Related Research Articles
Nephrology is a specialty for both adult internal medicine and pediatric medicine that concerns the study of the kidneys, specifically normal kidney function and kidney disease, the preservation of kidney health, and the treatment of kidney disease, from diet and medication to renal replacement therapy. The word "renal" is an adjective meaning "relating to the kidneys", and its roots are French or late Latin. Whereas according to some opinions, "renal" and "nephro" should be replaced with "kidney" in scientific writings such as "kidney medicine" or "kidney replacement therapy", other experts have advocated preserving the use of renal and nephro as appropriate including in "nephrology" and "renal replacement therapy", respectively.

Transplant rejection occurs when transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between donor and recipient and by use of immunosuppressant drugs after transplant.

Henoch–Schönlein purpura (HSP), also known as IgA vasculitis, is a disease of the skin, mucous membranes, and sometimes other organs that most commonly affects children. In the skin, the disease causes palpable purpura, often with joint pain and abdominal pain. With kidney involvement, there may be a loss of small amounts of blood and protein in the urine, but this usually goes unnoticed; in a small proportion of cases, the kidney involvement proceeds to chronic kidney disease. HSP is often preceded by an infection, such as a throat infection.
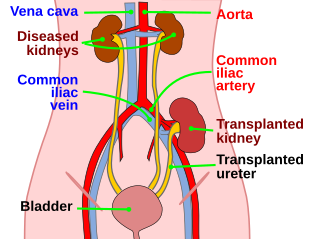
Kidney transplant or renal transplant is the organ transplant of a kidney into a patient with end-stage kidney disease (ESRD). Kidney transplant is typically classified as deceased-donor or living-donor transplantation depending on the source of the donor organ. Living-donor kidney transplants are further characterized as genetically related (living-related) or non-related (living-unrelated) transplants, depending on whether a biological relationship exists between the donor and recipient. The first successful kidney transplant was performed in 1954 by a team including Joseph Murray, the recipient's surgeon, and Hartwell Harrison, surgeon for the donor. Murray was awarded a Nobel Prize in Physiology or Medicine in 1990 for this and other work. In 2018, an estimated 95,479 kidney transplants were performed worldwide, 36% of which came from living donors.
Acute tubular necrosis (ATN) is a medical condition involving the death of tubular epithelial cells that form the renal tubules of the kidneys. Because necrosis is often not present, the term acute tubular injury (ATI) is preferred by pathologists over the older name acute tubular necrosis (ATN). ATN presents with acute kidney injury (AKI) and is one of the most common causes of AKI. Common causes of ATN include low blood pressure and use of nephrotoxic drugs. The presence of "muddy brown casts" of epithelial cells found in the urine during urinalysis is pathognomonic for ATN. Management relies on aggressive treatment of the factors that precipitated ATN. Because the tubular cells continually replace themselves, the overall prognosis for ATN is quite good if the underlying cause is corrected, and recovery is likely within 7 to 21 days.

Decoy cells are virally infected epithelial cells that can be found in the urine. Decoy cells owe their name to their strong resemblance to cancer cells, and may as such confuse the diagnosis of either viral infection or urothelial malignancy. During 1950s, cytotechnologist Andrew Ricci observed cells mimicking cancer cells by they were not, in a group of persons working in some kinds of industries - they were referred to as “decoy cells”, analogous to “decoy ducks” used in hunting wild ducks, by Andrew Ricci, a cytotechnologist working renown cytopathologist Dr. Leopold G. Koss.
Dr. Paul R. Billings is a distinguished American doctor, lecturer, researcher, professor, and consultant on genetic information. His research interests include the impact of genomic data on society, the integration of genomics with diagnostics in health and medical care, and individualised genomic medicine. He is the author of over 250 publications and has appeared on talk shows such as The Oprah Winfrey Show and 60 Minutes. He is currently the CEO and Director of Biological Dynamics.

Metanephric adenoma (MA) is a rare, benign tumour of the kidney, that can have a microscopic appearance similar to a nephroblastoma, or a papillary renal cell carcinoma.

Renal biopsy is a medical procedure in which a small piece of kidney is removed from the body for examination, usually under a microscope. Microscopic examination of the tissue can provide information needed to diagnose, monitor or treat problems of the kidney.

Chronic allograft nephropathy (CAN) is a kidney disorder which is the leading cause of kidney transplant failure, occurring months to years after the transplant.

