Related Research Articles
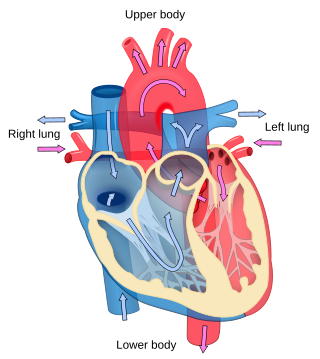
Cardiology is the study of the heart. Cardiology is a branch of medicine that deals with disorders of the heart and the cardiovascular system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease, and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a sub-specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.

Cardiac arrest is when the heart suddenly and unexpectedly stops beating. When the heart stops beating, blood cannot properly circulate around the body and the blood flow to the brain and other organs is decreased. When the brain does not receive enough blood, this can cause a person to lose consciousness and brain cells can start to die due to lack of oxygen. Coma and persistent vegetative state may result from cardiac arrest. Cardiac arrest is also identified by a lack of central pulses and abnormal or absent breathing.

A pacemaker, also known as an artificial cardiac pacemaker, is an implanted medical device that generates electrical pulses delivered by electrodes to one or more of the chambers of the heart. Each pulse causes the targeted chamber(s) to contract and pump blood, thus regulating the function of the electrical conduction system of the heart.

Defibrillation is a treatment for life-threatening cardiac arrhythmias, specifically ventricular fibrillation (V-Fib) and non-perfusing ventricular tachycardia (V-Tach). A defibrillator delivers a dose of electric current to the heart. Although not fully understood, this process depolarizes a large amount of the heart muscle, ending the arrhythmia. Subsequently, the body's natural pacemaker in the sinoatrial node of the heart is able to re-establish normal sinus rhythm. A heart which is in asystole (flatline) cannot be restarted by a defibrillator; it would be treated only by cardiopulmonary resuscitation (CPR) and medication, and then by cardioversion or defibrillation if it converts into a shockable rhythm.

Brugada syndrome (BrS) is a genetic disorder in which the electrical activity of the heart is abnormal due to channelopathy. It increases the risk of abnormal heart rhythms and sudden cardiac death. Those affected may have episodes of syncope. The abnormal heart rhythms seen in those with Brugada syndrome often occur at rest. They may be triggered by a fever.
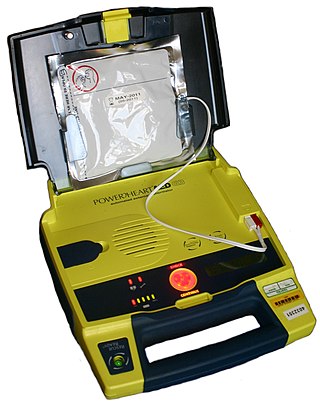
An automated external defibrillator or automatic electronic defibrillator (AED) is a portable electronic device that automatically diagnoses the life-threatening cardiac arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able to treat them through defibrillation, the application of electricity which stops the arrhythmia, allowing the heart to re-establish an effective rhythm.

An implantable cardioverter-defibrillator (ICD) or automated implantable cardioverter defibrillator (AICD) is a device implantable inside the body, able to perform defibrillation, and depending on the type, cardioversion and pacing of the heart. The ICD is the first-line treatment and prophylactic therapy for patients at risk for sudden cardiac death due to ventricular fibrillation and ventricular tachycardia.

Short QT syndrome (SQT) is a very rare genetic disease of the electrical system of the heart, and is associated with an increased risk of abnormal heart rhythms and sudden cardiac death. The syndrome gets its name from a characteristic feature seen on an electrocardiogram (ECG) – a shortening of the QT interval. It is caused by mutations in genes encoding ion channels that shorten the cardiac action potential, and appears to be inherited in an autosomal dominant pattern. The condition is diagnosed using a 12-lead ECG. Short QT syndrome can be treated using an implantable cardioverter-defibrillator or medications including quinidine. Short QT syndrome was first described in 2000, and the first genetic mutation associated with the condition was identified in 2004.
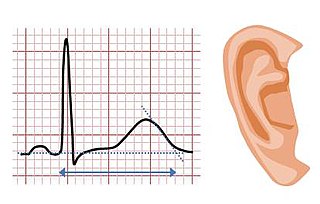
Jervell and Lange-Nielsen syndrome (JLNS) is a rare type of long QT syndrome associated with severe, bilateral sensorineural hearing loss. Those with JLNS are at risk of abnormal heart rhythms called arrhythmias, which can lead to fainting, seizures, or sudden death. JLNS, like other forms of long QT syndrome, causes the cardiac muscle to take longer than usual to recharge between beats. It is caused by genetic variants responsible for producing ion channels that carry transport potassium out of cells. The condition is usually diagnosed using an electrocardiogram, but genetic testing can also be used. Treatment includes lifestyle measures, beta blockers, and implantation of a defibrillator in some cases. It was first described by Anton Jervell and Fred Lange-Nielsen in 1957.

