Related Research Articles
Shortness of breath (SOB), known as dyspnea or dyspnoea, is an uncomfortable feeling of not being able to breathe well enough. The American Thoracic Society defines it as "a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity", and recommends evaluating dyspnea by assessing the intensity of its distinct sensations, the degree of distress and discomfort involved, and its burden or impact on the patient's activities of daily living. Distinct sensations include effort/work to breathe, chest tightness or pain, and "air hunger". The tripod position is often assumed to be a sign.

Spirometry is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD. It is also helpful as part of a system of health surveillance, in which breathing patterns are measured over time.

Exercise intolerance is a condition of inability or decreased ability to perform physical exercise at the normally expected level or duration for people of that age, size, sex, and muscle mass. It also includes experiences of unusually severe post-exercise pain, fatigue, nausea, vomiting or other negative effects. Exercise intolerance is not a disease or syndrome in and of itself, but can result from various disorders.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.
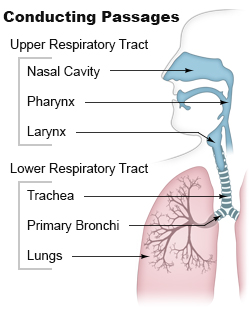
Airway obstruction is a blockage of respiration in the airway that hinders the free flow of air. Airway obstructions can occur either in the upper airway (UPA) or lower airway (LOA). The upper airway consists of the nose, throat, and larynx. The lower airway comprises the trachea, bronchi, and bronchioles.
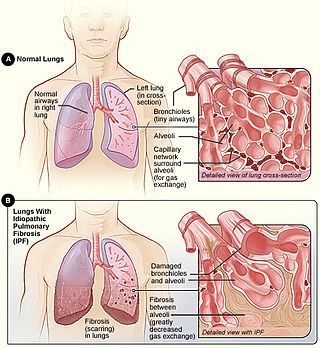
Idiopathic pulmonary fibrosis (IPF) synonymous with cryptogenic fibrosing alveolitis is a rare, progressive illness of the respiratory system, characterized by the thickening and stiffening of lung tissue, associated with the formation of scar tissue. It is a type of chronic pulmonary fibrosis characterized by a progressive and irreversible decline in lung function.

Erdosteine is a molecule with mucolytic activity. Structurally it is a thioether derivative with two thioether groups. These two functional organosulfur groups contained in the molecule are released following first-pass metabolism with the conversion of erdosteine into its pharmacologically active metabolite Met-I.
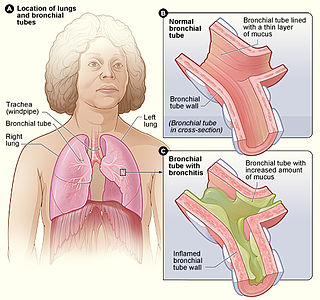
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.
Restrictive lung diseases are a category of extrapulmonary, pleural, or parenchymal respiratory diseases that restrict lung expansion, resulting in a decreased lung volume, an increased work of breathing, and inadequate ventilation and/or oxygenation. Pulmonary function test demonstrates a decrease in the forced vital capacity.

Pulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a pulmonary function technologist, respiratory therapist, respiratory physiologist, physiotherapist, pulmonologist, or general practitioner.

