of one spinal vertebra compared to another. While some medical dictionaries define spondylolisthesis specifically as the forward or anterior displacement of a vertebra over the vertebra inferior to it, it is often defined in medical textbooks as displacement in any direction. Spondylolisthesis is graded based upon the degree of slippage of one vertebral body relative to the subsequent adjacent vertebral body. Spondylolisthesis is classified as one of the six major etiologies: degenerative, traumatic, dysplastic, isthmic, pathologic, or post-surgical. Spondylolisthesis most commonly occurs in the lumbar spine, primarily at the L5-S1 level with the L5 vertebral body anteriorly translating over the S1 vertebral body.

Cauda equina syndrome (CES) is a condition that occurs when the bundle of nerves below the end of the spinal cord known as the cauda equina is damaged. Signs and symptoms include low back pain, pain that radiates down the leg, numbness around the anus, and loss of bowel or bladder control. Onset may be rapid or gradual.

Klippel–Feil syndrome (KFS), also known as cervical vertebral fusion syndrome, is a rare congenital condition characterized by the abnormal fusion of any two of the seven bones in the neck. It results in a limited ability to move the neck and shortness of the neck, resulting in the appearance of a low hairline.
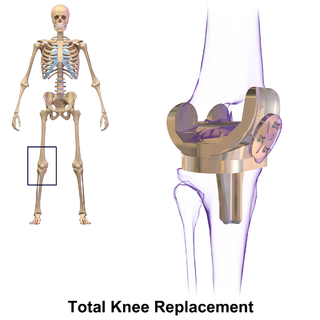
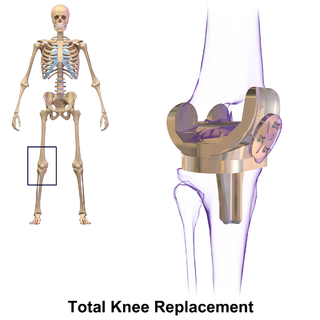
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability, most commonly offered when joint pain is not diminished by conservative sources and also for other knee diseases such as rheumatoid arthritis and psoriatic arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation and is not a reason to perform knee replacement.

Spinal fusion, also called spondylodesis or spondylosyndesis, is a neurosurgical or orthopedic surgical technique that joins two or more vertebrae. This procedure can be performed at any level in the spine and prevents any movement between the fused vertebrae. There are many types of spinal fusion and each technique involves using bone grafting—either from the patient (autograft), donor (allograft), or artificial bone substitutes—to help the bones heal together. Additional hardware is often used to hold the bones in place while the graft fuses the two vertebrae together. The placement of hardware can be guided by fluoroscopy, navigation systems, or robotics.
Failed back syndrome or post-laminectomy syndrome is a condition characterized by chronic pain following back surgeries. Many factors can contribute to the onset or development of FBS, including residual or recurrent spinal disc herniation, persistent post-operative pressure on a spinal nerve, altered joint mobility, joint hypermobility with instability, scar tissue (fibrosis), depression, anxiety, sleeplessness, spinal muscular deconditioning and even Cutibacterium acnes infection. An individual may be predisposed to the development of FBS due to systemic disorders such as diabetes, autoimmune disease and peripheral blood vessels (vascular) disease.

Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly. Radiculopathy can result in pain, weakness, altered sensation (paresthesia) or difficulty controlling specific muscles. Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.

Neurogenic claudication (NC), also known as pseudoclaudication, is the most common symptom of lumbar spinal stenosis (LSS) and describes intermittent leg pain from impingement of the nerves emanating from the spinal cord. Neurogenic means that the problem originates within the nervous system. Claudication, from the Latin word for to limp, refers to painful cramping or weakness in the legs. NC should therefore be distinguished from vascular claudication, which stems from a circulatory problem rather than a neural one.

Shoulder replacement is a surgical procedure in which all or part of the glenohumeral joint is replaced by a prosthetic implant. Such joint replacement surgery generally is conducted to relieve arthritis pain or fix severe physical joint damage.
Artificial disc replacement (ADR), or total disc replacement (TDR), is a type of arthroplasty. It is a surgical procedure in which degenerated intervertebral discs in the spinal column are replaced with artificial disc implants in the lumbar (lower) or cervical (upper) spine. The procedure is used to treat chronic, severe low back pain and cervical pain resulting from degenerative disc disease. Disc replacement is also an alternative intervention for symptomatic disc herniation with associated arm and hand, or leg symptoms.
Robert S. Biscup is an American orthopaedic surgeon.
Metallosis is the putative medical condition involving deposition and build-up of metal debris in the soft tissues of the body.

Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots. Symptoms may include pain, numbness, or weakness in the arms or legs. Symptoms are typically gradual in onset and improve with leaning forward. Severe symptoms may include loss of bladder control, loss of bowel control, or sexual dysfunction.
Minimally invasive spine surgery, also known as MISS, has no specific meaning or definition. It implies a lack of severe surgical invasion. The older style of open-spine surgery for a relatively small disc problem used to require a 5-6 inch incision and a month in the hospital. MISS techniques utilize more modern technology, advanced imaging techniques and special medical equipment to reduce tissue trauma, bleeding, radiation exposure, infection risk, and decreased hospital stays by minimizing the size of the incision. Modern endoscopic procedures can be done through a 2 to 5 mm skin opening. By contrast, procedures done with a microscope require skin openings of approximately one inch, or more.

Thomas Schuler, M.D., F.A.C.S is an American spinal surgeon, researcher and educator in the treatment of neck and low back conditions. He was an early adopter of stem cell therapy, biologics, robotics, laser and hybrid surgery and augmented reality for spinal surgery. Schuler specializes in cervical and lumbar disc replacement procedures, minimally invasive spine surgery and robotic spine surgery. He performed the first hybrid multi-level cervical artificial disc replacement with spinal fusion in the country. He founded a practice that has performed some of the first robotic and augmented reality spinal surgeries in the world. In 2002 he created and currently serves as President of the National Spine Health Foundation, a national non-profit focused on education, research and patient advocacy of neck and back health.