Transplant glomerulopathy(TG) is a morphologic lesion of renal allografts that is histologically identified by glomerular basement membrane (GBM) duplication and/or multilayering. Proteinuria, hypertension, and deteriorating graft function are the hallmarks of TG.
The Banff Foundation for Allograft Pathology also known as the Banff Foundation for Transplant Pathology is a nonprofit Swiss foundation which aims to "lead development and dissemination of the international Banff Classification of Allograft Pathology and to facilitate multidisciplinary, collaborative research to enhance its scientific basis and clinical utility to improve the care of transplant patients". Its predecessor group had organized transplant pathology meetings in every odd numbered year since 1991 and the Foundation has specific future meeting plans through 2025. The meetings establish and maintain the worldwide standards for tissue biopsy reporting and diagnosis of transplant rejection through consensus decision making. They thereby provide an essential service to the field of allotransplantation. The goals of the Banff foundation are to facilitate knowledge generation and translation in transplantation pathology with the ultimate aim of improving patient outcomes, maintaining the Banff meeting spirit of a multinational, multidisciplinary consensus group, raising funds for research and education in transplantation pathology, providing guidance and financial support for Working Group activities and Banff meetings activities. Kim Solez is the Chair of the Banff Foundation for Allograft Pathology. The 2015 Banff Conference for Allograft Pathology was held in conjunction with the Canadian Society of Transplantation in Vancouver, BC, and included consideration of molecular pathology and tissue engineering pathology as well as traditional light microscopy, immunofluorescence, and electron microscopy. The 2017 Banff Conference was held in Barcelona, Spain. The 2019 Banff Conference was held in Pittsburgh, Pennsylvania, and the 2021 Banff Conference will be in Banff, Alberta, Canada.

Kim Solez is an American pathologist and co-founder of the Banff Classification, the first standardized international classification for renal allograft biopsies. He is also the founder of the Banff Foundation for Allograft Pathology.

Margaret E. Billingham was a pathologist at Stanford University Medical Center, who made significant achievements in the early recognition and grading of transplant rejection following cardiac transplantation, known as 'Billingham's Criteria'. She also described chronic rejection and techniques in heart endomyocardial biopsy.
Bleselumab is a human monoclonal antibody designed for the prevention of organ transplant rejection.
Alexandre Loupy is a French nephrologist, a university professor and hospital practitioner at the Necker Hospital of the Assistance Publique - Hôpitaux de Paris, in the kidney transplant department. He is known for his discoveries on the topic of graft rejection.,, Its approach proposing innovative methodological tools has led to a better understanding but has also led to important changes in the international classification of graft rejection., These discoveries allow to improve the performance of clinical trials and to consider new therapeutic innovations in transplantation.
Javed Iqbal Kazi was a Pakistani pathologist specialized in renal pathology, professor and chairman of Histopathology at Karachi Medical and Dental College, Sindh Institute of Urology & Transplantation, Dr. Ziauddin Hospitals & National Institute of Blood Diseases, and served as Dean of medicine of University of Karachi. He was also the board member of Journal of Pakistan Medical Association since 2005. He established the department of Histopathology at Sindh Institute of Urology & Transplantation, Karachi, in 1995 and is the pioneer of Renal and Transplant Pathology in Pakistan.
Gaetano Ciancio is an Italian American surgeon at the University of Miami who specializes in kidney transplant. He is the chief medical and academic officer of the Miami Transplant Institute and the director of its Kidney & Kidney-Pancreas Programs. His most significant contributions to medicine are related to surgically treating kidney cancer once it has spread to the inferior vena cava and in optimizing the immunosuppression protocol after kidney transplant.
Agnes B. Fogo is a professor of renal pathology at the Vanderbilt University Medical Center.

J. Charles Jennette is a physician, nephropathologist, academic, and author. He served as Kenneth M. Brinkhous Distinguished Professor and Chair of Pathology and Laboratory Medicine at the University of North Carolina at Chapel Hill School of Medicine, and Chief of Pathology and Laboratory Medicine Services at UNC Hospitals from 1999 to 2019.
References
- ↑ Stephanie Pappas (22 July 2009). "Margaret Billingham, Pioneer in Heart Transplant Pathology Dies at 78". Stanford Medicine News Center.
- ↑ Solez, K.; Axelsen, RA; et al. (1993). "International standardization of criteria for the histologic diagnosis of renal allograft rejection: the Banff working classification of kidney transplant pathology". Kidney International. 44 (2): 411–22. doi: 10.1038/ki.1993.259 . PMID 8377384.
- ↑ Bhowmik, D.M.; Dinda, A.K.; et al. (2010). "The evolution of the Banff classification schema for diagnosing renal allograft rejection and its implications for clinicians". Indian Journal of Nephrology. 20 (1): 2–8. doi: 10.4103/0971-4065.62086 . PMC 2878403 . PMID 20535263.
- ↑ Mueller A, et al. (2000). "Impact of the Banff '97 classification for histological diagnosis of rejection on clinical outcome and renal function parameters after kidney transplantation". Transplantation. 69 (6): 1123–7. doi: 10.1097/00007890-200003270-00017 . PMID 10762217.
- ↑ Roufosse, Candice; Simmonds, Naomi; Clahsen-van Groningen, Marian; Haas, Mark; Henriksen, Kammi J.; Horsfield, Catherine; Loupy, Alexandre; Mengel, Michael; Perkowska-Ptasińska, Agnieszka; Rabant, Marion; Racusen, Lorraine C.; Solez, Kim; Becker, Jan U. (November 2018). "A 2018 Reference Guide to the Banff Classification of Renal Allograft Pathology". Transplantation. 102 (11): 1795–1814. doi: 10.1097/TP.0000000000002366 . PMC 7597974 . PMID 30028786. S2CID 51704933.