Cardiac resynchronisation therapy is the insertion of electrodes in the left and right ventricles of the heart, as well as on occasion the right atrium, to treat heart failure by coordinating the function of the left and right ventricles via a pacemaker, a small device inserted into the anterior chest wall.
A wearable cardioverter defibrillator (WCD) is a non-invasive, external device for patients at risk of sudden cardiac arrest (SCA). It allows physicians time to assess their patient's arrhythmic risk and see if their ejection fraction improves before determining the next steps in patient care. It is a leased device. A summary of the device, its technology and indications was published in 2017 and reviewed by the EHRA Scientific Documents Committee.

Arrhythmias, also known as cardiac arrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a resting heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath, chest pain, or decreased level of consciousness. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.
Cardiac contractility modulation is a therapy which is intended for the treatment of patients with moderate to severe heart failure with symptoms despite optimal medical therapy who can benefit from an improvement in cardiac output. The short- and long-term use of this therapy enhances the strength of ventricular contraction and therefore the heart's pumping capacity by modulating (adjusting) the myocardial contractility. This is provided by a pacemaker-like device that applies non-excitatory electrical signals adjusted to and synchronized with the electrical action in the cardiac cycle.
Frank I. Marcus was an American cardiologist and Emeritus Professor of Medicine at the University of Arizona Health Sciences Center, the author of more than 290 publications in peer-reviewed medical journals and of 90 book chapters. He was considered a world expert on arrhythmogenic right ventricular cardiomyopathy (ARVC) and was a member of the Editorial/Scientific Board of 14 Cardiovascular Journals as well as a reviewer for 26 other medical publications.

Yaariv Khaykin is a Canadian cardiologist and a clinical researcher in the area of electrophysiology. He is the director of the Newmarket Electrophysiology Research Group at the Southlake Regional Health Centre. He has published research into complex ablation and pioneered cardiac ablation methods.

Subcutaneous implantable cardioverter defibrillator, or S-ICD, is an implantable medical device for detecting and terminating ventricular tachycardia and ventricular fibrillation in patients at risk of sudden cardiac arrest. It is a type of implantable cardioverter defibrillator but unlike the transvenous ICD, the S-ICD lead is placed just under the skin, leaving the heart and veins untouched.
Tarlochan Singh Kler is an Indian interventional cardiologist, medical administrator, writer, Chairman at Fortis Heart and Vascular Institute, and. Born in Amargarh in the Indian state of Punjab, he graduated in medicine from Punjabi University in 1976, secured his MD in general medicine from Postgraduate Institute of Medical Education and Research (PGIMER) in 1980 and followed it up with the degree of DM in cardiology from the same institution in 1983. He succeeded Naresh Trehan as the executive director of Fortis Heart Institute and Research Centre before becoming its director. He has written several articles on interventional cardiology; Persistent left superior vena cava opening directly into right atrium and mistaken for coronary sinus during biventricular pacemaker implantation, Mammary coronary artery anastomosis without cardiopulmonary bypass through minithoracotomy: one year clinical experience, and Ventricular Fibrillation in the EP Lab. What is the Atrial Rhythm? are some of the notable ones. The Government of India awarded him the third highest civilian honour of the Padma Bhushan, in 2005, for his contributions to medicine.
Iqbal Mahmoud Al Assad is a physician pursuing a pediatric cardiology fellowship at Boston Children's Hospital. She was recognized as one of the youngest doctors in the world when she completed her medical training at age 20. Her name is also seen as Iqbal El-Assaad in some sources.
References
- ↑ "Barouh Berkovits Obituary: View Obituary for Barouh Berkovits by Levine Chapels, Brookline, MA". Obits.dignitymemorial.com. 1926-05-07. Archived from the original on 2015-06-10. Retrieved 2012-10-26.
- ↑ "Biography of Barouh V. Berkovits". Author.hrsonline.org. Retrieved 2012-10-26.[ permanent dead link ]
- ↑ Kirk Jeffrey (2001). Machines in Our Hearts: The Cardiac Pacemaker, the Implantable Defibrillator, and American Health Care. The Johns Hopkins University Press.
- ↑ Cakulev, I; Efimov, I. R.; Waldo, A. L. (2009). "Cardioversion: Past, Present, and Future". Circulation. 120 (16): 1623–1632. doi:10.1161/CIRCULATIONAHA.109.865535. PMC 2782563 . PMID 19841308.
- ↑ Levy, Samuel; Medina-Ravell, Victor A.; Castellanos Jr, Agustin (2013). "Barouh V. Berkovits, MSEE (1926–2012)". Heart Rhythm. 10 (3): 411. doi:10.1016/j.hrthm.2013.01.010. ISSN 1547-5271.
- ↑ "Archived copy" (PDF). Archived from the original (PDF) on 2016-06-23. Retrieved 2015-09-06.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ "Barouh V. Berkovits, MSEE (1926–2012)". Heart Rhythm. 10 (3): 411. 1 March 2013. doi:10.1016/j.hrthm.2013.01.010.