The FEV1/FVC ratio, also called modified Tiffeneau-Pinelli index, is a calculated ratio used in the diagnosis of obstructive and restrictive lung disease. It represents the proportion of a person's vital capacity that they are able to expire in the first second of forced expiration (FEV1) to the full, forced vital capacity (FVC). FEV1/FVC ratio was first proposed by E.A. Haensler in 1950. The FEV1/FVC index should not be confused with the FEV1/VC index as they are different, although both are intended for diagnosing airway obstruction. Current recommendations for diagnosing pulmonary function recommend using the modified Tiffeneau-Pinelli index. This index is recommended to be represented as a decimal fraction with two digits after the decimal point.
Pulmonary rehabilitation, also known as respiratory rehabilitation, is an important part of the management and health maintenance of people with chronic respiratory disease who remain symptomatic or continue to have decreased function despite standard medical treatment. It is a broad therapeutic concept. It is defined by the American Thoracic Society and the European Respiratory Society as an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities. In general, pulmonary rehabilitation refers to a series of services that are administered to patients of respiratory disease and their families, typically to attempt to improve the quality of life for the patient. Pulmonary rehabilitation may be carried out in a variety of settings, depending on the patient's needs, and may or may not include pharmacologic intervention.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.
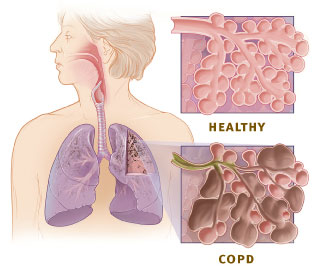
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by chronic respiratory symptoms and airflow limitation. GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms due to abnormalities of the airways and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.

Olodaterol is an ultra-long-acting β adrenoreceptor agonist (ultra-LABA) used as an inhalation for treating people with chronic obstructive pulmonary disease (COPD). It is manufactured by Boehringer Ingelheim.
Physiotherapists treating patients following uncomplicated coronary artery bypass surgery surgery continue to use interventions such as deep breathing exercises that are not supported by best available evidence. Standardised guidelines may be required to better match clinical practice with current literature.

Emphysema is any air-filled enlargement in the body's tissues. Most commonly emphysema refers to the permanent enlargement of air spaces (alveoli) in the lungs, and is also known as pulmonary emphysema.
Fluticasone furoate/umeclidinium bromide/vilanterol, sold under the brand name Trelegy Ellipta among others, is a fixed-dose combination inhaled medication that is used for the maintenance treatment of chronic obstructive pulmonary disease (COPD). The medications work in different ways: fluticasone furoate is an inhaled corticosteroid (ICS), umeclidinium is a long-acting muscarinic antagonist (LAMA), and vilanterol is a long-acting beta-agonist (LABA).
Asthma-Chronic Obstructive Pulmonary Disease (COPD) Overlap (ACO), also known as Asthma-COPD Overlap Syndrome (ACOS), is a chronic inflammatory, obstructive airway disease in which features of both asthma and COPD predominate. Asthma and COPD were once thought of as distinct entities; however, in some, there are clinical features of both asthma and COPD with significant overlap in pathophysiology and symptom profile. It is unclear whether ACO is a separate disease entity or a clinical subtype of asthma and COPD. The pathogenesis of ACO is poorly understood, but it is thought to involve both type 2 inflammation as well as type 1 inflammation. The incidence and prevalence of ACO are not well known. The risk factors for ACO are also incompletely understood, but tobacco smoke is known to be a major risk factor.
References
- ↑ Cislo, Geoffrey S.; Fer, Thomas M. De; Henderson, Katherine E. (2008-09-01). General Internal Medicine Consult (2 ed.). Lippincott Williams & Wilkins. p. 96. ISBN 978-0-7817-9155-7.
- ↑ Casanova, C.; Celli, B. R.; Barria, P. (2010-12-30). "The 6-min walk distance in healthy subjects: reference standards from seven countries". European Respiratory Journal. 37 (1): 150–156. doi:10.1183/09031936.00194909. ISSN 0903-1936. PMID 20525717.
- 1 2 Reilly, John J.; Silverman, Edwin K.; Shapiro, Steven D. (2011). "Chronic Obstructive Pulmonary Disease". In Longo, Dan; Fauci, Anthony; Kasper, Dennis; Hauser, Stephen; Jameson, J.; Loscalzo, Joseph (eds.). Harrison's Principles of Internal Medicine (18th ed.). McGraw Hill. pp. 2151–9. ISBN 978-0-07-174889-6.
- ↑ National Institute for Health and Clinical Excellence . Clinical guideline 101: Chronic Obstructive Pulmonary Disease . London, June 2010.