Related Research Articles

A gonad, sex gland, or reproductive gland is a mixed gland that produces the gametes and sex hormones of an organism. Female reproductive cells are egg cells, and male reproductive cells are sperm. The male gonad, the testicle, produces sperm in the form of spermatozoa. The female gonad, the ovary, produces egg cells. Both of these gametes are haploid cells. Some hermaphroditic animals have a type of gonad called an ovotestis.

Intracytoplasmic sperm injection is an in vitro fertilization (IVF) procedure in which a single sperm cell is injected directly into the cytoplasm of an egg. This technique is used in order to prepare the gametes for the obtention of embryos that may be transferred to a maternal uterus. With this method, the acrosome reaction is skipped.

Spermatogenesis is the process by which haploid spermatozoa develop from germ cells in the seminiferous tubules of the testis. This process starts with the mitotic division of the stem cells located close to the basement membrane of the tubules. These cells are called spermatogonial stem cells. The mitotic division of these produces two types of cells. Type A cells replenish the stem cells, and type B cells differentiate into primary spermatocytes. The primary spermatocyte divides meiotically into two secondary spermatocytes; each secondary spermatocyte divides into two equal haploid spermatids by Meiosis II. The spermatids are transformed into spermatozoa (sperm) by the process of spermiogenesis. These develop into mature spermatozoa, also known as sperm cells. Thus, the primary spermatocyte gives rise to two cells, the secondary spermatocytes, and the two secondary spermatocytes by their subdivision produce four spermatozoa and four haploid cells.
David C. Page is an American biologist and professor at the Massachusetts Institute of Technology (MIT), the director of the Whitehead Institute, and a Howard Hughes Medical Institute (HHMI) investigator. He is best known for his work on mapping the Y-chromosome and on its evolution in mammals and expression during development. He was cited by Bryan Sykes in Adam's Curse: A Future Without Men.

Y linkage, also known as holandric inheritance, describes traits that are produced by genes located on the Y chromosome. It is a form of sex linkage.

Azoospermia is the medical condition of a man whose semen contains no sperm. It is associated with male infertility, but many forms are amenable to medical treatment. In humans, azoospermia affects about 1% of the male population and may be seen in up to 20% of male infertility situations in Canada.
Terms oligospermia, oligozoospermia, and low sperm count refer to semen with a low concentration of sperm and is a common finding in male infertility. Often semen with a decreased sperm concentration may also show significant abnormalities in sperm morphology and motility. There has been interest in replacing the descriptive terms used in semen analysis with more quantitative information.
Y chromosome microdeletion(YCM) is a family of genetic disorders caused by missing genes in the Y chromosome. Many men with YCM exhibit no symptoms and lead normal lives. It is present in a significant number of men with reduced fertility. Reduced sperm production varies from oligozoospermia, significant lack of sperm, or azoospermia, complete lack of sperm.
Male infertility refers to a sexually mature male's inability to impregnate a fertile female. In humans it accounts for 40–50% of infertility. It affects approximately 7% of all men. Male infertility is commonly due to deficiencies in the semen, and semen quality is used as a surrogate measure of male fecundity. More recently, advance sperm analyses that examine intracellular sperm components are being developed.

Deleted in azoospermia-like is a protein that in humans is encoded by the DAZL gene.

Sertoli cell-only syndrome (SCOS), also known as germ cell aplasia, is defined by azoospermia where the testicular seminiferous tubules are lined solely with sertoli cells. Sertoli cells contribute to the formation of the blood-testis barrier and aid in sperm generation. These cells respond to follicle-stimulating hormone, which is secreted by the hypothalamus and aids in spermatogenesis.

Deleted in azoospermia 1, also known as DAZ1, is a protein which in humans is encoded by the DAZ1 gene.

Ubiquitin specific peptidase 9, Y-linked , also known as USP9Y, is an enzyme which in humans is encoded by the USP9Y gene. It is required for sperm production. This enzyme is a member of the peptidase C19 family and is similar to ubiquitin-specific proteases, which cleave the ubiquitin moiety from ubiquitin-fused precursors and ubiquitinylated proteins.

Deleted in azoospermia protein 3 is a protein that in humans is encoded by the DAZ3 gene.

Deleted in azoospermia protein 2 is a protein that in humans is encoded by the DAZ2 gene.

DAZ-associated protein 1 is a protein that in humans is encoded by the DAZAP1 gene.

RNA-binding motif protein, Y chromosome, family 1 member A1/C is a protein that in humans is encoded by the RBMY1A1 gene.
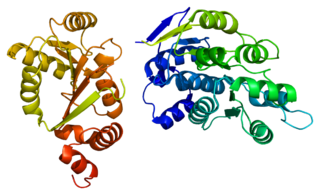
ATP-dependent RNA helicase DDX3Y is an enzyme that in humans is encoded by the DDX3Y gene.

Protein boule-like is a protein that in humans is encoded by the BOLL gene.
Ann Chester Chandley DSc, F.I.Biol., FRSE was an international cytogeneticist with the Medical Research Council unit which became the Human Genetics Unit at the University of Edinburgh. She became a Fellow of the Institute of Biology in recognition of her contribution and a Fellow of the Royal Society of Edinburgh.
References
- ↑ Repping S, Skaletsky H, Lange J, Silber S, Van Der Veen F, Oates RD, et al. (October 2002). "Recombination between palindromes P5 and P1 on the human Y chromosome causes massive deletions and spermatogenic failure". American Journal of Human Genetics. 71 (4): 906–22. doi:10.1086/342928. PMC 419997 . PMID 12297986.
- ↑ Ioulianos A, Sismani C, Fourouclas N, Patroclou T, Sergiou C, Patsalis PC (June 2002). "A nation-based population screening for azoospermia factor deletions in Greek-Cypriot patients with severe spermatogenic failure and normal fertile controls, using a specific study and experimental design". International Journal of Andrology. 25 (3): 153–8. doi: 10.1046/j.1365-2605.2002.00340.x . PMID 12031043.
- 1 2 3 4 5 6 7 8 9 10 O'Flynn O'Brien KL, Varghese AC, Agarwal A (January 2010). "The genetic causes of male factor infertility: a review". Fertility and Sterility. 93 (1): 1–12. doi: 10.1016/j.fertnstert.2009.10.045 . PMID 20103481.
- 1 2 3 4 5 6 7 8 9 10 Colaco S, Modi D (February 2018). "Genetics of the human Y chromosome and its association with male infertility". Reproductive Biology and Endocrinology. 16 (1): 14. doi: 10.1186/s12958-018-0330-5 . PMC 5816366 . PMID 29454353.
- 1 2 Nailwal M, Chauhan JB (2017). "Azoospermia Factor C Subregion of the Y Chromosome". Journal of Human Reproductive Sciences. 10 (4): 256–260. doi: 10.4103/jhrs.JHRS_16_17 . PMC 5799928 . PMID 29430151.
- 1 2 3 4 5 6 7 Yu XW, Wei ZT, Jiang YT, Zhang SL (2015). "Y chromosome azoospermia factor region microdeletions and transmission characteristics in azoospermic and severe oligozoospermic patients". International Journal of Clinical and Experimental Medicine. 8 (9): 14634–46. PMC 4658835 . PMID 26628946.
- ↑ Komori S, Kato H, Kobayashi S, Koyama K, Isojima S (2002). "Transmission of Y chromosomal microdeletions from father to son through intracytoplasmic sperm injection". Journal of Human Genetics. 47 (9): 465–8. doi: 10.1007/s100380200066 . PMID 12202984.
- ↑ Vogt PH (2005). "AZF deletions and Y chromosomal haplogroups: history and update based on sequence". Human Reproduction Update. 11 (4): 319–36. doi: 10.1093/humupd/dmi017 . PMID 15890785.
- ↑ Stouffs K, Lissens W, Tournaye H, Haentjens P (2010). "What about gr/gr deletions and male infertility? Systematic review and meta-analysis". Human Reproduction Update. 17 (2): 197–209. doi: 10.1093/humupd/dmq046 . PMID 20959348.